TITLE 28. Managed Health Care
Division 1. The Department of Managed Health Care
Chapter 1. Department Administration
Article 1. Conflict of Interest
§1000. Conflict of Interest Code for the Department of Managed Health Care.
Note • History
The Political Reform Act, Government Code Section 81000, et. seq., requires state and local government agencies to adopt and promulgate conflict of interest codes. The Fair Political Practices Commission has adopted a regulation (Title 2, California Code of Regulations (CCR), section 18730) which contains the terms of a standard conflict of interest code, which can be incorporated by reference in an agency's code. After public notice and hearing it may be amended by the Fair Political Practices Commission to conform to amendments in the Political Reform Act. Therefore, the terms of 2 CCR, section 18730, and any amendments to it duly adopted by the Fair Political Practices Commission are hereby incorporated by reference. This regulation, and the attached Appendix designating officials and employees and establishing disclosure categories, shall constitute the conflict of interest code of the Department of Managed Health Care.
Designated employees shall file statements of economic interests with the Office of Administration of the Department of Managed Health Care, which will make the statements available for public inspection and reproduction. (Government Code, Section 81008). Upon receipt of the statement of the Director of the Department of Managed Health Care, the Office of Administration shall make and retain a copy and forward the original to the Fair Political Practices Commission. Statements for all other designated employees will be retained by the Office of Administration of the Department of Managed Health Care.
NOTE
Authority cited: Section 1344, Health and Safety Code; Section 87300, Government Code. Reference: Sections 87300-87302 and 87306, Government Code (the Political Reform Act).
HISTORY
1. New chapter 1, article 1 (section 1000), section and appendix filed 12-12-2001, including editorial renumbering of former chapter 1 to chapter 2; operative 1-11-2002. Approved by Fair Political Practices Commission 10-3-2001 (Register 2001, No. 50).
2. Amendment of division heading filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
3. Change without regulatory effect amending chapter 1 heading, section and appendix disclosure category C(1)-(2) filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
4. Amendment of Appendix filed 7-21-2003; operative 8-20-2003. Approved by Fair Political Practices Commission 5-12-2003 (Register 2003, No. 30).
5. Change without regulatory effect amending first paragraph filed 2-24-2004 pursuant to section 100, title 1, California Code of Regulations (Register 2004, No. 9).
6. Amendment of Appendix filed 2-3-2005; operative 3-5-2005. Approved by Fair Political Practices Commission 12-3-2004 (Register 2005, No. 5).
Appendix
Assigned
Designated Positions Disclosure Categories
Director, Department of Managed Health Care A, B
Chief Deputy Director A, B
Deputy Director, Communications and Planning A, B
Deputy Director, External Affairs A, B
Medical Advisor to Directors Office A, B
Deputy Director, Plan & Provider Relations A, B
Deputy Director Financial Solvency Standards Board A, B
All Counsel, supervisory or nonsupervisory, regardless of level,
wherever assigned A, B
All Health Analysts, supervisory or nonsupervisory, regardless of level,
wherever assigned A, B
All Examiners, supervisory or nonsupervisory, regardless of level,
wherever assigned A, B
Chief, HMO Help Center A, B
Assistant Deputy Director, Office of Health Plan Oversight A, B
Assistant Deputy Director, Office of Legal Services A, B
Assistant Deputy Director, HMO Help Center A, B
Assistant Deputy Director, Office of Technology and Innovation A, B
Assistant Deputy Director, Office of Enforcement A, B
Assistant Deputy Director, Office of Administration A, B
Auditor A, B
Chief, Division of Financial Oversight A, B
Chief, Division of Plan Surveys A, B
Nurses, wherever assigned B
Consultants used by the Office of Technology and Innovation B, C
Chief, Accounting Section B, C
Chief, Business Management Section B, C
Supervisor, Application Support Section B, C
Supervisor, Support Services Section B, C
Application Architect B, C
Lead Systems Engineer B, C
Other Consultants* A*
_______________
*Consultants shall disclose pursuant to the broadest disclosure category in the code (Category A) subject to the following limitations:
The Director of the Department of Managed Health Care may determine in writing that a particular consultant, although a “designated position,” is hired to perform a range of duties that is limited in scope and thus is not required to fully comply with the disclosure requirements in this section. Such written determination shall include a description of the consultant's duties and, based upon that description, a statement of the extent of disclosure requirements. The Director's determination is a public record and shall be retained for public inspection in the same manner and location as this conflict of interest code. Nothing herein excuses any such consultant from any other provisions of this Conflict of Interest Code.
_______________
Disclosure Categories
Category A
Each “designated employee” in this category shall report:
(1) Income from any source, investments in any business entity, or business positions in any entity which has “transacted business” with the Department or has been the “subject of any legislation or rulemaking activity” during the previous two years or which the employee has reason to know is planning to transact business with the Department or be subject of any legislation or rulemaking activity.
(2) Any real property which during the preceding two years was rented, leased, or sold to a business entity, or leased or purchased from a business entity, which has transacted business with the Department or been the subject of any legislation or rulemaking activity during the preceding two years or which the designated employee knows or has reason to know is planning to transact business with the Department or be the subject of any legislation or rulemaking activity.
(3) For purposes of this category, “transacting business with the Department” includes, but is not limited to, any activity or contact with the Department in connection with a permit, order, registration, license, certificate, opinion, complaint known to or directly involving the employee, or enforcement action known to or directly involving the employee. A business entity has been or will be “the subject of any legislation or rulemaking activity” if the business entity is, was, will be, or would have been directly affected by any legislation or rule in connection with the laws over which the Department Director has jurisdiction, whether or not such legislation or rule was enacted, adopted, amended, or repealed.
Category B
Each “designated employee” in this category shall report:
(1)(a) Income from any source, investments in any business entity, or business positions in any business entity which is subject to, or which the designated employee knows or has reason to know may be subject to, or by rule of the Director exempted from, the provisions of the Knox-Keene Health Care Service Plan Act of 1975.
(b) Income from any source, investments in any business entity, or business positions in any business entity which provides medical services, including but not limited to, privately owned hospitals, medical clinics, laboratories, pharmacies, and ambulance companies.
(c) Income from any source, investments in any business entity, or business positions in any business entity which provides training or education for persons engaged in medical service activities or programs.
(2) Real property which during the preceding two years was rented, leased or sold to a business entity, or leased, or purchased from a business entity, which is subject to, or which he or she knows or has reason to know may be subject to, or by rule of the Director exempted from the provisions of the Knox-Keene Health Care Service Plan Act of 1975.
Category C
Each “designated employee” in this category shall report:
(1) Income from any source, investments in any business entity, or business positions in any business entity which is, of the type that, during the preceding two years provided the Department of Managed Health Care or its immediate predecessor agency (the Department of Corporations) with services, supplies, materials, machines, equipment or office space.
(2) Real property which during the preceding two years has been rented, leased or sold to a business entity or leased or purchased from a business entity, which is of the type which during the preceding two years has provided, the Department of Managed Health Care or its predecessor agencies (i.e., the Department of Corporations) with services, supplies, materials, machines, or office space.
Article 2. Administration
§1001. Department Internet Web Page and Web Addresses.
Note • History
The Department shall maintain an internet web page containing information about the Department, its functions and activities. The internet web page may be accessed to obtain departmental forms, notices, and other publications. The internet web page shall be accessible by either of two web addresses: http://www.dmhc.ca.gov, or http://www.hmohelp.ca.gov.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1344, Health and Safety Code.
HISTORY
1. New article 2 (sections 1001-1008) and section filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
§1002. Appearance and Practice Before the Department.
Note • History
A person may be represented by an attorney at law in any proceeding before the Director or Department, provided the attorney is admitted to practice before the highest court of any state or territory of the United States, or the Court of Appeals or the District Court of the United States for the District of Columbia. Alternatively, a person may appear before the Director or Department on his or her own behalf; a member of a partnership may represent the partnership; and an authorized officer of a corporation, trust or association may represent that corporation, trust or association.
NOTE
Authority cited: Sections 1344 and 1346, Health and Safety Code. Reference: Sections 1341, 1342, 1348-1349, 1370, 1386-1388 and 1390-1393, Health and Safety Code.
HISTORY
1. New section filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
§1002.4. Public Meetings and Hearings.
Note • History
(a) A public meeting or hearing may be held pursuant to Health and Safety Code section 1346(a)(5) at the discretion of the Director for the following types of proceedings:
(1) Investigation or analysis of matters affecting the interests of plans, subscribers, enrollees, or the public.
(2) Educational programs for the public, subscribers, enrollees, and licensees.
(3) An amendment, material modification or other plan filing that proposes:
(A) Any change that may have a significant impact, as determined by the Director, on the ability of enrollees to access health care services; or
(B) Any change that may have a material effect, as determined by the Director, on the health care service plan (plan) or on its operations.
(b) Factors that may be considered by the Director in determining whether to hold a public meeting or hearing include:
(1) Whether the proposal has a significant impact on plans, providers, subscribers, enrollees, or Californians generally, including the nature, scope, and significance of any such impact;
(2) Whether a public meeting or hearing would help to assure identification of all relevant issues raised in the proposal, and/or ongoing monitoring of the plan, and inform their resolution;
(3) Whether a public meeting or hearing would provide additional facts or opinions relevant to a decision whether to approve the filing, including any conditions or undertakings to impose on the approval;
(4) Whether a public meeting or hearing would provide a greater depth or scope of understanding of the potential short-term and long-term results or ramifications of an approval, with or without conditions;
(5) Whether the likely costs to the Department outweigh the potential benefit; and
(6) Whether there is sufficient time to hold a meeting or hearing.
(c) Requests for Public Meeting or Hearing.
(1) Any person may request a public meeting or hearing by filing a written request with the Department.
(2) A request for public meeting or hearing shall:
(A) Be in writing addressed to the Director, in care of the Office of Legal Services, Department of Managed Health Care, 980 Ninth Street, Suite 500, Sacramento, CA 95814, or by e-mail addressed to publichearing@dmhc.ca.gov; and
(B) Clearly state that it is a request for a public meeting or hearing and state the matter upon which the public meeting or hearing is requested, including the relevant facts and/or circumstances upon which the request is made; and
(C) Identify the persons or entities on whose behalf the request is made and specify the address to which the Director's determination pursuant to subsection (c)(3) may be mailed or e-mailed.
(3) The Director will determine whether the request for a meeting or hearing warrants a public meeting or hearing.
(4) The Director will notify the person requesting a meeting or hearing of the determination within ten business days of the date the request is submitted.
NOTE
Authority cited: Sections 1342, 1344 and 1346, Health and Safety Code. Reference: Section 1346(a)(5), Health and Safety Code.
HISTORY
1. New section filed 9-11-2006; operative 10-11-2006 (Register 2006, No. 37).
§1003. Public Comment During Department Meetings.
Note • History
At all Department committee, panel or board meetings that are subject to the Bagley-Keene Open Meeting Act (Government Code § 11120 et seq.), members of the public will be permitted to address the committee, panel or board prior to the committee, panel or board making any decision. Public comments will be heard in the order in which speakers sign up; limited to only agenda items; and may be no longer than five minutes in length unless otherwise permitted.
NOTE
Authority cited: Sections 1344 and 1346, Health and Safety Code; and Section 11125.7, Government Code. Reference: Sections 1347, 1347.1 and 1347.15, Health and Safety Code.
HISTORY
1. New section filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
Note • History
(a) Whenever a statute, regulation or the Director requires that a document filed with the Department be verified, the verification shall be by declaration under penalty of perjury pursuant to Code of Civil Procedure section 2015.5.
(b) “Declaration” means a certification in substantially the following form:
(1) I declare under penalty of perjury under the laws of the State of California that the foregoing is true and correct.
Executed at ________________________________________________________
(Location)
______ :_____________________ ______________________________________
(Date) (Signature) (Typed or printed name)
NOTE
Authority cited: Sections 1344 and 1346, Health and Safety Code. Reference: Sections 2012-2015.5, Code of Civil Procedure.
HISTORY
1. New section filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
Note • History
(a) The Director in his or her discretion may honor requests from interested person(s) for written interpretive opinions regarding any provision of, or regulation promulgated pursuant to, the Act.
(b) An interpretive opinion request shall satisfy each of the following conditions:
(1) The request shall be in writing addressed to the Director in care of the Office of Legal Services at the Sacramento Office of the Department or by e-mail at interpretiveopinion@dmhc.ca.gov. The request shall clearly state that it is a request for an interpretive opinion and set forth the question(s) presented, including the relevant facts and/or circumstances upon which the request is made.
(2) The persons or entities on whose behalf the request is made shall be identified and all documents relevant to the request shall be appended to the request.
(c) Each interpretive opinion is applicable only to the matter identified in the specific written request for which the interpretive opinion was prepared. The interpretive opinion may not be relied upon in connection with any other matter.
(d) Attorneys seeking interpretive opinions on behalf of clients shall include with the opinion requests their own analyses of the issues presented by the request, their views with respect to the issues presented and citations of legal authority in support of those views.
(e) The Department shall maintain an index of the person(s) on whose behalf an interpretive opinion was prepared, and the nature of the request.
(f) The Director may select interpretive opinions for publication. Published opinions will be available on the Department's web page. The decision to publish an interpretive opinion will be made solely by the Director with regard to the public interest and the legal question(s) considered. The Director may rescind any published opinion and shall notify the party for whom the opinion was prepared of the rescission. Rescission of a published opinion shall be indicated on the Department's website.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1344, Health and Safety Code.
HISTORY
1. New section filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
2. Amendment of subsection (a), new subsections (b)-(d), subsection relettering and amendment of newly designated subsection (f) filed 10-27-2003; operative 11-26-2003 (Register 2003, No. 44).
3. Change without regulatory effect amending subsection (b)(1) filed 5-5-2004 pursuant to section 100, title 1, California Code of Regulations (Register 2004, No. 19).
4. Change without regulatory effect amending subsection (b)(1) filed 9-9-2004 pursuant to section 100, title 1, California Code of Regulations (Register 2004, No. 37).
§1006. Inspection of Public Records.
Note • History
(a) Public access to records maintained by the Department is governed by the California Public Records Act (Government Code § 6250 et. seq.). The term “public record,” as used in this section, is defined in Government Code section 6252(e). Public records are available for inspection and/or copying pursuant to the following procedures:
(1) Requests for the inspection and/or copying of public records must be sufficiently descriptive to enable Department personnel to identify, locate, and retrieve the records.
(2) Requests must be in writing and sent to the Department's mailing address at Department of Managed Health Care, 980 9th Street, Suite 500, Sacramento, CA 95814, Attention: Office of Legal Services. A properly addressed request will ensure prompt response by the Department.
(3) Retrieval and inspection of any record shall not interfere with the ordinary business operations of the Department. Operational functions of the Department will not be suspended to permit inspection of records where the records are reasonably required by Department personnel in the performance of their duties. If the request requires reviewing numerous records, a mutually agreeable time will be established for the inspection of the records. All inspections will occur during regular business hours of the Department.
(4) Physical inspection of records is permitted in Department offices. Upon completion of the inspection, the person conducting the inspection shall relinquish possession of the records. Persons inspecting Department records shall not destroy, mutilate, deface, alter, or remove any such records from the Department. The Department reserves the right to have Departmental personnel present during the inspection of records in order to prevent the loss or destruction of records.
(b) The Department may refuse to disclose records that are exempt from disclosure under the Public Records Act. (See e.g, Gov. Code, §6254.)
(c) Requests for copies of public records will be conducted pursuant to the following procedures:
(1) The Department shall charge the person requesting copies of public records made by Department personnel at the rate of thirty cents ($0.30) per page. Payment of the total estimated copy charge shall be required before Department personnel copy any records. The Department may waive copying costs when the total copying cost for records requested is less than ten dollars ($10.00) per year.
(2) If the number of records requiring copying is determined to be voluminous by Department personnel, then the Department may require the person requesting the records to supply or hire his/her own copy service to photocopy the records. The cost associated with providing the copy service shall be borne entirely by the requesting person.
(3) Persons requesting copies of transcripts from Department committees, panels or boards shall be charged a flat fee of $30.00 per transcript regardless of page length. Tape-recorded cassette transcripts of Department committees, panels or board meetings shall be charged a flat fee of $5.00 per proceeding.
NOTE
Authority cited: Section 6253.4, Government Code; and Section 1344, Health and Safety Code. References: Section 6250, 6253, 6254 and 6255, Government Code.
HISTORY
1. New section filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
§1007. Request for Confidentiality.
Note • History
(a) The Director will withhold from public inspection, pursuant to the applicable state and/or federal law, information received in connection with an application (including applications for interpretive opinions) or report, if in the opinion of the Director, the public inspection of such information is not necessary for the purposes of the law under which the information was filed, and the information is reasonably shown to meet either of the following:
(1) The information is proprietary or of a confidential business nature, including but not limited to trade secrets, and has been confidentially maintained by the business entity and the release of which would be damaging or prejudicial to the business concern.
(2) The information is such that the private and/or public interest is served in withholding the information.
(b) Requests for Confidential treatment. A request for confidential treatment of any information received in connection with an application or report submitted to the Department must be filed with the information submitted. The information intended to remain confidential must be filed separately from the remaining parts of the application or report and marked “Confidential Treatment Requested.” The person filing the application or report and requesting confidential treatment must sign the request. The signed request must contain the following:
(1) A statement identifying the information that is the subject of the request and the application or report relating thereto.
(2) A statement specifying the provisions of subsection (a) pursuant to which the request is made.
(3) A statement of the grounds upon which the request is made, including (if applicable) a statement as to the information's confidentiality and the measures taken to protect its confidentiality, and a statement of the adverse consequences that are expected to result if the information is disclosed through the public records of the Department.
(4) A statement of the specific time for which confidential treatment of the information is necessary, and the basis for such conclusion.
(5) If appropriate, a statement of the extent to which such information has been, or will be, disclosed to present or proposed investors, or other persons appropriate under the statute pursuant to which the information is filed.
(c) Request for Confidentiality Available for Public Inspection. Requests for confidentiality will be available for public inspection. Therefore, the request for confidentiality should not contain information that is itself confidential.
(d) Granting of Request. If a request for confidential treatment is granted, the person making such request will be notified in writing, the information will be marked “confidential” and kept separate from the public file, and the application or report will be noted with the following legend: “Additional portions of this filing have been granted confidential treatment pursuant to Section 1007 of Title 28, Chapter 1, of the California Code of Regulations. They are contained in a separate confidential file.”
(e) Denial of Request. Material for which confidential treatment is requested shall not be deemed filed unless the request is granted, and may be withdrawn by the applicant if the request is denied, unless (1) the Director has already taken an official action in reliance on such information prior to receiving the request for confidential treatment; or (2) the Director determines that the withdrawal of such information is otherwise contrary to the public interest. If withdrawn, such information will not be considered by the Director in connection with the application or report.
(f) Permissible Disclosure of Information Held Confidential. Information held confidential pursuant to this section may be disclosed by the Director, at any time and in the Director's sole discretion, whether on the Director's own motion or upon the request of any person, under the following circumstances:
(1) To other local, state, or federal regulatory or law-enforcement agencies, in accordance with the law;
(2) When necessary or appropriate in any proceeding or investigation pursuant to the law under which the information was filed;
(3) Upon a determination by the Director that the private and/or public interest in disclosing such information outweighs the public interest in non-disclosure; or
(4) Upon a determination by the Director that the justifications for the confidential treatment no longer exist.
(5) If the Director determines to disclose confidentially held information pursuant to subsections (f)(1) through (f)(4), and concludes that the disclosure of such information is necessary and urgent, or that it is impractical under the circumstances to give notice to the person who requested confidential treatment of the information, the information may be disclosed without notice. Otherwise, the person who requested confidential treatment of such information shall be given written and actual notice through certified mail that the release of such information is under consideration and the reasons therefor. Thereafter, the person will be given five business days to explain why the need and justification for continued confidentiality exists.
(g) Requests to Inspect Confidential Information. A request to inspect confidential information pursuant to subsections (f)(1) through (f)(4) shall be in writing, state the justification for the request, and be signed by the person making the request. A copy of the request for inspection shall be forwarded to the person who requested confidential treatment of the information in accordance with subsection (f)(5). If a request for inspection should be held confidential and not disclosed to the owner of the confidential information, the reasons therefor must be stated in such request, in accordance with subsection (b).
(h) Nothing contained herein shall be interpreted as affording any person a right to withdraw information once it has been received by the Director, except as provided in subsection (e).
NOTE
Authority cited: Sections 1344 and 1346, Health and Safety Code. References: Sections 6253, 6254 and 6255, Government Code; Section 1040, Evidence Code; and Sections 1344 and 1351, Health and Safety Code.
HISTORY
1. New section filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
§1008. Availability of Department Forms, Publications and Notices; Fees.
Note • History
(a) Department forms required by the Act or regulations, releases, notice of regulatory changes, and other publications are available free of charge on the Department's web page.
(b) Department forms required by the Act or regulations, releases, notice of regulatory changes, and other publications are available at either the Department's Sacramento or Los Angeles office, or via the mail. The Department will charge thirty cents ($0.30) per page for any document picked up at the Department's offices. Documents requested by mail should be directed to the Department of Managed Health Care, 980 9th Street, Suite 500, Sacramento, CA 95814-2724. The fee for any document mailed will be thirty cents ($0.30) per page, plus postage. The minimum charge for any single order by mail will be $5.00. No charges will be incurred for providing a single copy of the Department's consumer complaint form.
NOTE
Authority cited: Sections 1344 and 1346.4, Health and Safety Code. Reference: Sections 1344 and 1346, Health and Safety Code.
HISTORY
1. New section filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
§1009. Retention of Department Records.
Note • History
(a) The Department shall maintain records and files necessary to accomplish the Department's regulatory function according to subdivision (b) and the approved Record Retention Schedule by the Department of General Services. Records and files may be maintained by the Department using either paper, electronic or other alternative storage technologies, including but not limited to, photography, microphotography, electronically recorded video images on magnetic surfaces, electronic data processing systems, optical disk storage, or any other trusted medium that does not permit additions, deletions, or changes to the original document. Unless specifically superseded by another legal obligation, Department records and files shall be destroyed pursuant to the schedule in subsection (b).
(b) Department records and files shall be destroyed as follows:
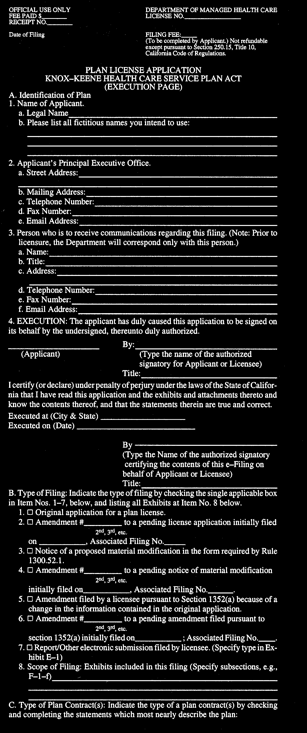
(1) Plan license applications, amendments, and material modifications:
(A) A plan's license, original application and execution pages A through D, as described in section 1300.51, shall be retained by the Department until a plan's license is surrendered or revoked. Records and files pertaining to the plan's license will be maintained by the Department for a minimum of two years following the plan's surrender or revocation of the license. Thereafter, the records and files shall be destroyed.
(B) Exhibits to a plan's license application, as described in section 1300.51 subsections E through FF, amendments, and material modifications shall be retained by the Department for a minimum of five years from the date of filing. Thereafter, the records and files shall be destroyed.
(C) Records and files regarding a plan's financial status and fiscal arrangements, as described in section 1300.51, shall be retained for a minimum of five years from the date of filing. Thereafter, the records and files shall be destroyed.
(2) Correspondence between a plan and Department counsel or staff may be retained by the Department if it is determined that the correspondence is of material value in the continued regulation of the plan. Such correspondence shall be maintained for a minimum of five years. Thereafter, the correspondence shall be destroyed.
(3) Final financial and medical survey plan reports shall be maintained by the Department for a minimum of five years from the date of the final report's release or until release of the next final report, whichever is later. Examiner and surveyor working documents used in preparing the report shall also be maintained for a minimum of five years from the date of the final report's release. Thereafter, the report and all working documents shall be destroyed.
(4) Records and files pertaining to Department enforcement investigations and actions, and Department litigation shall be retained for a minimum of five years from the date the matter is closed. Thereafter, the records and files shall be destroyed.
(5) Records and files pertaining to enrollee and consumer complaints, and the Independent Medical Review process, shall be retained for a minimum of two years from the date the Department closes the matter except any medical x-rays may be destroyed immediately following the closure of the matter. Thereafter, the records and files shall be destroyed. Records and files that are determined to be outside of the Department's jurisdiction pertaining to enrollee and consumer complaints, and the Independent Medical Review process may be destroyed immediately following the closure of the matter.
(c) Notwithstanding this section the Department may retain a record, file, or document at the Director's discretion.
(d) The record retention schedule outlined in subsection (b) shall apply to all records and files maintained by the Department after January 1, 1998. Documents filed with the Department, or its predecessor Department of Corporations before January 1, 1998, may be destroyed at the Director's discretion.
NOTE
Authority cited: Section 14750, Government Code; and Section 1344, Health and Safety Code. Reference: Sections 14741, 14745, 14750, 14755 and 14756, Government Code; and Section 1344, Health and Safety Code.
HISTORY
1. New section filed 10-29-2003; operative 11-28-2003 (Register 2003, No. 44).
§1010. Consumer Participation Program.
Note • History
(a) Intent and Regulatory Purpose.
The purpose of this regulation is to establish the Department's substantive and procedural process and criteria, in accordance with section 1348.9 of the Health & Safety Code for determining discretionary awards, if any, of reasonable advocacy and witness fees to Participants on the basis that the Participant Represent the Interests of Consumers in a Proceeding, and has made Substantial Contribution to the Department in its deliberations. Nothing in this article shall be construed to prohibit any person from participating in a Proceeding if that person does not seek compensation pursuant to this article.
(b) Definitions.
For purposes of this section, the following definitions shall apply:
(1) “Advocacy Fee” means expenses, incurred for in-house advocates or billed, by a Participant for the services of an advocate in the proceeding. An advocate need not be an attorney. Advocacy fees shall not exceed market rates as defined in this section.
(2) “Compensation” means payment for all or part of the amount requested by a Participant for advocacy fees and witness fees in any proceeding relating to the adoption of any regulation or to an order or decision, including a decision not to adopt a regulation, made by the Director.
(3) “Market Rate” means, with respect to advocacy and witness fees, the prevailing rate for comparable services in the private sector in the Los Angeles and San Francisco Bay Areas at the time of the Director's decision awarding compensation to a Participant for attorney advocates, non-attorney advocates, or experts with similar experience, skill and ability. Billing rates shall not exceed the Market Rate.
(4) “Participant” means a person whose Request for Finding of Eligibility to Participate, filed under subsection (c) or Petition to Participate, filed under subsection (d) below, has been granted by the Director.
(5) “Proceeding” or “Administrative Proceeding” mean an administrative decision-making process of the Department of Managed Health Care that results in the adoption of a regulation, or in an order or decision of the Director that has the potential to impact a significant number of enrollees. For purposes of this Article, “order or decision made by the Director” shall include a decision not to adopt a regulation or take an action and shall not include resolution of individual grievances, complaints, or cases.
(6) “Represents the Interests of Consumers” means that the person or organization has a record of advocacy on behalf of health care consumers in administrative or legislative proceedings. A party which represents, in whole or in part, any entity regulated by the Department shall not be eligible for compensation.
(7) “Submit to the Director” means to send material electronically to The Director, at dmhc.ca.gov., or, for entities that do not have access to e-mail, by mail to The Director, Department of Managed Health Care, 980 9th Street, Suite 500, Sacramento, CA 95814.
(8) “Substantial Contribution” means that the Participant significantly assisted the Department in its deliberations by presenting relevant issues, evidence, or arguments which were helpful, and seriously considered, and the Participant's involvement resulted in more relevant, credible, and non-frivolous information being available to the Director.
(9) “Verified” means executing a statement stating that the facts contained in the Request for Finding of Eligibility to receive an award of compensation are true and correct, to the best of their knowledge.
(10) “Witness Fees” means expenses, incurred or billed, by a Participant for the services of an expert witness in the proceeding. Witness fees shall not exceed market rates as defined in this section.
(c) Request for Finding of Eligibility to Participate and Seek Compensation.
(1) A person who intends to seek an award under this article shall submit to the Director a Request for Finding of Eligibility to Participate and Seek Compensation, giving notice that it represents the interests of consumers and of its intent to claim compensation. The request shall be verified, and may be submitted at any time independent of the pendency of a proceeding in which the person seeks to participate.
(2) The request shall contain:
a. The petitioner's name, mailing address, telephone number, and e-mail address, if any.
b. A showing that the petitioner Represents the Interests of Consumers, including a description of its experience in advocating on behalf of health care consumers in administrative or legislative proceedings.
c. For petitioners that are organizations, the following information about the organization:
1. Names, addresses, and titles of the members of the organization's governing body,
2. A description of the organization's general purposes, size, and structure,
3. Whether the organization is a nonprofit organization, and
4. Under what statute the organization is incorporated.
(3) Within 30 days of the receipt of the Request for Finding of Eligibility to Participate, the Director shall rule on the requestor's eligibility to participate and to seek an award of compensation. If the Director finds that the requestor has met the requirements for eligibility, the Director shall grant the request. A finding of eligibility to seek compensation shall be valid in any proceeding in which a Participant's involvement commences within two years of the finding of eligibility so long as the Participant still Represents the Interests of Consumers.
(4) A person found eligible to participate and seek compensation shall promptly disclose to the Department any material changes in the information submitted in its request.
(d) Procedure for Petition to Participate.
(1) Periodically, the Director may identify regulatory proceedings in which he or she believes consumer participation would be helpful and anticipates that fees may be awarded. Nothing in this subsection shall be construed as limiting compensation only to those proceedings on the Director's list, if any. A person desiring to participate in a proceeding and seek an award of fees under this subsection shall submit electronically to the Director a Petition to Participate, as described in this subdivision. The request shall be submitted no later than the end of the public comment period or the date of the first public hearing in the proceeding in which the proposed Participant seeks to become involved, whichever is later. For orders or decisions, the request shall be submitted within ten working days after the order or decision becomes final.
(2) The Petition to Participate shall contain the following:
a. The petitioner's name, mailing address, telephone number, and e-mail address, if any.
b. An identification of the proceeding in which the petitioner seeks to participate.
c. A clear and concise statement of the petitioner's interest in the proceeding explaining why participation is needed.
d. A statement adopting or amending the information submitted in support of the request for a determination of eligibility to participate and seek compensation, or, if there has been no prior submission, a showing of eligibility to participate on the basis that the petitioner Represents the Interests of Consumers as set forth in subpart c of this section.
e. An estimate of the fees to be sought.
(3) Approval of a Petition to Participate shall not guarantee the payment of the dollar amounts set forth in the estimate, or any amount whatever.
(4) Within 30 days of the receipt of a completed Petition to Participate, the Director shall rule on whether the Petition to Participate shall be granted. The petition may be denied if the Director determines that he or she elects not to award compensation to any participants in that proceeding, or that the petition does not meet the requirements of this regulation or the governing statute.
(5) An amended estimate shall be submitted as soon as possible when the Participant learns that the total estimated amount substantially increases. The Director may approve or disapprove of an amended amount.
(e) Procedure for Applying For An Award Of Fees.
(1) Following the issuance of a final regulation, order or decision by the Director in the proceeding, a Participant who has been found to be eligible for an award of compensation may submit within 60 days an application for an award of advocacy and witness fees. A Participant who makes a Substantial Contribution may be eligible for full compensation.
(2) The application for an award of compensation shall be submitted electronically to the designated departmental hearing officer and shall include:
a. A detailed, itemized description of the advocacy and witness services for which the Participant seeks compensation;
b. Legible time and/or billing records, created contemporaneously when the work was performed, which show the date and the exact amount of time spent on each specific task; and
c. A description of the ways in which the Participant's involvement made a Substantial Contribution to the proceeding as defined in subpart (b)(8), supported by specific citations to the record, Participant's testimony, cross-examination, arguments, briefs, letters, motions, discovery, or any other appropriate evidence.
(3) As used in this subdivision, the phrase “exact amount of time spent” refers either to quarters (15 minutes) of an hour for attorneys, or to thirty (30) minute increments for non-attorney advocates. The phrase “each specific task,” refers to activities including, but not limited to:
a. Telephone calls or meetings/conferences, identifying the parties participating in the telephone call, meeting or conference and the subject matter discussed;
b. Legal pleadings or research, or other research, identifying the pleading or research and the subject matter;
c. Letters, correspondence or memoranda, identifying the parties and the subject matter; and,
d. Attendance at hearings, specifying when the hearing occurred, subject matter of the hearing and the names of witnesses who appeared at the hearing, if any.
(4) Within 30 days after submission of the request, which will be posted on the Department's web site, the Department or any other person participating in the proceeding may file an objection to the request, which must be submitted to the Department and sent to the claiming Participant.
(5) If any person participating in the proceeding questions the Market Rates or reasonableness of any amount set forth in an application for an award of compensation, it shall disclose, in a verified declaration in support of its memorandum, the fees and rates which it anticipates will be, and which have been, billed or incurred for its advocates and witnesses in connection with the proceeding.
(6) The hearing officer may request additional information or documentation from the Participant to clarify or substantiate the claim, and, if considered necessary by the hearing officer, may request additional memoranda, and/or audit the records and books of the Participant to the extent necessary to verify the basis for the amount claimed in seeking the award.
(7) The hearing officer shall issue a written decision that determines whether or not the Participant has made a substantial contribution to the proceeding; and, if so, shall determine the amount of compensation to be paid, which may be all or part of the amount claimed. The decision will be posted promptly on the Department's web site and will be sent, electronically or by mail, as appropriate, to all parties who participated in the hearing.
(8) Within 30 days after posting and sending of the decision by the hearing officer, a Participant who is dissatisfied with that decision may appeal to the Director for review of the hearing officer's decision. The notice of appeal should state the relief which the Participant is seeking and the reasons why the decision by the hearing officer should be modified or changed. The Director may request additional briefing if the Director deems that would be helpful in reaching a decision. The review shall be of the written record and limited to whether the hearing officer's decision constituted an abuse of discretion. The Director's decision is final and there is no further administrative remedy.
NOTE
Authority cited: Sections 1341 and 1344, Health and Safety Code. Reference: Section 1348.9, Health and Safety Code.
HISTORY
1. New section filed 6-20-2003; operative 7-20-2003 (Register 2003, No. 25).
§1011. Assessment for University of California Analysis of Proposed Mandate Legislation.
Note • History
(a) For the fiscal years 2004-05 and 2005-06, the Department shall assess each full service plan its share of the amount necessary to fund the Health Care Benefits Fund for that fiscal year. The amount necessary for each fiscal year will be determined by the Department and the Department of Insurance in consultation with the University of California (University) and will be based on the amount necessary to fund the actual and necessary expenses of the University, not to exceed $2 million, in the analysis of legislative health care benefit mandates for the fiscal year.
(b) The total amount owed by all full-service health plans will be 87.6% of the total amount necessary to fund the Health Care Benefits Fund. That percentage is based on the ratio between persons enrolled in full-service health care service plans and those persons enrolled in health reimbursement plans regulated by the Department of Insurance as reported in the publication “Accident & Health Covered Lives 2002” (Revised December 11, 2003) published by the Department of Insurance in May, 2002.
(c) The Department shall annually calculate each full-service health plan's portion of the amount specified in subsection (b) as follows:
(1) The Department shall calculate the per-enrollee cost by dividing the amount of revenues required to be paid by all full-service health care service plans, by the total number of enrollees in this state that are enrolled in all full-service plans as of the March 31 immediately preceding the date of the assessment.
(2) The Department shall calculate each plan's annual fee by multiplying the per-enrollee cost determined pursuant to paragraph (1) of this subsection (c) by the number of enrollees in the plan as of the March 31 immediately preceding the date of the assessment.
(d) The Department shall notify affected plans of the amount of the assessment on or before June 15 of each fiscal year and all amounts due under the assessments will be due and payable from the affected plans on or before the first day of August immediately following the date of the notice.
(e) Any amount that remains due from a plan for assessments issued for the 2002-2003 and 2003-2004 fiscal years (pursuant to Section 127662 of the California Health and Safety Code) that have not been paid to the Department by May 31, 2004, will be added to the amount of the assessment due under the notice to be issued on or before June 15 of each fiscal year.
NOTE
Authority cited: Sections 1344, 1346 and 127662, Health and Safety Code. Reference: Sections 1356, 127660, 127661, 127662, 127663, 127664 and 127665, Health and Safety Code.
HISTORY
1. New section filed 6-2-2004; operative 7-2-2004 (Register 2004, No. 23).
Article 3. Electronic Filing
§1300.41.8. Electronic Filing.
Note • History
(a) Definitions:
(1) “Electronic” means relating to technology having electrical, digital, magnetic, wireless, optical, electromagnetic, or similar capabilities;
(2) “Electronic signature” means an electronic sound, symbol, or process attached to or logically associated with an electronic record, executed or adopted by a party with the intent to represent a manual signature.
(b) Notwithstanding any other provision of the regulations contained in title 28 of the CCR, plans shall file electronically any document required or permitted by law to be filed with the Department, or its designated agent, except as specified in subsection (d).
(c) Signatures:
(1) The Plan shall submit to the Director for approval, the manner, type, and format of signatures, including electronic signatures, which shall be required by the Department to be affixed to all filings.
(2) Prior to submitting electronically, the plan shall certify, under penalty of perjury, that all statements within all documents filed electronically with the Department are true and correct.
(3) Electronic signatures may be used to sign a legally effective declaration under penalty of perjury.
(4) If notarization is required, an electronic signature to be notarized must be accompanied by the electronic signature of a notary public and must include all other information to render the notarization effective under California law.
(5) The signature requirements apply to all plans, and their designated agents or representatives.
(d) The Director may grant a one-time limited exemption upon a satisfactory showing that a plan lacks the electronic capacity to satisfy the requirements for electronic filings.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1341.8, 1349, 1351, 1352, 1386 and 1387, Health and Safety Code; Sections 1633.1-1633.17, Civil Code (Uniform Electronic Transactions Act); and Section 16.5, Government Code.
HISTORY
1. New section filed 12-27-2001 as an emergency; operative 12-27-2001 (Register 2001, No. 52). A Certificate of Compliance must be transmitted to OAL by 4-24-2002 or emergency language will be repealed by operation of law on the following day.
2. New section refiled 4-24-2002 as an emergency; operative 4-24-2002 (Register 2002, No. 17). A Certificate of Compliance must be transmitted to OAL by 8-22-2002 or emergency language will be repealed by operation of law on the following day.
3. Certificate of Compliance as to 4-24-2002 order transmitted to OAL 6-28-2002 and filed 8-8-2002 (Register 2002, No. 32).
4. New article 3 heading filed 8-12-2002; operative 9-11-2002 (Register 2002, No. 33).
Chapter 2. Health Care Service Plans
HISTORY
1. Change without regulatory effect renumbering former Title 10, Chapter 3, Subchapter 5.5 (sections 1300.43-1300.826) to new Title 28, Division 1, Chapter 1 (sections 1300.43-1300.826) filed 12-22-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 51).
2. Editorial renumbering of former chapter 1 to new chapter 2 (Register 2001, No. 50).
Article 1. Exemptions
Note • History
A health care service plan or specialized health care service plan which provides health care services or specialized health care services only to the employees of one employer, or only to the employees of employers under common ownership and control, which is administered solely by the employer, and which does not have more than five subscribers (regardless of the number of persons enrolled based upon their relationship to or dependence upon such subscribers) is exempt from all provisions of the Act and the rules thereunder, except Sections 1381, 1384 and 1385. Such plans are exempt from any rules adopted pursuant to such sections unless such rules are made specifically applicable to plans exempted under this section.
NOTE
Authority cited: Section 6, Chapter 941, Statutes 1975, and Section 1344, Health and Safety Code. Reference: Knox-Keene Health Care Service Plan Act of 1975.
HISTORY
1. New Subchapter 5.5, Articles 1-14 (1300.43-1300.99, not consecutive) filed 6-1-76; effective thirtieth day thereafter (Register 76, No. 23).
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. Amendment filed 11-30-76 as an emergency; effective upon filing (Register 76, No. 49). For prior history, see Register 76, No. 42.
2. Reinstatement of section as it existed prior to emergency amendment filed 11-30-76, by operation of Section 11422.1(b), Government Code (Register 77, No. 24).
3. Repealer filed 6-29-84; effective thirtieth day thereafter (Register 84, No. 26).
§1300.43.2. Extension for Enrollers Under Medi-Cal Program.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 8-12-76 as an emergency; effective upon filing (Register 76, No. 33).
2. Amendment filed 9-30-76 as an emergency; effective upon filing (Register 76, No. 40).
3. Amendment filed 10-12-76 as an emergency; effective upon filing. Certificate of Compliance included (Register 76, No. 42).
4. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.43.3. Ambulance Plans: Conditional Exemption.
Note • History
(a) Definitions. For the purposes of this section:
(1) “Ground ambulance services” means the emergency, including advanced life support services, and non-emergency transportation of an enrollee by an individual licensed pursuant to Articles 1 and 2 of Chapter 2.5 of Division 2 of the Vehicle Code where health care services are provided to an enrollee for the duration of such transportation.
(2) “Air ambulance services” means the emergency, including advanced life support services, and non-emergency transportation of an enrollee by legally authorized air ambulance where health care services are provided to the enrollee for the duration of such transportation.
(b) A health care service plan which lawfully operates air and/or ground ambulances and provides pursuant to a plan contract only air and/or ground ambulance services to subscribers and enrollees in ambulances owned or leased by it and operated by its employees (hereinafter “Ambulance Plan”) is exempted from all provisions of the Knox-Keene Health Care Service Plan Act of 1975 (Health and Safety Code section 1340 et seq.) except those provisions specified herein, and subject to the condition that the Ambulance Plan complies with each of the following requirements:
(1) Every Ambulance Plan shall directly provide ground and/or air ambulance services for its enrollees throughout the Ambulance Plan's service area exclusively in ambulances owned or leased by it and operated by its employees.
(2) At the time of initial enrollment or renewal, every plan contract between an Ambulance Plan and a group or individual subscriber, and every disclosure form, evidence of coverage or plan brochure shall prominently display as a separate article the following legend, in boldface type and font size not smaller than the font size used in the general body of the document, either on the first page or on another page if referenced as “See Important Notices on Page [insert page number] Prior to Purchase” in boldface type and font size not smaller than the font size used in the general body of the document on the front page:
(A) “BEFORE YOU PURCHASE: If you are currently enrolled in a health maintenance organization (HMO) or other health insurance, the benefits provided by an Ambulance Plan may duplicate the benefits provided by your HMO or other health insurance. If you have a question regarding whether your HMO or other health insurance offers benefits for ambulance services, you should contact that other company directly.”
(B) “WARNING: This Ambulance Plan is not an insurance program. It will not compensate or reimburse another ambulance company that provides emergency transportation to you or your family. This may occur when the 911 Emergency System has independently determined that another company could provide more expeditious service or is next in the rotation to receive a call. This might also occur when this Ambulance Plan is unable to perform within a medically appropriate timeframe due to a mechanical or maintenance problem or being on another call.” Immediately following this warning, the Ambulance Plan shall include the words, “sign or initial here,” and include a line for the subscriber's signature or initials.
(C) “COMPLAINTS: For complaints regarding this Ambulance Plan, first attempt to call the plan at [plan's toll-free telephone number]. If the Ambulance Plan fails to resolve the complaint to your satisfaction, contact the Department of Managed Health Care at 1-800-400-0815. The Department's website is http://www.dmhc.ca.gov. You may obtain complaint forms and instructions online.”
(D) “OPERATING UNDER CONDITIONAL EXEMPTION: This Ambulance Plan is operating pursuant to an exemption from the Knox-Keene Health Care Service Plan Act of 1975 (Health and Safety Code section 1340 et seq.).”
The Ambulance Plan may amend the wording of the legend to use its name and personal pronouns.
(3) Ambulance Plans that fail to comply with all of subsection (b)(2), including obtaining the signature or initials of subscribers next to or under the “WARNING” statement, shall be responsible for paying, reimbursing, or covering the enrollee's cost for ambulance transportation services provided by another ambulance company, less any compensation received from the subscriber's HMO, health insurer, or managed care organization, if any, and less any applicable overall annual deductible or any co-payment.
(4) An Ambulance Plan shall operate in compliance with the requirements of each local emergency medical services agency (Health and Safety Code section 1797.94) that regulates emergency services in any portion of the plan's service area and that has developed an emergency medical services plan (Health and Safety Code section 1797.76) for an emergency medical services system (Health and Safety Code section 1797.78), implemented pursuant to the authority granted in Health and Safety Code section 1797.105(b).
(5) No Ambulance Plan shall offer or sell plan contracts to or for persons who do not live or work in the plan's service area, or use or permit the use of any advertising or solicitation regarding its services outside of its service area. Every Ambulance Plan shall comply with the following sections of the Health and Safety Code: 1360, 1363.1, 1365(a), 1365.5, 1366, subsections (a), (b), (c), (d), (e)(1), (f), (g), and (h)(1) of section 1367, 1368, 1368.01, 1368.02(b), 1373(a), 1379, 1381, subsections (a), (d), and (f) of 1384, and 1385, except that approval by the Department under section 1368(a)(1) is waived.
(6) Every Ambulance Plan shall maintain a procedure whereby enrollees, or authorized persons on their behalf, may submit grievances to the plan and in each case receive from the plan a written acknowledgement within five days of receipt of the grievance and a written response sent within 30 days of receipt of the grievance indicating what the plan will do to resolve the grievance. Both the acknowledgement and the response shall include a notice that the enrollee may contact the Department of Managed Health Care through the Department's toll-free telephone number after the grievance has been pending with the plan for at least 30 days.
(7) No Ambulance Plan contract shall require, nor shall the Ambulance Plan or any contracting provider collect, a co-payment of greater than 50 percent of an ambulance or other emergency care provider's negotiated fee-for-service rate pursuant to a contract with the ambulance service, or, in the absence of such a contract, 50 percent of the ambulance company's usual, customary, and reasonable rate (within the meaning of Business and Professions Code section 657(c)) for the particular service, or $500, whichever amount is less. An Ambulance Plan that does not impose any co-payments may impose an overall annual deductible of a specified dollar amount applicable to all covered services, provided that the deductible for an enrollee shall not exceed:
(A) 200 percent of the amount of prepaid or periodic charge for one year for the enrollee; or
(B) 200 percent of the amount of prepaid or periodic charge for one year for the family, whichever is less.
(8) Every Ambulance Plan operating ground or air ambulances shall:
(A) If operating a ground ambulance, provide proof to the Director upon request that the Ambulance Plan currently complies with Articles 1 and 2 of Chapter 2.5 of Division 2 of the California Vehicle Code, including but not limited to license and certification requirements, and with professionally recognized standards of patient care and safety in emergency medical services and transport.
(B) If operating an air ambulance, provide proof to the Director upon request that the Ambulance Plan currently complies with regulations established by the Federal Aviation Administration and with professionally recognized standards of patient care and safety in emergency medical air services and transport.
(9) Every Ambulance Plan operating air ambulances shall comply with the general standards and other applicable standards and provisions of the “Association of Air Medical Services Standards and Safety Guidelines for Fixed Wing, Rotorwing, & Critical Care Ground Services,” revised June 2000 and published by the Association of Air Medical Services, which is incorporated by reference.
(10) No Ambulance Plan shall receive prepaid or periodic charges pursuant to its plan contract for more than one year in advance.
(11) Every Ambulance Plan shall deliver:
(A) To each prospective subscriber, upon presenting a plan contract for offer or sale, a disclosure form, combined disclosure form and evidence of coverage, or copy of its plan contract,
(B) Annually, to each subscriber a copy of its plan contract and evidence of coverage, and
(C) To each subscriber and enrollee a membership card or other form of identification easily carried by the subscriber or enrollee that indicates that the subscriber or enrollee is an Ambulance Plan member and that lists phone numbers and other instructions for activating ambulance transport.
(12) The plan contract and any disclosure form and evidence of coverage used by the Ambulance Plan, shall comply with Health and Safety Code sections 1362 and 1363 and the rules of the Director of the Department of Managed Health Care pursuant to and including sections 1300.63, 1300.63.1, 1300.63.2, and 1300.63.3 of title 28.
(13) Every Ambulance Plan must maintain documentation demonstrating compliance with all the conditions of the exemption and provide to the Department of Managed Health Care all or any part of such documentation as required by the Department within 30 days of request.
(14) No Ambulance Plan shall purport to rely on the exemption pursuant to this section if the Director has issued an order of termination pursuant to subsection (c).
(c) An Ambulance Plan's exemption pursuant to this section may be terminated by order of the Director, upon a determination that such action is in the public interest and for the protection of enrollees, or for any of the following reasons:
(1) The services of the Ambulance Plan are not accessible to enrollees.
(2) The Ambulance Plan, or a person employed by the Ambulance Plan, has failed to comply with licensing or certification requirements imposed by law.
(3) The Ambulance Plan is operating in an unsafe, unfair, unreasonable or discriminatory manner as to its enrollees or as to its enrollment practices.
(4) The financial condition of the Ambulance Plan is such that its continued operation will constitute a substantial risk to its subscribers and enrollees.
(5) The Ambulance Plan has engaged in conduct proscribed by the Health and Safety Code section 1386(b), subsections (5), (6), (7), (8), (9), (10), (11), or (14).
(6) The Ambulance Plan has been or is subject to a limitation, requirement, condition, adverse action, or disciplinary action taken by a licensing agency or an emergency medical services agency that would materially impair its ability to perform its plan contracts or constitute or result in a violation of the provisions of this section or of the referenced provisions of the Act.
(7) The Ambulance Plan has violated any condition of this exemption.
(d) An Ambulance Plan's exemption pursuant to this section shall terminate automatically by operation of law upon the plan's failure to comply with any of the conditions set forth in subsection (b).
(e) An Ambulance Plan whose exemption has been terminated by operation of law because of failure to comply with the conditions set forth in subsection (b) or by order of the Director under subsection (c) shall be in violation of section 1349 of the Health and Safety Code and shall be subject to all of the provisions of the Knox-Keene Health Care Service Plan Act of 1975, including but not limited to the provisions relating to discipline and enforcement procedures.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1343(b), Health and Safety Code.
HISTORY
1. New section filed 9-30-76 as an emergency; effective upon filing (Register 76, No. 40).
2. Certificate of Compliance filed 1-27-77 (Register 77, No. 5).
3. Amendment filed 4-2-79; effective thirtieth day thereafter (Register 79, No. 14).
4. Editorial correction of subsections (a)7.f. and (b)(6) (Register 80, No. 4).
5. Change without regulatory effect amending section filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
6. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
7. Change without regulatory effect updating title references in Notice filed 12-22-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 51).
8. Change without regulatory effect amending subsection (a)--form filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
9. Repealer and new section heading and section and amendment of Note filed 7-24-2003; operative 8-23-2003 (Register 2003, No. 30).
§1300.43.4. Employee Welfare Benefit Plans.
Note • History
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. Amendment filed 3-6-78 as an emergency; designated effective 3-6-78 (Register 78, No. 10). For prior history, see Register 77, No. 36.
2. Certificate of Compliance filed 4-20-78 (Register 78, No. 16).
3. Amendment filed 8-14-78 as an emergency; designated effective 8-15-78 (Register 78, No. 33).
4. Certificate of Compliance filed 11-8-78 (Register 78, No. 45).
. 5. Repealer filed 9-27-79; effective thirtieth day thereafter (Register 79, No. 39).
§1300.43.5. Exemption for Licensees of Insurance Commissioner.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 12-20-77 as an emergency; effective upon filing (Register 77, No. 52).
2. Certificate of Compliance filed 4-4-78 (Register 78, No. 14).
3. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
Note • History
A health care service plan which is a general acute care hospital whose business as a plan is limited to providing, administering, or otherwise arranging for the provision of health care services to members of one moribund group of not more than 250 members is exempted from the provisions of the Knox-Keene Health Care Service Plan Act of 1975, subject to each of the following conditions:
(a) That such plan is licensed as a health facility pursuant to Chapter 2 (commencing with Section 1250) of the Health and Safety Code, and is not insolvent.
(b) That such plan has not accepted any new members for the last twenty years and does not accept any new members for the duration of this exemption.
(c) That such plan receives prepaid or periodic charges, if any, from members of such group in an amount not exceeding $5 per member per month and has received no substantial payment or transfer of property from or on behalf of such contracting group during the last twenty years.
(d) That such plan derives not more than one-half of one percent of its annual income from prepaid or periodic charges paid by or on behalf of members of such group, and has a minimum net worth of $15,000,000 based upon its most recent certified financial statements (prepared as of a date within the preceding 15 months).
(e) That such plan establish and maintain a grievance procedure substantially complying with Section 1300.68.
(f) That such plan deliver to each subscriber and enrollee within 60 days of the adoption of this section, and thereafter to any subscriber or enrollee upon request, the following written notice:
“(Name of plan) IS A HEALTH CARE SERVICE PLAN OPERATING PURSUANT TO AN EXEMPTION FROM THE KNOX-KEENE HEALTH CARE SERVICE PLAN ACT OF 1975 PROVIDED BY RULE OF THE DIRECTOR OF THE DEPARTMENT OF MANAGED HEALTH CARE OF THE STATE OF CALIFORNIA.”
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 6-13-78 as an emergency; effective upon filing (Register 78, No. 24).
2. Certificate of Compliance filed 8-18-78 (Register 78, No. 33).
3. Editorial correction of subsection (f) (Register 95, No. 12).
4. Change without regulatory effect amending subsection (f) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
5. Change without regulatory effect amending subsection (f) filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.43.7. Student Emergency Care Arrangements.
Note • History
There is exempted from the provisions of the Act any nonprofit corporation or association all of whose members are licensed physicians and which is a health care service plan as defined by subdivision (f) of Section 1345 only by reason of health care service plan contracts with one or more colleges or universities pursuant to which such nonprofit corporation or association furnishes or arranges only emergency health care services and health care services ancillary thereto to members of the student body of, employees of, and visitors to such colleges or universities, provided that each of the following conditions is met:
(a) At least 95 percent of the cost of health care services furnished pursuant to such contracts is furnished by employees or members of such nonprofit corporation or association or contracting providers.
(b) All services furnished by members pursuant to such contracts are furnished pursuant to provider contracts which comply with Section 1379 of the Act.
NOTE
Authority cited: Section 1343, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 8-22-78; effective thirtieth day thereafter (Register 78, No. 34).
Note • History
NOTE
Authority cited: Section 1343, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 9-27-79; effective thirtieth day thereafter (Register 79, No. 39).
2. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.43.9. Unlicensed Solicitors and Solicitor Firms.
Note • History
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 11-9-79 as an emergency; effective upon filing (Register 79, No. 45). A Certificate of Compliance must be filed within 120 days or emergency language will be repealed on 3-9-80.
2. Repealed by operation of Section 11422.1(c), Government Code (Register 80, No. 24).
§1300.43.10. Nonprofit Retirees' Plan.
Note • History
A health care service plan which was registered under the Knox-Mills Health Plan Act as in effect on June 30, 1976, whose activity as a plan is limited to reimbursing part or all of the cost of health care services as a supplement to Medicare (Parts A and B) to persons who were retired from professions associated with higher learning after having been employed therein for not less than 10 cumulative years and such persons' spouses, providing all such persons are enrolled in Medicare, is exempted from the provisions of Section 1349 of the Knox-Keene Health Care Service Plan Act of 1975, subject to each of the following conditions:
(a) That such plan is a nonprofit corporation which does not engage, directly or indirectly, in any for profit business, which is not affiliated with (Rule 1300.45(c)) a corporation or other entity which engages, directly or indirectly, in any for profit business, and which does not contract or otherwise arrange for the performance by persons other than its directors, officers or employees of any portion of its administrative or other functions.
(b) That such plan is exempted from federal income tax as an organization described in Section 501(c)(3) of the Internal Revenue Code and from state income tax on similar grounds.
(c) That such plan is a charitable corporation subject to, and in compliance with, the Uniform Supervision of Trustees for Charitable Purposes Act.
(d) That such plan does not directly provide any health care services through entity-owned or contracting health facilities or providers.
(e) That such plan has a tangible net equity within the meaning of Section 1300.76(b) of not less than $300,000, including liquid tangible assets in an amount not less than $300,000, based upon its most recent certified financial statement (prepared as of a date within the preceding 15 months and such other date as may be requested by the Director pursuant to Section 1384 of the Act) and its most recent quarterly and monthly uncertified statements prepared on a basis consistent with the annual certified statement, with additional liquid tangible assets in an amount not less than $1,000 for each person enrolled in excess of 400; provided that the maximum number of enrollees shall not exceed 500.
(f) That not more than 15% of the total charges paid by or on behalf of subscribers or enrollees for enrollment in, or for health care benefits from, such plan is expended for administrative costs, including all costs of solicitation and enrollment; except that such plan may expend additional sums of money for administrative costs excluding costs of solicitation and enrollment provided that such money is not derived from revenue obtained from subscribers or enrollees.
(g) That such plan issues a uniform health care service plan contract to all subscribers
(1) which provides, except for a permissible calendar year deductible not to exceed $100 per enrollee, full coverage for all copayments and deductibles relating to allowable charges under Medicare (Parts A and B) for all health care services covered by Medicare (Parts A and B) pursuant to Title XVIII of the Social Security Act as amended, and not less than 50% of the reasonable charges for each health care service which is not covered by Medicare but is covered by such plan; provided, however, that such coverage may be subject to a lifetime limitation allowing not less than $300,000 of benefits per lifetime and
(2) which provides that an enrollment or subscription may not be cancelled except upon grounds complying with Section 1365 of the Act.
(h) That such plan provides to each subscriber a disclosure statement covering the provisions of its health care service plan contract which complies substantially with the provisions of Section 1363 of the Act and which also states, if such is the case, that such contract does not cover, and that subscribers and enrollees will be solely liable for,
(1) any charges in excess of allowable charges under Medicare with respect to health care services covered by Medicare,
(2) any charges in excess of reasonable charges for any health care services covered by such plan but not covered by Medicare and any copayments related to such health care services, and
(3) any permissible plan deductible.
(i) That no less than 75% of the officers and of the directors of such corporation are persons who are retired from the professions associated with higher learning after having been employed therein not less than 10 cumulative years, are enrolled in Medicare, and are enrolled in such plan subject to terms and conditions no more favorable than any other enrollee, and that no officer or director receives any compensation from such corporation.
(j) That such plan solicits enrollments or subscriptions in this state only through persons who are officers or employees of such plan.
(k) That such plan establishes and maintains a grievance procedure substantially complying with Section 1300.68 of these rules.
(l) That such plan not represent any contract of such plan as a Medicare supplement contract and discloses to each prospective subscriber and enrollee when presenting any information regarding the plan, and again at the time of application, the following written notice:
“THE HEALTH PLAN CONTRACT OFFERED BY (Name of plan) DOES NOT MEET THE REQUIREMENTS FOR CERTIFICATION AS A MEDICARE SUPPLEMENT CONTRACT PURSUANT TO APPLICABLE STATE OR FEDERAL LAW, AND HAS NOT BEEN CERTIFIED. PERSONS DESIRING INFORMATION REGARDING CERTIFIED MEDICARE SUPPLEMENT COVERAGE SHOULD CONTACT THEIR LOCAL MEDICARE OFFICE.”
(m) That such plan delivers to each subscriber and enrollee within 60 days of the adoption of this section, and annually thereafter, the following written notice:
“(Name of plan) IS A HEALTH CARE SERVICE PLAN OPERATING PURSUANT TO AN EXEMPTION FROM THE KNOX-KEENE HEALTH CARE SERVICE PLAN ACT OF 1975. COMPLAINTS REGARDING THIS PLAN, THE ADMINISTRATION THEREOF, AND THE SERVICES PROVIDED THEREBY MAY BE DIRECTED TO THE DIRECTOR OF THE DEPARTMENT OF MANAGED HEALTH CARE OF THE STATE OF CALIFORNIA.”
(n) That such plan provides written notice to the Director of its intent to rely on the exemption provided by this section, executed by a duly authorized officer of such plan, together with a signed opinion of legal counsel to the effect that such plan complies with subsections (a), (b), (c), (d) and (g) of this section.
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 11-21-79; effective thirtieth day thereafter (Register 79, No. 47).
2. Amendment filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
3. Change without regulatory effect amending subsections (e), (m) and (n) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
4. Change without regulatory effect amending subsection (m) filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.43.11. Exemption for Solicitors of Nonprofit Retirees' Plans.
Note • History
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 11-21-79; effective thirtieth day thereafter (Register 79, No. 47).
2. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.43.12. Medi-Cal Dental Contract.
Note • History
The contract of the Department of Health Services which is entered as the result of successful bidding in response to said Department's request for proposal and which requires the contractor to provide only dental benefits for the state's Medi-Cal beneficiaries pursuant to Section 14104.3 of the Welfare and Institutions Code and incorporates the terms and provisions set forth in the request for proposal, is exempt from the provisions of the Act, if the successful bidder (“entity”) is not already licensed under the Act, for the period indicated below, subject to each of the following:
(a) The entity engages in no activities as a plan other than those pursuant to the Medi-Cal dental contract described above or pursuant to a separate exemption in the Act or these rules.
(b) The entity properly files an application for licensure under the Act, as required by Sections 1351 and 1356 of the Act, prior to executing the contract referred to above, except that the information contained in the application submitted at the time of filing need not include information not required to be provided to the Department of Health Services pursuant to its request for proposal, so long as the additional information required by Section 1351 of the Act or by the application form provided by the Director is filed as an amendment to the license application within six weeks of the date of execution of the contract referred to above, or any longer period as the Director by order may allow under the Director's waiver authority set forth in Section 1344(a) of the Act.
(c) The entity reasonably pursues the completion of its application and compliance with the provisions of the Act and applicable rules thereunder.
(d) The entity, for the duration of the exemption provided by this section, shall be subject to the provisions of Sections 1351.1, 1381, 1384, and 1385 of the Act, and may be examined by the Director in the manner and subject to the arrangements provided in Section 1382 of the Act.
(e) The exemption provided by this section shall be effective only until the earlier of
(1) final action by the Director on the application, or
(2) the expiration of nine months after execution of the contract referred to above, except that said nine month period may be waived by order of the Director for any additional one month periods under the Director's waiver authority set forth in Section 1344(a) of the Act.
(f) For the purposes of this section, the term “order” means a written waiver applicable to a specific case issued by the Director pursuant to Section 1344(a) of the Act.
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Sections 1343, 1344, 1351, 1351.1, 1353, 1356, 1381, 1382, 1384 and 1385, Health and Safety Code.
HISTORY
1. New section filed 3-9-84; effective thirtieth day thereafter (Register 84, No. 10).
2. Change without regulatory effect amending subsections (b) and (d)-(f) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.43.13. Mutual Benefit Plans.
Note • History
A health care service plan which is a bona fide mutual benefit society within the meaning of this section and which was registered under the Knox-Mills Health Plan Act as in effect on June 30, 1976 is exempted from the provisions of the Knox-Keene Health Care Service Plan Act, except as otherwise indicated below, subject to each of the following conditions:
(a) That such a plan is a corporation organized and operating as a California nonprofit corporation; does not engage, directly or indirectly, in any for-profit business; is not affiliated (Rule 1300.45(c)) with any other plan or with any corporation or other entity which engages, directly or indirectly, in any for-profit business; and does not contract or otherwise arrange for the performance of any portion of its administrative functions by persons other than its officers, directors, or employees.
(b) That such plan consists of a mother lodge and not more than one subordinate lodge; provided, however, that such mother lodge and any such subordinate lodge are located in a county whose population exceeds 1,500,000 persons.
(c) That the assets and funds available for the payment of health care services are held in trust by and under the sole control of the mother lodge exclusively for the benefit of the beneficiary members of the mother lodge and any subordinate lodge.
(d) That such plan is exempted from federal income tax as an organization described in Section 501(c)(8) of the Internal Revenue Code and from state income tax on similar grounds.
(e) That such plan is in compliance with the Uniform Supervision of Trustees for Charitable Purposes Act (Article 7 (commencing with Section 12580) of Chapter 6 of Part 2 of Division 3 of Title 2 of the Government Code.)
(f) That such plan not practice any discrimination in violation of state or federal law or constitutional provision.
(g) That the beneficial membership in such plan is limited to beneficial members of the mutual benefit society (including only the mother lodge and any subordinate lodge) and consists of a total of not more than 800 persons.
(h) That such plan not receive any prepaid or periodic charges, except that admission fees of not more than $500 per each beneficial or social member may be received and dues of not more than $100 per each beneficial or social member per year may be received, provided, however, that no part of any admission fees or membership dues may be deposited in the health care trust or used to pay for or reimburse any part of the cost of health care services.
(i) That such plan, at all times while it relies upon this exemption, has a tangible net equity within the meaning of Section 1300.76(b) of not less than $500,000, including liquid tangible assets in an amount not less than $500,000, based upon its most recent annual certified financial statement and its most recent quarterly and monthly statements prepared on a basis consistent with the annual certified statement, with additional liquid tangible assets in an amount not less than $1,000 for each beneficial member in excess of 700; provided that the maximum number of beneficial members shall not exceed 800.
(j) That such plan, upon request of the Director, pursuant to Section 1384(a) of the Act, submits to the Director a copy of its most recent annual certified financial statement, and, upon request of the Director pursuant to Section 1384(f) of the Act, submits to the Director its most recent quarterly and monthly statements prepared on a basis consistent with the annual certified statement.
(k) That such plan issues to all beneficial members health care service plan contracts which provide at least all of the benefits indicated below, except that such contracts may diminish or qualify any of the benefits indicated below through the use of such copayments, limitations, and other terms as may be determined from time to time by vote of the plan's beneficial members:
(1) Physician services (including consultation and referral) through contracting physicians;
(2) Hospital inpatient services through at least one contracting nonprofit, nongovernmental hospital;
(3) Hospital outpatient services through at least one contracting nonprofit, nongovernmental hospital when prescribed by the treating, contracting physician.
(l) That all of the plan's contracts with providers comply with, and recite that the contracting providers are bound by, the provisions of Section 1379 of the Act.
(m) That such plan provides to each beneficial member a disclosure statement covering the provisions of its health care service plan contract which complies substantially with the provisions of Section 1363 of the Act.
(n) That the officers and directors of such corporation are enrolled in such plan subject to terms and conditions no more favorable than any other beneficial member, and that no officer or director receives any compensation from such corporation.
(o) That such plan solicits beneficial members in this state only through persons who are officers, directors, or employees of such plan, and not by means of any unsolicited telephone call or written or printed communication or by radio, television, or similar communications media.
(p) That such plan establishes and maintains a grievance procedure substantially complying with Section 1368 of the Act.
(q) That such plan delivers to each beneficial member within 60 days of the effective date of this section, and annually thereafter, the following written notice:
“(Name of Plan) IS A HEALTH CARE SERVICE PLAN OPERATING PURSUANT TO AN EXEMPTION FROM THE KNOX-KEENE HEALTH CARE SERVICE PLAN ACT OF 1975. COMPLAINTS REGARDING THIS PLAN, THE ADMINISTRATION THEREOF, AND THE SERVICES PROVIDED THEREBY MAY BE DIRECTED TO THE DIRECTOR OF THE DEPARTMENT OF MANAGED HEALTH CARE OF THE STATE OF CALIFORNIA.”
(r) That such plan provides, within 60 days of its initial reliance on this section, and within 30 days of any subsequent request of the Director therefor, written notice to the Director of its intent to rely on the exemption provided by this section, executed by a duly authorized officer of such plan, together with a signed opinion of legal counsel to the effect that such plan complies with subsections (a), (b), (c), (d), (e), (f), (g), (h), (i), (k), (l), and (m) of this section.
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Sections 1343 and 1344, Health and Safety Code.
HISTORY
1. New section filed 6-5-84; effective thirtieth day thereafter (Register 84, No. 23).
2. Change without regulatory effect amending subsections (j) and (q)-(r) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
3. Change without regulatory effect amending subsection (q) filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.43.14. Employee Assistance Programs.
Note • History
(a) A health care service plan which, pursuant to a contract with an employer, labor union or licensing board within the Department of Consumer Affairs, consults with employees, members of their families or licensees of such board to identify their health, mental health, alcohol and substance abuse problems and refer them to health care providers and other community resources for counseling, therapy or treatment, is exempt from the provisions of the Act (other than Sections 1360, 1360.1, 1368 and 1381, relating to advertising, client grievance procedures and the inspection of records by the Director) if the plan complies with each of the following provisions, and the contracts of a licensed health care service plan are exempt from the provisions of the Act if they comply with each of the following provisions:
(1) The plan has filed a notice with the Director as provided in subsection (c) within the preceding 24 months.
(2) The purpose of the contract, insofar as it relates to the provision of services to clients is either
(A) to maintain or improve employee efficiency through identification and referrals for counseling, treatment or therapy, in connection with personal problems affecting employee performance and the contract does not provide for counseling, treatment or therapy with respect to health, mental health, alcohol or substance abuse problems or
(B) to identify alcohol and substance abuse problems or mental health or health problems of DCA licensees and refer them to appropriate health care providers or organizations for treatment, and the plan does not provide for counseling, treatment or therapy with respect to health, mental health, alcohol or substance abuse problems.
(3) No client or member of his or her family, directly or indirectly shall pay any prepaid or periodic charge under the contract or pay any copayment, fee or other charge for any service rendered under the contract in connection with a health, mental health, alcohol or substance abuse problem. The payment of regular union dues by an employee, a license fee by a DCA licensee, or of a benefit payment by an employer on behalf of an employee and members of the employee's family which does not affect the employee's compensation or other benefits is not a “prepaid or periodic charge” for the purpose of this subsection.
(4) If such plan, its employees or contracting consultants, or an affiliate of any of the foregoing, has a financial interest in referrals made under the contract in connection with a health, mental health, alcohol or substance abuse problem, such person prior to making any such referral shall disclose to the contracting employer, union or state licensing agency and to the person who is referred, the existence of such financial interest; provided that neither the plan nor its employees shall receive any payment, fee or commission directly or indirectly from any person to whom an employee, licensee or family member is referred for counseling, treatment or therapy. The disclosure requirement to the employer may be a single blanket disclosure provided it identifies the providers to which referrals will be made and identifies the financial interest involved.
(5) The number of sessions with any client under the contract shall not exceed 3 within any six month period.
(6) Except as otherwise provided in Division 2 (commencing with Section 500) of the Business and Professions Code, the plan shall maintain a record for a period of not less than two years of each session with a client concerning a health, mental health, alcohol or substance abuse problem, and each consultation excluded from the definition of “session.” The record shall include the name of or identifier for the client, the date and purpose of the session and the outcome if any, including the name of the provider to which the client was referred. The employee assistance program contracts and the records specified pursuant to subparagraph (6) shall be available for inspection by the Director as provided in Section 1381 of the Act.
(7) The plan and the personnel, facilities and equipment of the plan, including that employed under contract, shall be licensed or certified when required by applicable law and persons engaged in identification and referral who are not licensed under Division 2 of the Business and Professions Code shall be certified by any of the following organizations:
(A) Any organization accredited by the National Commission for Accreditation of Alcohol/Drug Abuse Counselors' Credentialing Bodies, Inc.
(B) Alcoholism Council of California.
(C) California Association of Alcoholism and Drug Abuse Counselors.
(D) Association of Labor-Management Administrators and Consultants on Alcoholism.
(8) Unless the plan is licensed under the Act, no prepaid fees shall be collected more than 45 days in advance.
(b) For the purposes of this section the following definitions apply:
(1) “Client” means the employee, the employee's family member, the DCA licensee or other person eligible for the services provided under the plan contract.
(2) “DCA licensee” means a licensee of the Department of Consumer Affairs.
(3) “Session” means any in-person or telephone consultation with the client in connection with the client's health, mental health, alcohol or substance abuse problems, excluding a consultation that occurs in an acute emergency situation, a consultation after referral for motivation or re-referral or a consultation due to a management, state licensing agency or union request for information or assessment regarding work performance issues.
(c) The notice specified in subsection (a)(1) shall be in the following form and contain the information specified below:
DEPARTMENT OF MANAGED HEALTH CARE
STATE OF CALIFORNIA
NOTICE OF EMPLOYEE ASSISTANCE PROGRAM
EXEMPTION RULE 1300.43.14,
KNOX-KEENE HEALTH CARE SERVICE PLAN ACT
( ) Original Notice ( ) Amendment to Notice Dated
The person/entity named in Item 1 below files this notice/amended notice claiming the exemption pursuant to Rule 1300.43.14 under the Knox-Keene Health Care Service Plan Act:
1. Legal name of person or entity filing this notice:
2. Address of principal office, and if different, mailing address:
3. Fictitious names used in connection with the operation of employee assistance programs (if none, so specify):
4. Identify each location at which the plan maintains records subject to inspection by the Director under Rule 1300.43.14(a)(6) (if space is insufficient, continue on separate sheet):
5. Name, title, address and telephone number of representative who may be contacted concerning this notice:
6. The person/entity filing this notice declares hereby that it is in compliance with the provisions of Rule 1300.43.14, and undertakes to amend this notice within 30 calendar days of any material change in the information specified in its current notice as filed with the Director of the Department of Managed Health Care.
Date of Notice
(Name of Person/Entity Filing Notice)
(Signature of Authorized Officer)
(Printed Name and Title of Signatory)
Verification:
I certify (or declare) under penalty of perjury under the laws of the State of California that I have read this Notice and its attachments thereto and know the contents thereof and that the statements therein are true and correct.
Executed at ____________________ on ____________
(City and State) (Date)
(Signature)
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 6-12-87; operative 6-12-87 (Register 87, No. 28).
2. Change without regulatory effect amending section filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
3. Change without regulatory effect amending subsections (a)-(a)(1), (a)(6) and (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
4. Change without regulatory effect amending subsection (c)--form filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
Note • History
(a) There is exempted from the provisions of the Act (other than Sections 1360, 1360.1, 1381 and 1395) any plan whose activity in this state is limited to the offer and sale of plan contracts for enrollees who are residents of or domiciled in a foreign country, provided:
(1) the provision of health care services by the plan, and the receipt of consideration from persons located in this State, does not violate any law of the foreign country in which the enrollee resides or any law of the United States,
(2) the annual premium per enrollee does not exceed $200 (US),
(3) the solicitors or solicitor firms authorized to solicit on behalf of the plan are physically present in this state, and
(4) the plan has filed a notice with the Director as provided in subsection (b) within the preceding 24 months.
(b) The notice specified in subsection (a) shall be in the following form and contain the information specified below:
DEPARTMENT OF MANAGED HEALTH CARE
STATE OF CALIFORNIA
NOTICE OF FOREIGN PLAN EXEMPTION
RULE 1300.43.15, KNOX-KEENE HEALTH CARE
SERVICE PLAN ACT
( ) Original Notice ( ) Amendment to Notice Dated
The person/entity named in Item 1 below files this notice/amended notice claiming the exemption pursuant to Rule 1300.43.15 under the Knox-Keene Health Care Service Plan Act:
1. Legal name of person or entity filing this notice:
2. Address of principal office, and if different, mailing address:
3. List name, address and telephone number of authorized solicitors or solicitor firms who will be soliciting on behalf of the plan in this state. (Continue on separate sheet if space is insufficient.)
4. Name, title, address and telephone number of representative who may be contacted concerning this notice:
5. The person/entity filing this notice declares hereby that it is in compliance with the provisions of Rule 1300.43.15, and undertakes to amend this notice within 30 calendar days of any material change in the information specified in it current notice as filed with the Director of the Department of Managed Health Care.
Date of Notice
(Name of Person/Entity Filing Notice)
(Signature of Authorized Officer)
(Printed Name and Title of Signatory)
Verification:
I certify (or declare) under penalty of perjury under the laws of the State of California that I have read this Notice and its attachments thereto and know the contents thereof and that the statements therein are true and correct.
Executed At ________________ on ________________ 19____.
(Signature)
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Section 1343, Health and Safety Code.
HISTORY
1. New section filed 9-8-88; operative 10-8-88 (Register 88, No. 38).
2. Change without regulatory effect amending subsections (a)(4) and (b) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
3. Change without regulatory effect amending subsection (b)--form filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
Article 2. Administration
§1300.44. Interpretive Opinions.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code.
HISTORY
1. Repealer filed 6-29-84; effective thirtieth day thereafter (Register 84, No. 26).
§1300.44.1. Application for Exemption from Rule.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1344, 1351 and 1352, Health and Safety Code.
HISTORY
1. Amendment of subsection (b) filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Repealer filed 6-29-84; effective thirtieth day thereafter (Register 84, No. 26).
Note • History
In addition to the definitions contained in Section 1345 of the Act, the following definitions apply to the interpretation of these rules and the Act:
(a) “Act” means the Knox-Keene Health Care Service Plan Act of 1975.
(b) “Advertisement” includes the disclosure form required pursuant to Section 1363 of the Act.
(c) (1) An “affiliate” of a person is a person controlled by, under common control with, or controlling such person.
(2) A person's relationship with another person is that of an “affiliated person” if such person is, as to such other person, a director, trustee or a member of its executive committee or other governing board or committee, or that of an officer or general partner, or holds any other position involving responsibility and authority similar to that of a principal officer or general partner; or who is the holder of 5% or more of its outstanding equity securities; or who has any such relationship with an affiliate of such person. An affiliate is also an affiliated person.
(d) The term “control” (including the terms “controlling,” “controlled by” and “under common control with”) means the possession, direct or indirect, of the power to direct or cause the direction of the management and policies of a person, whether through the ownership of voting shares, debt, by contract, or otherwise.
(e) The term “certified” or “audited,” when used in regard to financial statements, means examined and reported upon with an opinion expressed by an independent public or certified public accountant.
(f) “Code” means the California Health and Safety Code.
(g) “Copayment” means an additional fee charged to a subscriber or enrollee which is approved by the Director, provided for in the plan contract and disclosed in the evidence of coverage or the disclosure form used as the evidence of coverage.
(h) “Department” means the California Department of Managed Health Care.
(i) “Facility” means
(1) any premises owned, leased, used or operated directly or indirectly by or for the benefit of a plan or any affiliate thereof, and
(2) any premises maintained by a provider to provide services on behalf of a plan.
(j) “Family unit” means a unit composed of a subscriber and each person whose eligibility for benefits is based upon such person's relationship with, or dependency upon, such subscriber.
(k) “Hospital based plan” means a health care service plan which owns, operates or is affiliated with a hospital as an integral part of delivering health care services.
(l) “Material”: A factor is “material” with respect to a matter if it is one to which a reasonable person would attach importance in determining the action to be taken upon the matter.
(m) “Primary care physician” means a physician who has the responsibility for providing initial and primary care to patients, for maintaining the continuity of patient care, or for initiating referral for specialist care. A primary care physician may be either a physician who has limited his practice of medicine to general practice or who is a board-certified or board-eligible internist, pediatrician, obstetrician-gynecologist, or family practitioner.
(n) “Principal creditor” means
(1) a person who has loaned funds to another for the operation of such other person's business, and
(2) a person who has, directly or indirectly, 20 percent or more of the outstanding debts of a person.
(o) “Principal officer” means a president, vice-president, secretary, treasurer or chairman of the board of a corporation, a sole proprietor, the managing general partner of a partnership, or a person having similar responsibilities or functions.
(p) “Surcharge” means an additional fee which is charged to a subscriber or enrollee for a covered service but which is not approved by the Director, provided for in the plan contract and disclosed in the evidence of coverage or the disclosure form used as the evidence of coverage.
(q) The term “generally accepted accounting principles,” when used in regard to financial statements, assets, liabilities and other accounting items, means generally accepted accounting principles as used by business enterprises organized for profit. Accordingly, Financial Accounting Standards Board statements, Accounting Principles Board opinions, accounting research bulletins and other authoritative pronouncements of the accounting profession should be applied in determining generally accepted accounting principles unless such statements, opinions, bulletins and pronouncements are inapplicable. Section 510.05 of the AICPA Professional Standards, in and of itself, shall not be sufficient reason for determining inapplicability of statements, opinions, bulletins and pronouncements.
NOTE
Authority cited: Sections 1344 and 1352, Health and Safety Code. Reference: Sections 1351, 1351.1 and 1352, Health and Safety Code.
HISTORY
1. Amendment of subsection (c) filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. New subsection (q) filed 4-27-79; effective thirtieth day thereafter (Register 79, No. 17).
3. Amendment of subsection (e) filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
4. Amendment of subsection (c) filed 12-17-85; effective thirtieth day thereafter (Register 85, No. 51).
5. Change without regulatory effect amending subsections (g)-(h) and (p) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
6. Change without regulatory effect amending subsection (h) filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.46. Prohibition of Bonuses or Gratuities in Solicitations.
No person subject to the provisions of the Act shall offer or otherwise distribute any bonus or gratuity to potential subscribers for the purpose of inducing enrollment or to existing subscribers for the purpose of inducing the continuation of enrollment.
§1300.47. Advisory Committee on Managed Health Care.
Note • History
Each member of the Advisory Committee on Managed Health Care shall file with the Director a statement setting forth the following:
(a) The firm with which such member is employed or affiliated and the capacity in which employed or affiliated.
(b) Whether such firm is a health care service plan or solicitor firm under the Act or is a provider, or a fiscal intermediary for a plan, or furnishing services, goods or facilities to any plan, solicitor firm or provider.
(c) Whether such member has any financial interest in any firm specified in (b) or receives compensation from such firm.
(d) The name of each plan in which the member is enrolled, or has been enrolled during the preceding 10 years.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1347, Health and Safety Code.
HISTORY
1. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Change without regulatory effect amending section heading and first paragraph filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
3. Change without regulatory effect amending section heading and first paragraph filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
Article 3. Plan Applications and Amendments
§1300.50. Notice of Intention to Apply for Plan License.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code.
HISTORY
1. Repealer filed 6-29-84; effective thirtieth day thereafter (Register 84, No. 26).
§1300.51. Application for License as a Health Care Service Plan or Specialized Health Care Service Plan.
Note • History
(a) An application for license as a health care service plan or specialized health care service plan shall be filed in the form specified in subsection (c) and contain the information specified in this section and prepared as required by Rule 1300.51.3.
(b) Applications filed prior to the effective date of subsection (c) (revised plan application form) and which remain pending on that date will be processed; however, amendments to such applications filed prior to licensure shall be filed upon the form specified in subsection (c) in accordance with the instructions specified in Rule 1300.51.3, and in accordance with the correlation table for the old and new applications provided in Form HP 1300.51-COR. Such amendments will be required only to update the information contained in the application and to remedy deficiencies in the information provided therein.
(c) Revised Health Care Service Plan Application Form.
(d) Exhibits to Plan Application.
E. Summary of Information in Application.
1. Summary Description of Plan Organization and Operation. Provide as Exhibit E-1 a summary description of the organization and operation of applicant's business as a health care service plan, covering the highlights and essential features of the information provided in response to the other portions of this application which is essential or desirable to an effective overview of the applicant health care service plan business.
2. Summary Description of Start-up. Provide as Exhibit E-2 a concise description of applicant's start-up program and its assumptions. Indicate applicant's projected date for the beginning of plan operations, and discuss the factors which require such date.
F. Organization and Affiliated Persons.
1. Type of Organization.
a. Corporation. If applicant is a corporation, and attach as Exhibits F-1-a-i, F-1-a-ii and F-1-a-iii, respectively, the Articles of Incorporation, Bylaws, and the Corporation Information Form. (Form HP 1300.51-A)
b. Partnership. If applicant is a partnership, and attach as Exhibits F-1-b-i, and F-1-b-ii, respectively, the Partnership Agreement, and the Partnership Information Form. (Form HP 1300.51-B)
c. Sole Proprietor. If applicants a sole proprietorship, and attach as Exhibit F-1-c the Sole Proprietorship Information Form. (Form HP 1300.51-C)
d. Other Organization. If applicant is any other type of organization, and attach as Exhibit F-1-d, Articles of Association, trust agreement, or any other applicable documents, and any other organizational documents relating to the conduct of the internal affairs of the applicant, and attach as Exhibit F-1-d-ii the Information Form for other than Corporations, Partnerships, and Sole Proprietorships. (Form HP 1300.51-D)
e. Public Agency. If applicant is a public agency, and attach as Exhibit F-1-e-i a description of the public agency, its legal authority, organization, decision making body. Also attach as Exhibit F-1-e-ii a description of the division or unit of the public agency which is to be responsible for operating the plan, its legal authority, organization, and decision making role. Also attach as Exhibit F-1-e-iii the name and address of the local public agency which is the plan.
f. Individual Information Sheet. Attach as Exhibit F-1-f, an Individual Information Sheet (Form HP 1300.51.1) for each natural person named in any exhibit in Item F-1.
2. Contracts with Affiliated Persons, Principal Creditors and Providers of Administrative Services.
a. Persons to Be Identified. Attach as Exhibit F-2-a list identifying each individual or entity who is a party to a contract with applicant, if such contract is one for the provision of administrative services to the applicant or any such party is an Affiliated Person or Principal Creditor (Rule 1300.45(c) and (n)) or of the applicant. As to each such person, show the following information in columnar form:
(i) The names in alphabetical order.
(ii) The exhibit and page number of the contract (including loans and other obligations).
(iii) The type of contract of loan.
(iv) Each relationship which such individual or entity bears to the applicant (officer, director, partner, trustee, member, Principal Creditor, employee, administrative services provider, health care services provider, or shareholder).
(v) Whether (yes or no) such individual or entity is intended to become a Principal Creditor (Rule 1300.45(n)) of applicant.
(vi) Whether (yes or no) such individual or entity is intended to become an “Affiliated Person” of applicant, or to become an Affiliated Person in any capacity other than that disclosed in item F-2-a-iv.
b. Copies of Contracts. Attach as Exhibit F-2-b a copy of each contract (other than a contract for the provision of administrative services or health care services furnished pursuant to Items K or N below) identified in Item F-2-a. Preceding the first page of each such contract, attach a summary sheet which
(1) identifies the contract,
(2) specifies its terms, including its expiration date, and
(3) if a loan or obligation, specifies the unpaid balance of principal and interest and states whether applicant is in default upon the loan or obligation.
3. Other Controlling Persons. Does any individual or entity not named as a contracting party in Item F-2 or any exhibit thereto have any power, directly or indirectly, to manage, influence, or administer the operation, or to control the operations or decisions, of applicant?
If the appropriate response to this item is “yes,” attach as Exhibit F-3 a statement identifying each such person or entity and explaining fully, and summarizing every contract or other arrangement or understanding (if any) with each such person. (Each such contract should be submitted pursuant to Subsection F-2 or Subsection G-2, as appropriate.)
4. Criminal, Civil and Administrative Proceedings. Within the preceding 10 years, has the applicant, its management company, or any Affiliate of the applicant (Rule 1300.45(c)), or any controlling person, officer, director or other person occupying a principal management or supervisory position in such plan, management company or Affiliate, or any person intended to hold such a relationship or position, been convicted of or pleaded nolo contendere to a crime, or been held to have committed any act involving dishonesty, fraud or deceit in a judicial or administrative proceeding to which such person was a party?
If “yes,” attach a separate exhibit as to each such person designated Exhibit F-4, identifying such person and fully explaining the crime or act committed. Also, attach a copy of the exhibit for an individual to any Individual Information Sheet required by Item F-1-f for such individual.
5. Employment of Barred Persons. Has the plan engaged or does the plan intend to engage, as an officer, director, employee, associate, or provider, any person named in any order of the Director pursuant to Section 1386(c) or Section 1388(d) of the Act? If the appropriate response to this item is “yes,” attach as Exhibit F-5 a statement identifying each such person and explaining fully.
G. Miscellaneous.
1. Consent to Service of Process. If applicant is not a California corporation, attach as Exhibit G-1 a Consent to Service of Process, in the form required by Rule 1300.51.2.
2. Disclosure of Financial Information. Attach as Exhibit G-2, authorizations for the disclosure of financial records of the applicant, and of any association, partnership or corporation controlling, controlled by or otherwise affiliated with the applicant pursuant to Section 1351.1 of the Act. (See Items F-3 and F-5.)
HEALTH CARE DELIVERY SYSTEM
H. Geographical Area Served.
Note: The applicant is required to demonstrate that, throughout the geographic regions designated as the plan's Service Area, a comprehensive range of primary, specialty, institutional and ancillary services are readily available at reasonable times to all enrollees and, to the extent feasible, that all services are readily accessible to all enrollees.
For the purpose of evaluating the geographic aspects of availability and accessibility, consideration will be given to the actual and projected enrollment of the plan based on the residence and place of work of enrollees within and, if applicable, outside the service area, including the individual and group enrollment projections furnished in Items CC, DD and EE of this application.
An applicant for plan license must demonstrate compliance with the accessibility requirement in each of the areas specified in paragraphs (i) through (iv) below, either by demonstrating compliance with the guideline specified in such paragraphs or, in the alternative, by presenting other information demonstrating compliance with reasonable accessibility. These guidelines apply only with respect to initial license applications and provide presumptively reasonable standards in the absence of actual operating experience. Such guidelines are not intended to express minimum standards of accessibility either for applicants or for licensees nor to create any inference that a plan which does not meet these guidelines does not meet the requirement of reasonable accessibility.
(i) Primary Care Providers. All enrollees have a residence or workplace within 30 minutes or 15 miles of a contracting or plan-operated primary care provider in such numbers and distribution as to accord to all enrollees a ratio of at least one primary care provider (on a full-time equivalent basis) to each 2,000 enrollees.
(ii) Hospitals. In the case of a full-service plan, all enrollees have a residence or workplace within 30 minutes or 15 miles of a contracting or plan-operated hospital which has a capacity to serve the entire dependent enrollee population based on normal utilization, and, if separate from such hospital, a contracting or plan-operated provider of all emergency health care services.
(iii) Hospital Staff Privileges. In the case of a full-service plan, there is a complete network of contracting or plan-employed primary care physicians and specialists each of whom has admitting staff privileges with at least one contracting or plan-operated hospital equipped to provide the range of basic health care services the plan has contracted to provide.
(iv) Ancillary Services. Ancillary laboratory, pharmacy and similar services and goods dispensed by order or prescription on the primary care provider are available from contracting or plan-operated providers at locations (where enrollees are personally served) within a reasonable distance from the primary care provider.
1. Description of Service Area. As Exhibit H-1, attach a narrative description of the applicant's service area and the geographic area in which its enrollees (actual and/or projected) live and work and list all U.S. Postal ZIP Code numbers included in the service areas. If the applicant has more than one service area, each service area should be separately described. To the extent possible, service areas should be delineated by political or natural boundaries. (If applicant uses sub-service areas or regions within its service areas for the purpose of allocating the provision of health care services by providers to enrollees, include that information in the description of the considerations which underlie the geographic distribution of the applicant's contracting and plan-operated providers.)
2. Map of Service Area. As Exhibit H-2, attach a map or maps upon which the information specified below is indicated by the specified system of symbols. The map(s) employed should be of convenient size and of the largest scale sufficient to include the applicant's entire service area and the surrounding area in which the actual or projected enrollees live or work. The use of good-quality city street maps or the street and highway maps available for various metropolitan areas, and regions of the state, such as are commonly available from automobile associations or retail service stations is preferred. The map or maps should show the following information:
a. Such geographic detail, including highways and major streets, as is generally portrayed on the kinds of maps referred to above.
b. The boundaries of applicant's service area.
c. The location of any contracting or plan-operated hospital and, if separate, each contracting or plan operated emergency health care facility. Hospitals are to be designated by an “H” and emergency care facilities by an “E.”
d. The location of primary care providers, designated by a “P.” For convenience, the primary care providers within any mile-square area may be considered as being at one location within that area.
e. The location of all other contracting or plan-operated health care providers including the following: Dental, designated by a “D.” Pharmacy, designated by an “Rx.” Laboratory, designated by an “L.” Eye Care, designated by an “O.” Specialists and ancillary health care providers, designated by an “S.”
f. The location of all subscriber groups which have submitted letters of intent or interest to join the applicant's plan designated by a “G.” (See Item CC-3.)
3. Index to Map. As Exhibit H-3, attach an index to the map or maps furnished as Exhibit H-2 which shows, for each symbol placed on the map for a hospital, emergency care facility, primary care provider or ancillary provider, the following information:
a. For each hospital, its total beds and the number of beds available to enrollees of the plan.
b. For each symbol for primary care providers, the number of full-time equivalent primary care providers represented by that symbol.
c. For each interested subscriber group, the name of the group and the projected number of enrollees from that group.
I. Description of Health Care Arrangements.
Note: Providers of Health Care Services. The information in this item is for the purpose of assessing the adequacy of the applicant's health care provider arrangements.
If the service area of the plan and the distribution of its enrollees is so geographically limited that all plan health care providers are readily available and accessible to all enrollees, no geographic division of the provider information required in this part need be made.
However, if applicant's service area is divided into separate provider networks for regions within the service area, the information required in this Item-1 must be furnished separately for each such region and provider network.
1. Physicians Services.
a. Individual Physicians. As Exhibit I-1-a list all individuals who provide covered physician services as employees of the plan or, whether directly or through an association or other entity, as contracting providers: For each physician, furnish the following information.
(i) Name.
(ii) License Number.
(iii) Type of service as determined by board certification and eligibility. Primary care physicians should be designated as general practice, pediatrics, obstetrics, gynecology and internal medicine. Specialists should be designated as allergy, anesthesiology, dermatology, cardiology and other internal medicine specialists, neonatology, neurology, oncology, ophthalmology, orthopedics, pathology, psychiatry, radiology, surgeries, otolaryngology, urology, and other designated as appropriate.
(iv) The plan-owed or contracting hospitals at which the physician has admitting staff privileges.
(v) The professional address of the physician.
(vi) The physician's relationship to the plan (employed by or contracting with the plan, or contracting through an IPA or one of the parties identified in Item I-1-a.
(vii) The percentage of the physician's time allocated to enrollees of the plan.
(viii) The business hours of the physician's office (i.e., Monday through Friday 8-5, closed Wednesdays).
b. Physician Associations. For all entities other than individuals or independent practice associations who contract with applicant to provide physician services, and each plan-operated facility at which physician services are rendered by employees of the plan, as Exhibit I-1-b furnish the following information for each such contractor or facility:
(i) The name of the contractor or facility.
(ii) The street address of the contractor or facility at which the physician services are rendered for the particular region or provider network.
(iii) The type of entity (professional corporation, sole proprietor, partnership, etc.).
(iv) The number of physicians rendering services for the plan by reason of such contract or by employment at such facility, and the number of “full-time equivalent” physicians being provided to enrollees of the plan.
2. Hospitals. Attach as Exhibit I-2 a list of all hospitals which are operated by or contract with the plan. Provide the following information for each hospital:
a. Its legal name and any “dba” (fictitious name under which it does business).
b. Its address.
c. Its license number.
d. Whether it is a member of the American Hospital Association, whether it is currently accredited by the Joint Commission on the Accreditation of Hospitals, (JCAH) and the expiration date of its current accreditation.
e. Its bed capacity and rate of occupancy.
f. Its emergency room capabilities.
g. A list and full description of all services available to enrollees. Applicant may use a JCAH form or the equivalent.
h. Its relationship with applicant (owned by, contracting provider, joint venture with applicant, etc.).
3. All Other Providers of Health Care Services. Attach as Exhibit I-3 a list of all providers of health care service contracting with or owned by the applicant which are not included in the physician and hospital listings. For each such provider, furnish the following information:
a. The legal name of the provider and any “dba.”
b. Its address.
c. Its license number.
d. The health care services it provides to enrollees of the plan (e.g., home health agencies, ambulance company, laboratory, pharmacy, skilled nursing facility, surgi-center, mental health, family planning, etc.).
e. Its hours of operation and the provision made for after-hours service.
f. An appropriate measure of the provider's capacity to provide health care service, the existing utilization of such services by other than enrollees of the plan and the projected use of the services by enrollees.
g. The provider's relationship to the plan (owned by, contracting with, etc.).
4. Calculation of Provider-Enrollee Ratios. As Exhibit I-4, furnish a calculation of the adequacy of the applicant's provider arrangements for each region or provider network within applicant's service area. This should be based on the full range of the health care services covered by the applicant's full-service or specialized plan contracts, the extent to which contracting and planned-owned or employed providers are available to provide such services, the enrollee population served by such providers and the adequacy of the provider system in each category based on standard utilization data. Assumptions employed in such calculations should be stated, including the extent to which paraprofessionals and allied health personnel will be used by applicant or providers and the protocols and method of supervision of such personnel.
5. Applicant's Standards of Accessibility. Attach as Exhibit I-5 a detailed description of the applicant's standards with respect to the accessibility and its procedures for monitoring the accessibility of services. Standards should be expressed in terms of the level of accessibility which the applicant has as its objective and the minimum level of accessibility below which corrective action will be taken. Cover each of the following:
a. the availability of appointments for primary care and specialty services,
b. the availability of after hours and emergency services,
c. an assessment of probable patient waiting times for scheduled appointments,
d. the proximity of specialists, hospitals, etc. to sources of primary care, and
e. a description of applicant's system for monitoring and evaluating accessibility. (Discuss applicant's system for monitoring problems that develop, including telephone inaccessibility, delayed appointment dates, waiting time for appointments, other barriers to accessibility, and any problems or dissatisfaction identified through complaints from contracting providers or grievances from subscribers or enrollees.)
f. the contractual arrangements utilized by the applicant to assure the monitoring of accessibility and conformance to standards of accessibility by contracting providers.
6. Referrals. Attach as Exhibit I-6 a detailed description of applicant's system of documentation of referrals to physicians or other health professionals. Include:
a. the provisions made for written documentation of the referral policies and procedures,
b. the procedures for following up on contracting and noncontracting referrals, including turnaround times, and
c. applicant's arrangements for paying for services delivered by noncontracting providers.
J. Internal Quality of Care Review System.
Applicant is required to demonstrate that it has a system for the review of the quality of health care to identify, evaluate and remedy problems relating to access, continuity and quality of care, utilization and the cost of services. The following exhibits require a description and explanation of the system, including narrative, organization and process charts and review criteria. See Rule 1300.70.
1. Organization and Operation. As Exhibit J-1, furnish a description of the basic structure, organization and authority of the applicant's quality of care review system, including:
a. An organization chart showing the key persons, the committees and bodies responsible for the conduct of the review system, the provisions for support staff and the relationship of such persons, committees and bodies to the general organization of the plan. See Item J-4 below.
b. A narrative explanation of the review system covering the matters depicted in the organization chart and the following: the key persons involved, their titles and their qualification; the extent and type of support staff; the areas of authority and responsibility of the key persons and the committees, if divided among persons and committees; the frequency of meetings of the committees and the portion of their time devoted to the review system by key persons. See Item J-4 below.
2. Standards and Norms. Attach as Exhibit J-2 a description of the standards and norms of the system (including any measurement of deviation in their application), and indicate how these standards and norms will be communicated to providers.
3. Operation of System. Attach as Exhibit J-3 a description of the operation of the review system, including the frequency and scope of audits, the utilization of the audit results and the procedures and methods for the enforcement of the standard and norms of the system.
4. Administration of System by Providers. If portions of the review system are administered by contracting providers, by affiliates of the applicant or by other persons who are not officers or employees of the applicant, attach Exhibit J-4 identifying those portions of the system together with the providers, affiliates or persons administering them on behalf of the applicant, and describe and furnish copies of the contractual provisions which assure the maintenance of the system to the standards of the applicant and those of the Act and the rules thereunder.
5. Monitoring of Provider Administration. Attach as Exhibit J-5, a description of the contractual arrangements which will be employed to enable the plan to monitor, and require, compliance with the quality of care review system, to the extend such system is administered by such contracting providers.
K. Contracts with Providers.
1. Copies of Contracts. Attach as Exhibit K-1 a copy of each contract made, or to be made, between applicant and each provider of health care services. If a contract shows the payment to be rendered a provider, delete such minimum portion of the contract as is necessary to prevent disclosure of such information, by blanking out or other suitable means.
a. If standard form contracts are used, only a specimen of each type of form contract need be filed together with any variations to be used in the terms and provisions of such standard forms, other than in the amount of payments to providers.
b. The contracts and other information submitted in this exhibit will be available for public inspection (see Section 1351(d)).
2. Compliance with Requirements. Attach as Exhibit K-2 a statement in tabular form for each provider contract, and for each standard form contract and its variations, if any, specifying the provisions of such contract which comply with the following provisions of the act and rules:
Section 1379
Rule 1300.67.1(a) and (c)
Rule 1300.67.2(b), (c) and (f)
Rule 1300.67.4(a)(9) and (10)
Rule 1300.67.8(a), (b), (c) and (d)
Rule 1300.68
Rule 1300.70
Rule 1300.51, Item J-5
3. Compensation of Health Care Providers. Attach as Exhibit K-3 one copy of the following provisions from each provider contract, or proposed provider contract, from which payment information was deleted in Exhibit K-1 and clearly mark the extracts from each contract “confidential”:
a. The title page of the contract or other information sufficient to identify the contract submitted as Exhibit K-1 to which the extract relates and the providers who are parties.
b. The effective date of the contract and its expiration date.
c. The provisions describing the mechanism by which payments are to be rendered to the provider, including any risk sharing arrangement, clearly identified by the name of the provider.
d. The provider's signature on the execution page of the contract, with the name of the provider typed beneath the signature.
ADMINISTRATION OF THE PLAN
L. Organization Chart.
Attach as Exhibit L an organization chart which shows the lines of responsibility and authority in the administration of the applicant's business as a health care service plan. One chart should be limited to the applicant itself, showing its management and operational structure, including the names and titles of key positions and its board. If necessary, a second chart should show the total management structure of the business in all areas, and including the key positions and departments of the applicant and those in any affiliate and/or contracting provider of health care and/or administrative services, including but not limited to the particular management functions required in the administration of a health care delivery system. The charts are to show the names of the corporations, partnerships and other entities involved in such administration, their boards, committees, and key management positions involved, giving the names of the boards, committees and positions and the persons serving therein.
M. Narrative Information.
1. Attach as Exhibit M-1 a narrative explanation of the organization chart, including the responsibility and authority of each entity, board, committee and position and identifying the persons who serve on such boards and committees and in such positions.
2. Attach as Exhibit M-2, a statement as to each individual who is a member of a board or committee or who occupies a position specified in Exhibit L and Exhibit M-1, covering the following:
a. Name.
b. Each position (e.g., director, officer, committee member, key management personnel and the managers of key departments) such person holds which is indicated in Exhibits L and M-1, whether with applicant, an affiliate or a contracting provider of health, administrative or other services. Also state the person's principal responsibilities and authority in each position, and the portion of the individual's time devoted to each principal function.
c. A resume or similar description of such person's training and experience during the preceding five years (or longer, if desired) which are relevant to the duties and responsibility in applicant's business as a health care service plan.
N. Contracts for Administrative Services.
1. As Exhibit N-1, attach a copy of each contract which applicant has for administrative or management services, or consulting contracts, or which applicant intends to have for the Health Plan.
2. As Exhibit N-2, describe applicant's administrative arrangements to monitor the proper performance of such contracts and the provisions which are included in them to protect applicant, its plan business and its enrollees and providers in the event there is a failure of performance or the contract is terminated.
O. Attach as Exhibit O a statement describing how the Health Plan organization will provide for separation of medical services from fiscal and administrative management to assure that medical decisions will not be unduly influenced by fiscal and administrative management. Describe what controls will be put into place to assure compliance with this requirement. Refer to appropriate items in Exhibit “J,” Internal Quality of Care Review System.
SUBSCRIBER CONTRACTS, DISCLOSURES, AND RELATIONS
Note: In Items P and Q, the applicant is required to include as exhibits copies of the health care service contracts it will issue, including standard form contracts and any variations in the provisions of those forms. In addition, the applicant is required to identify the particular provisions of these contracts which comply with the provisions of the Act and rules listed at the end of this note, or which vary from those provisions. The applicant is also required to explain its proposed variations (if any) from the Act or rules, giving the reasons and justifications for such variances.
The provisions of the Act and rules required to be covered in the information furnished pursuant to Items P and Q are the following:
All Plan Contracts
Section 1345 (definitions)
Section 1362 (definitions)
Section 1363 (only if used for evidence of coverage)
Section 1365
Section 1367.6
Section 1367.8
Section 1373
Section 1373.4
Rule 1300.45 (definitions)
Rule 1300.63(a) (only if used as evidence of coverage)
Rule 1300.63.1 (only if used as evidence of coverage)
Rule 1300.63.2 (only if used as evidence of coverage)
Rule 1300.67.4
Rule 1300.68(b)
Group Contracts Only
Section 1367.2
Section 1367.3
Section 1367.5
Section 1367.7
Section 1373.1
Section 1373.2
Section 1373.5
Section 1373.6
Section 1374
Section 1374.10
P. Group Health Care Service Plan Contracts.
1. Copies of Contracts. Attach as Exhibit P-1 a copy of each group contract which is to be issued by applicant. With respect to contracts based on a standard form, only a specimen of each standard form need be submitted, accompanied by Exhibit P-2.
2. Variations in Standard Form. Attach as Exhibit P-2, if applicant uses standard form group contracts, a schedule or explanation of the variations which will be made in the terms and provisions of such contracts when issued. If no variations will be made, so state.
3. Compliance with Requirements. Attach as Exhibit P-3 a schedule in tabular form for each group contract and each standard form group contract, identifying the particular provision of such contract which complies with each relevant provision of the Act and the rules listed in the preface note to this part, covering also any variations made in standard form contracts. As to any provision which varies from the applicable provision of the Act or rules, identify such provision in Exhibit P-3 and furnish Exhibit P-4.
4. Variance with Requirements. As Exhibit P-4, attach a statement with respect to each variance which the applicant proposes to make from the Act or rules in its group contracts, indicating the reasons for the variance and, if applicable, the circumstances under which the variance from the Act or rules is proposed to be used.
Q. Individual Health Care Service Plan Contracts.
1. Copies of Contracts. Attach as Exhibit Q-1 a copy of each individual contract which is to be issued by applicant. With respect to contracts based on a standard form, only a specimen of each standard form need be submitted, accompanied by Exhibit Q-2.
2. Variations in Standard Form. Attach as Exhibit Q-2, if applicant uses standard from individual contracts, a schedule or explanation of the variations which will be made in the terms and provisions of such contracts when issued. If no variations will be made from the standard form, so state.
3. Compliance with Requirements. Attach as Exhibit Q-3 a schedule in tabular form for such individual contract and each standard form individual contract, identifying the particular provision of such contract which complies with each relevant provision of the Act and rules listed in the preface note to this part, covering also any variations to be made in standard form contracts. As to any provision which varies from the applicable provision of the Act or rules, identify such provision in Exhibit Q-3 and furnish Exhibit Q-4.
4. Variance from Requirements. As Exhibit Q-4, attach a statement with respect to each variance which the applicant proposes to make from the Act or rules in its individual plan contracts, indicating the reasons for the variance and, if applicable, the circumstances under which the variance from the Act or rules is proposed to be used.
R. (Reserved for future use.)
S. Disclosure Forms.
1. Attach as Exhibit S-1 a copy of each disclosure form which applicant proposes to use, and identify by name and by exhibit number the contract or contracts in Exhibit P-1 or Q-1 with which the disclosure form will be used. If the disclosure forms vary in text, format and arrangement in a manner which may make it difficult to identify and compare alternatives and their effect upon the contract, include an explanation which indicates how such difficulties will be avoided.
2. Attach as Exhibit S-2 a statement in tabular form for each disclosure form submitted as Exhibit S-1 above, identifying the section, paragraph, or page number of the disclosure form which shows compliance with each of the following sections of the Act or rules (following the parenthetical instructions set forth in the note immediately preceding Item P above, if there are multiple disclosure forms):
Section 1345 (definitions)
Section 1362 (definitions)
Section 1363(a)(1) through (8)
Section 1363(a)(10)
Section 1378(g) (if disclosing group contract)
Rule 1300.67(a)(1)
Rule 1300.63(b)(1) through (14)
T. Evidence of Coverage.
1. Attach as Exhibit T-1 a copy of each evidence of coverage which applicant proposes to use. Each evidence of coverage should relate to one form of plan contract which must be identified by name and by exhibit number; however, an evidence of coverage for alternative plans or options will be permitted if presented in a manner which clearly identifies the alternatives and their effect upon the contract and if the alternative contracts are clearly identified by name or exhibit number.
2. Attach as Exhibit T-2 a statement in tabular form for each evidence of coverage submitted as Exhibit T-1 above, the section, paragraph, or page number of the evidence of coverage which shows compliance with each of the following sections of the Act or rules (following the parenthetical instructions set forth in the note immediately preceding Item P above, if there are multiple evidences of coverage):
Section 1345 (definitions)
Section 1362 (definitions)
Rule 1300.63(a)(1)
Rule 1300.63.1(b)(1) and (2)
Rule 1300.62.2(b)(1) and (2)
Rule 1300.63.2(c)(1) through (16)
Rule 1300.69(i)
U. Combined Evidence of Coverage and Disclosure Forms.
Applicant may combine the evidence of coverage and disclosure form into one document if it complies with each of the requirements set forth in Rule 1300.63.2.
1. Attach as Exhibit U-1 a copy of each combined evidence of coverage and disclosure form. Each combined evidence of coverage and disclosure form should relate to one form of plan contract; however, a combined evidence of coverage and disclosure form offering alternative plans or options will be permitted if presented in a manner which clearly identifies the alternatives and their effect upon the contract.
2. Attach as Exhibit U-2 a statement in tabular form for each combined evidence of coverage and disclosure form submitted as Exhibit U-1 above, the section, paragraph or page number which shows compliance with each of the following sections of the Act or Rules (following the parenthetical instructions set forth in the note immediately preceding Item P above, if there are multiple combined evidences of coverage and disclosure forms):
Section 1345 (definitions)
Section 1362 (definitions)
Rule 1300.63.2(b)(1) and (2)
Rule 1300.63.2(c)(1) through (27)
Rule 1300.69(i)
V. Advertising.
Attach as Exhibit V a copy of any advertising which is subject to Section 1361 of the Act and which applicant proposes to use. With respect to each proposed advertisement indicate the contract(s) by name and by exhibit number(s) to which said advertisement relates and identify the segment of the public to which the advertisement is directed.
W. Enrollee/Subscriber Grievance Procedures.
1. Attach as Exhibit W-1 a copy of its written grievance procedure adopted or to be adopted by applicant to comply with all of the provisions of Section 1368 of the Act and Rules 1300.68, 1300.85 and 1300.85.1.
2. Attach as Exhibit W-2, copies of the compliant forms and the written explanation of its grievance procedure which the plan will make available to enrollees and subscribers.
3. If the written procedure furnished as Exhibit W-1 does not identify the key personnel of applicant and provider organizations that will be responsible for carrying out its grievance procedures and the review of its results, attach Exhibit W-3 giving the name and title of each such person and identifying their responsibility for carrying out the procedure.
X. Public Policy Participation.
1. If applicant is in compliance with the requirements of the Federal Health Maintenance Organization Act of 1973 and intends to rely on such compliance to satisfy the provisions of Section 1369 of the Act, attach as Exhibit X-1 documentation necessary to validate compliance with the Health Maintenance Organization Act.
2. Unless applicant has satisfied the provisions of Section 1369 of the Act in the manner indicated in Subsection X-1, above, attach as Exhibit X-2 a description of applicant's procedures to permit subscribers and enrollees to participate in establishing the public policy of the plan, including at least the following:
a. the composition of applicant's governing board,
b. the composition of the standing committee established which shall participate in establishing the public policy of the plan as defined in Section 1369 of the Act, the frequency of said committee's meetings, the frequency of receipt by applicant's governing body of said committee's reports and recommendations, and the procedures established by the governing body for dealing with such reports and recommendations;
c. the means by which subscribers and enrollees participating in established public policy will be given access to information and information regarding the specific nature and volume of complaints received by applicant and their disposition;
d. specific identification by name and section or paragraph number of pertinent provisions of applicant's bylaws and/or other governing documents (as submitted in response to Item F) which set forth the procedures for public policy participation for subscribers and enrollees; and
e. the manner and frequency with which applicant will furnish to its subscribers and enrollees a description of its system for their participation in establishing public policy and communicate material changes affecting public policy to subscribers and enrollees.
MARKETING OF PLAN CONTRACTS
Y. Marketing of Group Contracts.
Attach as Exhibit Y a statement describing the methods by which applicant proposes to market group contracts, including the use of employee or contracting solicitors or solicitor firms, their method or form of compensation and the methods by which applicant will obtain compliance with Rules 1300.59, 1300.61, 1300.76.2, and 1300.85.1.
Z. Marketing of Individual Contracts.
Attach as Exhibit Z a statement describing the methods by which applicant proposes to market individual plan contracts, including the use of employee or contracting solicitors or solicitor firms, their method or form of compensation and the methods by which applicant will obtain compliance with Rules 1300.59, 1300.61, 1300.76.2, and 1300.85.1.
AA. Supervision of Marketing.
Attach as Exhibit AA a statement setting forth applicant's internal arrangements to supervise the marketing of its plan contracts, including the name and title of each person who has primary management responsibility for the employment and qualification of solicitors, advertising, contracts with solicitors and solicitor firms and for monitoring and supervising compliance with contractual and regulatory provisions.
BB. Solicitation Contracts.
1. Attach as Exhibit BB-1 a list of all persons (other than any employee of the plan whose only compensation is by salary) soliciting or agreeing to solicit the sale of plan contracts on behalf of the applicant. For each such person, identify by exhibit number that person's contract furnished pursuant to Item BB-2 and, if such contract does not show the rate of compensation to be paid, specify the person's rate of compensation.
2. Attach as Exhibit BB-2, a copy of each contract or proposed contract between applicant and the persons named in Exhibit BB-1 for soliciting the sale of or selling plan contracts on behalf of applicant. If a standard form contract is used, furnish a specimen of the form, identify the provision and terms of the form which may be varied and include a copy of each variation.
3. If the rate of compensation for any solicitor or for any plan contract exceeds 5 percent of the prepaid or periodic charge for the contract(s) on an annual basis, attach as Exhibit BB-3 a statement explaining and justifying the rate of compensation in each such case.
CC. Group Contract Enrollment Projections.
Note: All projections required by Items CC, DD, EE and HH are to cover the period commencing from its commencement of operations as a licensed health care service plan until the applicant's financial statement projections under Item HH demonstrate that it has reached the break-even point (or for one year, whichever is longer) and for an additional period of one year thereafter. For the initial period, all projections are to be on a monthly basis. For the additional year, all projections are to be on a quarterly basis.
1. Projections. Attach as Exhibit CC-1 projections of applicant's enrollments under group contracts for the periods specified in the above note. (Medi-Cal, Medicare, and Medicare supplemental programs are to be treated as individual contracts under Item DD below.) Exhibit CC-1 is to contain the following information with respect to each anticipated group contract:
a. The name of the group.
b. The number of potential subscribers in the group.
c. The locations within and around applicant's service area in which the potential subscribers and enrollees live and work.
d. The estimated date (or period after licensing) for entry into the group contract.
e. Identification of the plan contract anticipated with the group, by reference to Exhibit P-1. If more than one type of group contract is expected with a group, each contract must be covered separately.
f. The projected number of (1) subscribers and (2) enrollees (including subscribers), on a monthly basis for the initial period specified in the above note and quarterly for the following year.
g. State whether the contract will be “community rated” or “experience rated.”
h. Evaluation of the competition for each group.
2. Substantiation of Projections. Attach as Exhibit CC-2 for each group contract specified in Exhibit CC-1 a description of the facts and assumptions used in connection with the information specified in that exhibit and include documentation of the source and validity of such facts and assumptions.
3. Letters of Interest. Attach as Exhibit CC-3 letters of interest or intent from each group listed in Exhibit CC-1, on the letterhead of the group and signed by its representative.
DD. Individual Contract Enrollment Projections.
1. Projections. Attach as Exhibit DD-1 a projection of applicant's sales of individual contracts for the periods specified in the note in Item CC above. Programs involving Medi-Cal, Medicare and Medicare supplemental coverages are to be treated as individual contracts. The exhibit is to contain the following information as to each type of individual contract:
a. A description (e.g., ethnic, demographic, economic, etc.) of each target population.
b. The estimated number of persons in each target population.
c. The distribution of the target population within and around applicant's service area.
d. The projected number of (1) subscribers and (2) enrollees (including subscribers) expected to be obtained from each target population, on a monthly basis for the initial period and quarterly for the following year.
e. State whether the contract will be “community rated” or “experience rated.”
f. Evaluation of the competition within the target area.
2. Substantiation of Projections. Attach as Exhibit DD-2 a statement of the facts and assumptions employed with respect to the information furnished for each contract and target population listed in Exhibit DD-1 and furnish documentation, including reliable market surveys, validating the facts and assumptions.
EE. Summary Enrollment Projections.
Attach as Exhibit EE summary enrollment projections on a monthly basis for the initial period specified in the note to Item CC and on a quarterly basis for the following year. Such enrollment projections should reflect the breakdown of enrollment by groups, individuals, Medi-Cal, Medicare, and others.
FF. Prepaid and Periodic Charges.
1. Determination of Prepaid Charges. Attach as Exhibit FF-1, a description of the method used by applicant to determine the prepaid or periodic charges fixed for individual and group contracts, including the method by which administrative and other indirect costs are allocated. Describe the facts and assumptions upon which such charges are based (e.g., contract mix, family size) and furnish supporting documentation to substantiate the validity of the facts and assumptions used.
2. Schedule of Prepaid Charges. Attach as Exhibit FF-2-a complete schedule of the prepaid or periodic charges assessed subscribers under each group contract identified in response to Item P and attach as Exhibit FF-2-b a schedule of the prepaid or periodic charges assessed subscribers under each individual contract identified in response to Item Q.
3. Collection of Prepaid Charges. Attach as Exhibit FF-3 a description of the manner in which applicant will collect prepaid and periodic charges and copayments from subscribers and enrollees under its group and individual contracts. If prepaid or periodic charges will be paid by subscribers to an entity other than the plan, identify the entity and specify the measures used by the plan to safeguard and account for such funds (see Rules 1300.76.2, 1300.85 and 1300.85.1).
FINANCIAL VIABILITY
GG. Current Financial Viability, Including Tangible Net Equity.
1. Financial Statements.
a. Attach as Exhibit GG-1-a the most recent audited financial statements of applicant, accompanied by a report, certificate, or opinion of an independent certified public accountant or independent public accountant, together with all footnotes to said financial statements.
b. If the financial statements attached as Exhibit GG-1-a are for a period ended more than 60 days before the date of filing of this application, also attach as Exhibit GG-1-b financial statements prepared as of date no later than 60 days prior to the filing of this application consisting of at least a balance sheet, a statement of income and expenses, and any accompanying footnotes; these more recent financial statements need not be audited, so long as they are prepared in accordance with generally accepted accounting principles.
2. Tangible Net Equity. Attach as Exhibit GG-2 a calculation of applicant's tangible net equity in accordance with Rule 1300.76, based on the most recent balance sheet submitted as Exhibit GG-1-a or b above.
HH. Projected Financial Viability
1. Attach as Exhibit HH-1, the following projected financial statements of the applicant reflecting actual and projected changes which have, or which are expected to occur between the date of its most recent financial statements furnished pursuant to Item GG and the date specified for the commencement of its operations as a plan in Item E above. The projected financial statements must be prepared in accordance with generally accepted accounting principles and on a basis consistent with the financial statements supplied in Item GG.
a. Applicant's projected balance sheet as of the start up date of the plan. (See Item E)
b. Applicant's projected statement of income and expenses covering the period between the date of the most recent financial statements furnished in Item GG and the date specified in Item E.
c. A calculation of applicant's projected tangible net equity in accordance with Rule 1300.76 as of the date specified in Item E and in accordance with its projected balance sheet.
2. Attach as Exhibit HH-2, projected financial statements as of the close of each month during applicant's initial period of operations, as defined in the note to Item CC, and as of the close of each quarter for the following year, prepared on a consistent basis with the financial statements furnished for Item HH-1, including the following:
a. Applicant's projected balance sheet as of the close of such month or quarter.
b. Applicant's projected statement of income and expense for such month or quarter.
c. Applicant's projected cash-flow statement for such month or quarter.
d. A calculation of applicant's tangible net equity pursuant to Rule 1300.76 as of such month or quarter.
e. A calculation of applicant's administrative costs pursuant to Rule 1300.78 for such month or quarter.
3. Furnish the following information to substantiate the assumptions and conclusions upon which the projections required by Items HH-1 and HH-2 are based:
a. Attach as Exhibit HH-3-a the complete results of feasibility studies obtained by applicant as normally required by conventional lending institutions, including at least the following: legal, marketing/enrollment, providers and financial.
b. Attach as Exhibit HH-3-b an actuarial report which includes at least the following information for all enrollees reflected in Exhibit EE as covered by contracts which are community rated:
(i) Utilization rates for each medical expense item reflected in applicant's income statements furnished pursuant to Item HH-2, expressed in terms of utilization units per member per month, including the methodology and source of data used to determine such rates.
(ii) The cost per utilization unit for each medical expense item reflected in the income statement, including the methodology and source of data used to determine such costs.
(iii) The per member per month cost for each medical expense item.
(iv) The methodology and source of data used to estimate copayments, coordination of benefits, and reinsurance recoveries, including the expression of such items on a per member per month basis.
(v) Inflation estimates used in the projections and the source utilized to determine such estimates.
c. For each contract which is designated as experience rated (as summarized in Exhibit EE) attach as Exhibit HH-3-c an actuarial report for the contract which conforms to the requirements stated in Item HH-3-b.
d. Attach as Exhibit HH-3-d a summary schedule which reflects the breakdown of the total revenue and expense included in the projected income statements in Exhibit HH-2-b by community rated contacts and experience rated contracts.
e. As Exhibit HH-3-e the assumptions made by the applicant to determine the time lag between the delivery by covered health care services and applicant's payment for those services. Also indicate all other assumptions made in preparing the projected cash flow statements in Item HH-2-c.
f. Attach as Exhibit HH-3-f-i a detailed description of any measures taken or proposed to be taken by applicant to maintain compliance with the tangible net equity requirement under Rule 1300.76 and the financial viability requirement under Rule 1300.76.1 in view of losses and expenditures prior to reaching a break-even point in its operations. This information should include a schedule setting forth the amounts of any additional needed funding and the dates when such amounts will be infused into applicant. If such arrangements involve arrangements for additional capital, to subordinate or postpone the payment of accounts, notes or other obligations of the plan or other agreements, cite the exhibit numbers of such agreements and identify their applicable provisions, if supplied elsewhere in the application, or if not otherwise furnished, attach copies of such agreements or proposed agreements, identifying the parties thereto and their relationship to the plan and its affiliates.
If any funding is to be obtained from an entity other than a national bank or a bank incorporated under the laws of this state, attach as Exhibit HH-3-f-ii a copy of such entity's most recent annual audited and quarterly unaudited financial statements.
4. Reimbursements. Attach as Exhibit HH-4 the following information regarding applicant's projected reimbursements:
a. Monthly and quarterly projections as specified in the note to Item CC for each of the following (see instruction in Item 4-b):
(i) Payments to reimburse noncontracting providers for covered health care services furnished to enrollees (see Section 1377(a)).
(ii) Payments to reimburse enrollees for covered health care services furnished by noncontracting providers (see Section 1377(a)).
(iii) Total reimbursements for services by noncontracting providers (1) plus (2) (see Section 1377(a)).
(iv) Fee-for-service payments to reimburse contracting providers for covered health care services.
(v) Total reimbursements (3) plus (4).
(vi) Total expenditures by applicant for covered health care services.
(vii) The ratio of total reimbursements to total health care expenditures (5) divided by (6).
(viii) The ratio of reimbursements for services by noncontracting providers to total expenditures (3) divided by (6).
b. Describe and substantiate the facts and assumptions upon which the projections are based, including those for fee-for-service payments to contracting providers and document the source and validity of such assumptions. (Actuarial studies or comparable information should be furnished in response to these items.)
c. If the ratio of total reimbursements to total expenditures in Item 4-a (viii) exceeds 10%, specify the measures by which applicant will comply with Section 1377(a) of the Act and Rules 1300.77 and 1300.77.3. If applicant will maintain reserves as specified in Section 1377(a)(1) of the Act, specify the size of the reserve and the fiscal impact upon applicant arising from its maintenance.
d. If the ratio of total reimbursements to total expenditures in Item 4-a(vii) exceeds 10%, specify the measures by which applicant will comply with Section 1377(b) of the Act and Rules 1300.77.1, 1300.77.2 and 1300.77.3.
5. Administrative Costs. If applicant's administrative costs (as defined in Rule 1300.78) as projected for its initial period of operation (as specified in the Note to Item CC and calculated pursuant to Item HH-2-e) exceed 25% of the prepaid or periodic charges paid by or on behalf of subscribers, and if such administrative costs exceed 20% of such charges for the following year, attach as Exhibit HH-5 a calculation of the percentage of administrative costs to such charges for both such periods and furnish information which explains the necessity for the level of administrative costs projected and the manner in which applicant will reduce such costs to not more than 15% of such charges within five years after licensure.
6. Provision for Extraordinary Losses. The following requirements require an initial applicant to submit legible copies of the actual policies of insurance (including any riders or endorsements) or specimen copies of the policies of insurance which show all of the terms and conditions of coverage, or with respect to those items expressly allowing for self-insurance, allow applicant to provide evidence of self-insurance at least as adequate as insurance coverage.
a. Attach as Exhibit HH-6-a evidence of adequate insurance coverage or self-insurance to respond to claims for damages arising out of furnishing health care services (malpractice insurance).
b. Attach as Exhibit HH-6-b evidence of adequate insurance coverage or self-insurance to respond to claims for tort claims, other than with respect to claims for damages arising out of furnishing health care services.
c. Attach as Exhibit HH-6-c evidence of adequate insurance coverage or self-insurance to protect applicant against losses of facilities upon which it has the risk of loss due to fire or other causes. Identify facilities covered by individual policies and indicate the basis upon which applicant believes that the insurance thereon is adequate.
d. Attach as Exhibit HH-6-d, evidence of fidelity bond coverage for at least the amounts specified in Rule 1300.76.3, in the form of a primary commercial blanket bond or a blanket position bond written by an insurer licensed by the California Insurance Commissioner, providing 30 days' notice to the Director of the Department of Managed Health Care prior to cancellation, and covering each officer, director, trustee, partner and employee of the plan, whether or not compensated.
e. Attach as Exhibit HH-6-e evidence of adequate workmen's compensation insurance coverage against claims which may arise against applicant.
II. Fiscal Arrangements.
1. Maintenance of Financial Viability. Attach as Exhibit II-1 a statement describing applicant's arrangements to comply with Section 1375.1(b) of the Act and Rule 1300.75.1(a)(2). If applicant will maintain insurance under these provisions, furnish a specimen of the policy, the name of the insurer and the premium cost to the policy.
2. Capitation Payments to Providers. If applicant intends to pay some or all providers on a capitation basis, attach as Exhibit II-2 a statement indicating the percentage of contracting providers who will be compensated on that basis, a description of the method used to determine and adjust the capitation rates, and substantiate by means of calculations or other information that such capitation rates are adequate to reasonably assure the continuance of the applicant/provider relationship.
3. Risk of Insolvency. Attach as Exhibit II-3 a description of the manner in which applicant will provide for each of the following in the event of applicant's insolvency:
a. The continuance of benefits to enrollees for the duration of the contract period for which payment has been made.
b. The continuance of benefits to enrollees until their discharge, for those enrollees confined in an in-patient health care facility on the date of insolvency.
c. Payments to noncontracting providers for services rendered.
4. Provider Claims. Attach as Exhibit II-4 a statement describing applicant's system for processing claims from contracting providers and noncontracting providers for payment, and from subscribers and enrollees for reimbursement, including, the rules defining applicant's obligation to reimburse, the standards and procedures for applicant's claims processing system (including receipt, identification, handling, screening, and payment of claims), the timetable for processing claims, procedures for monitoring the claims processing system, and procedures for reviewing the claims processing system in view of complaint from contracting or noncontracting providers or grievances from subscribers or enrollees. The records maintained regarding fee-for-service reimbursements must be in accordance with the provisions of Rule 1300.77.4.
5. Other Business. If the applicant is or will engage in any business other than as a health care service plan, attach as Exhibit II-5 a statement describing such other business, its relationship to applicant's business as a plan, and the anticipated financial risks and liabilities of such other business. If the financial statements and projections in Exhibits GG-1-a, GG-1-bb, HH-1 and HH-2 do not include such other business, explain.
(e) Information Forms Required by Item F-1 of Subsection (d):
(1) Corporation Information Form.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1351, 1351.1, 1352, 1359, 1363, 1367, 1367.2, 1367.3, 1367.4, 1367.5, 1367.6, 1367.7, 1367.8, 1367.9, 1367.15, 1368, 1369, 1370, 1370.1, 1373, 1373.1, 1373.2, 1373.4, 1373.5, 1373.6, 1373.7, 1373.8, 1374, 1374.7, 1374.10, 1374.11, 1374.12, 1375.1, 1376, 1378, 1386, 1399.62 and 1399.63, Health and Safety Code.
HISTORY
1. Amendment of Item 23-C filed 12-20-77 as an emergency; effective upon filing (Register 77, No. 52).
2. Amendment filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
3. Amendment of Item 23 filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
4. Amendment of Item 22-G filed 6-29-84; effective thirtieth day thereafter (Register 84, No. 26).
5. Amendment filed 12-17-85; effective thirtieth day thereafter (Register 85, No. 51).
6. Change without regulatory effect amending subsection (c) filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
7. Change without regulatory effect amending subsections (c), (d)F.5., (d)HH.6.d., (e)(1), (e)(2), (e)(3) and (e)(4) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
8. Change without regulatory effect amending subsection (d)HH.6.d., (e)(1)-(4)(forms), filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
9. Amendment of subsection (c) filed 10-26-2004; operative 11-25-2004 (Register 2004, No. 44).
§1300.51.1. Individual Information Sheet.
Note • History
An individual information sheet required pursuant to these rules shall be in the following form:
CONFIDENTIAL
See Note to Item 5
DEPARTMENT OF MANAGED HEALTH CARE
State of California
INDIVIDUAL INFORMATION SHEET
under the
Knox-Keene Health Care Service Plan Act of 1975
(California Health & Safety Code Sec. 1340 et. seq.)
1. Name of Applicant: File No. ____________________
________________________________________
2. Exact full name of person completing this statement:
First Middle Last
3. Physical Description:
Sex______Hair______Eyes_______Height_______Weight______
4. Birthdate: __________________ Birthplace:__________________________
5. Social Security No. or
Taxpayer Ident. No:
NOTE: The inclusion of your social security number is not required but is voluntary. It is solicited pursuant to Sections 1344 and 1351 of the Health and Safety Code. It may be used to conduct a background investigation by the Department, the California Department of Justice Information Branch, or by other federal, state or local law enforcement agencies. This form, including the social security number, will be held confidential, but is a public record and available to the public pursuant to the Public Records Act (Gov. Code Section 6250), at the discretion of the Director.
6. Residence Telephone: 7. Business Telephone:
8. Current Residence Address:
Number and Street City State Zip
9. Employment for the last 5 years (list most recent first and include any employment with a plan or any person or entity which is or was affiliated with a plan (Section 1300.45(c)):
From to Present Employer Name and Address Occupation and Duties
NOTE: Attach separate schedule if space is not adequate.
10. Business contacts, dealings and affiliations (see section 1300.45(c)(2)) with health care service plans during the last 5 years (but including, for example, such roles as director, stockholder, consultant, manager, provider and supplier, and such dealings as sales, leasing, and any contractual relationships) (list most recent business contacts and dealings first):
From to Present Plan Name and Address Relationship and Duties
NOTE: Attach separate schedule if space is not adequate.
11. Have you ever had a certificate, license, permit registration or exemption issued pursuant to the Business and Professions Code or Health and Safety Code denied, revoked or suspended or been otherwise subject to disciplinary action, while you were in the employ of the applicant, or while you had a contract with the applicant as a provider or otherwise? [ ] Yes [ ] No
If “yes” state the date of the action and the administrative body taking such action.
12. Have you ever been convicted or pled nolo contendere to a misdemeanor involving moral turpitude or any felony, other than traffic violations?
[ ] Yes [ ] No
If the answer is “yes” give details:
13. Have you ever changed your name or ever been known by any name other than that herein listed? (Including a married person's prior surname, if any.)
[ ] Yes [ ] No
If so, explain. Change in name through marriage or court order should also be listed.
EXACT DATE OF EACH NAME CHANGE MUST BE LISTED.
14. Have you ever engaged in business under a fictitious firm name either as an individual or in the partnership or corporate form? [ ] Yes [ ] No
If the answer is “yes” set forth particulars:
VERIFICATION
I, the undersigned, state that I am the person named in the foregoing Individual Information Sheet, that I have read and signed said Individual Information Sheet and know the contents thereof, including all exhibits attached thereto; and that the statements made therein, including any exhibits attached thereto, are true.
I certify/declare under penalty of perjury that the foregoing is true and correct.
Executed at
City County State
this _____________ day of _________ .
(Signature of Declarant)
NOTE: If this form is signed outside California complete the verification before a notary public in the space provided below.
State of
County of
Dated
at
(Signature of Affiant)
Subscribed and sworn to before me,
Notary Public in and for said
County and State
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1351, Health and Safety Code.
HISTORY
1. Amendment filed 6-29-84; effective thirtieth day thereafter (Register 84, No. 26).
2. Amendment filed 12-17-85; effective thirtieth day thereafter (Register 85, No. 51).
3. Change without regulatory effect amending section filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
4. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
5. Change without regulatory effect amending section filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.51.2. Consent to Service of Process.
Note • History
The consent to service of process required pursuant to these rules shall be in the following form:
TO THE DIRECTOR OF THE DEPARTMENT OF
MANAGED HEALTH CARE OF
THE STATE OF CALIFORNIA
CONSENT TO SERVICE OF PROCESS
KNOW ALL MEN BY THESE PRESENTS:
That the undersigned, ,
(a corporation organized under the laws of the State of )
(a partnership) (an individual) (other )
hereby irrevocably appoints the Director of the Department of Managed Health Care of the State of California, or his successor in office, to be his (its) attorney to receive service of any lawful process in any noncriminal suit, action or proceeding against him (it), or his (its) successor, executor, or administrator which arises under the Knox-Keene Health Care Service Plan Act of 1975 or any rule or order thereunder after this consent has been filed, with the same force and validity as if served personally on the undersigned.
For the purpose of compliance with the Corporations Code of the State of California, notice of the service and a copy of the process should be sent by registered or certified mail to the undersigned at the following address:
Name
Street Address
City State Zip Code
Dated: ____________________.
By
Title
State of California )
County of )
On ____________________ before me, (here insert name and title of the officer, personally appeared __________________________ personally known to me (or proved to me on the basis of satisfactory evidence) to be the person(s) whose name(s) is/are subscribed to the within instrument and acknowledged to me that he/she/they executed the same in his/her/their authorized capacity(ies), and that by his/her/their signature(s) on the instrument the person(s), or the entity upon behalf of which the person(s) acted, executed the instrument.
WITNESS my hand and official seal.
Signature (Seal)
Any certificate of acknowledgement taken in another state shall be sufficient in the State of California if it is taken in accordance with the laws of the place where the acknowledgement is made.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1351, Health and Safety Code and Section 1189, Civil Code.
HISTORY
1. Amendment filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
3. Change without regulatory effect amending section and Note filed 12-7-95 pursuant to section 100, title 1, California Code of Regulations (Register 95, No. 49).
4. Change without regulatory effect amending section filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
5. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
6. Change without regulatory effect amending section filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.51.3. Preparation and Amendment of Application for License As a Health Care Service Plan Under Section 1300.51.
Note • History
(a) General Instructions.
(1) Type the information requested in the English language using black ribbon.
(2) Complete each item on the application, and type “N/A” in the right hand margin for those items which are not applicable.
(3) Number each exhibit as specified in the item to which the exhibit responds. If several exhibits are required under the same letter/number designation, add a sequential letter or roman numeral as indicated in the following example. Example: If Item Q-1 calls for copies of the specified documents, an applicant employing three different documents would label them as follows: Exhibit Q-1-a; Exhibit Q-1-b; Exhibit Q-1-c.
(4) Arrange all exhibits in sequential order. Attach a “tab” to the right margin of the first page of each major exhibit or series of exhibits to facilitate ready reference.
(5) Submit originals only when requested. Otherwise, submit clearly legible mechanical reproductions.
(6) Submit requested information as an exhibit if the space provided in the application form itself is insufficient. Use the procedure detailed in Item (3), above, to indicate the exhibit number.
(7) Submit three complete copies of the original license application and each amendment submitted prior to licensure to the Department's Sacramento Office to the attention of the Health Plan Division Filing Clerk.
(b) Amendment of an Application.
(1) An amendment to application either before or after issuance of a license must comply with Rule 1300.52. However, Rules 1300.52.1 and 1300.52.2 apply only after an applicant has been licensed.
(c) Updating Application Prior to Licensure. In addition to complying with Rule 1300.52, an amendment to a pending application shall comply with the following:
(1) Material changes (see Rule 1300.45(1)) to information previously submitted in connection with an application (as amended to date) shall be submitted as an amendment to the license application immediately, except as provided in subsection (f) of Rule 1300.52.
(2) Nonmaterial changes to the information previously submitted in connection with an application (as amended to date) may be accumulated and shall be submitted as an amendment to the license application monthly or within 30 days (or other period requested by the Director) of each such change.
(3) Financial statements and calculations of tangible net equity previously submitted in connection with an application (as amended to date) shall be updated to an amendment to the license application which shall consist of quarterly financial statements (see Rule 1300.84.2a(1), (2), and (3)) and a calculation of applicant's tangible net equity as of the closing date of such quarter, and shall be filed within 30 days after the close of each quarter of applicant's fiscal year.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1351 and 1352, Health and Safety Code.
HISTORY
1. New section filed 12-17-85; effective thirtieth day thereafter (Register 85, No. 51).
2. Change without regulatory effect amending subsection (a)(7) filed 8-24-92; operative 9-23-92 (Register 92, No. 35).
3. Change without regulatory effect amending subsection (a)(7) filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
4. Change without regulatory effect amending subsection (c)(2) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.52. Amendments to Plan Application.
Note • History
An amendment to a plan application pursuant to subdivision (a) of Section 1352 of the Act shall be filed in the Department's Sacramento Office to the attention of the Health Plan Division Filing Clerk, upon the form contained in Section 1300.51 and shall include an original and two complete copies and comply with the following:
(a) The following portions of the application specified in Rule 1300.51 need not be amended after the issuance of a license:
Item E Summary of Information in Application
Item H-2 Map of Service Area.
Item H-3 Index to Map.
Item V Advertising.
Item CC Group Contract Enrollment Projections.
Item DD Individual Contract Enrollment Projections.
Item EE Summary of Enrollment Projections.
Item GG Current Financial Visibility Including Tangible Net Equity.
Item HH Projected Financial Viability.
(b) The amendment must be accompanied by a copy of the Execution Page of the application, and all portions of those pages must be completed.
(c) Attach to the Execution Page only those pages of the application and/or those exhibits which are changed by the amendment.
(d) If a page of the application is amended, complete all items on that page and “redline” or otherwise clearly designate the changed item.
(e) If an exhibit, other than a list required by Item 13A, 13C or 24D of the old application form or Item I-1, I-2 or I-3 of the new application is being amended.
(1) Furnish the complete exhibit as amended, bearing the same number as the original exhibit, with the changed portions of the exhibit “redlined” or otherwise clearly designated, or
(2) Furnish the pages of the exhibit which are amended, each page to be marked with the exhibit number and the page number of the exhibit, and with the changed portions “redlined” or otherwise clearly designated. If this method of amendment is employed, the applicant shall refile the entire exhibit as amended whenever more than 10% of its pages have been amended or promptly upon the request of the Director.
(f) A list furnished pursuant to Items 13A, 13C or 24D of the old application or Item I-1, I-2 or I-3 of the new application need be amended only when 10 percent or more of the names contained in the list for a service area have been changed. When amended, the complete list (or the list for the service area) shall be furnished following the instructions for the particular item, with each added item “redlined” and the names of persons deleted from the list shown at the end under the heading “deletions.”
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1351, 1351.1, 1352, 1359, 1363, 1367, 1367.2, 1367.3, 1367.5, 1367.6, 1367.7, 1367.8, 1367.9, 1367.15, 1368, 1369, 1370, 1370.1, 1373, 1373.1, 1373.2, 1373.4, 1373.5, 1373.6, 1373.7, 1373.8, 1374, 1374.7, 1374.10, 1374.11, 1374.12, 1375.1, 1376, 1377, 1378, 1386, 1399.52 and 1399.63, Health and Safety Code.
HISTORY
1. Amendment filed 12-17-85; effective thirtieth day thereafter (Register 85, No. 51).
2. Change without regulatory effect amending first paragraph filed 8-24-92; operative 9-23-92 (Register 92, No. 35).
3. Change without regulatory effect amending first paragraph filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
4. Change without regulatory effect amending subsection (e)(2) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.52.1. Notice of Material Modification.
Note • History
A notice of material modification of its operations or of any plan contract pursuant to subdivision (b) of Section 1352 of the Act shall be filed as an amendment to the application as provided in Section 1300.52, and there shall be attached to such amendment, preceding the Execution Page, the following form:
DEPARTMENT OF MANAGED HEALTH CARE
STATE OF CALIFORNIA
NOTICE OF MATERIAL MODIFICATION
Pursuant to
Health and Safety Code Sec. 1352(b)
1. Name of applicant:
2. Department of Managed Health Care File Number:
3. The fee for filing this application will be forwarded upon receipt of the billing therefore from the Director of the Department of Managed Health Care, pursuant to Health and Safety Code Section 1352(d) or pursuant to Section 1399.73 if this application involves a conversion or restructuring.
4. Pursuant to Subdivision (b) of Section 1352 of the Health and Safety Code, applicant requests approval of the material modification of its plan and/or operations, within the time specified below:
(Check appropriate box)
( ) Within the 20 business-day period provided in Section 1352(b).
( ) Applicant extends the time for action upon this notice by the Director until .
( ) Applicant requests accelerated approval by the Director for the following reasons:
5. Conversion or Restructuring. If this application involves a conversion or restructuring, the applicant shall fully disclose information which describes the proposed transaction and demonstrates how the charitable trust requirements of Section 1399.72(c) of the Act will be satisfied. In addition, the applicant shall submit a copy of all of its original and amended articles of incorporation and bylaws, and a report as described in Section 1399.70(a) of the Act. If this application involves a restructuring, the applicant shall also submit a public benefit program as described in Section 1399.71(b) of the Act.
6. Exempt Restructuring Transaction. If this application involves a transaction or transactions described in Section 1399.71(e) of the Act, the applicant shall fully disclose information which describes the transaction or transactions and demonstrates how the applicable conditions of exemption of Section 1399.71(e) of the Act will be satisfied.
7. Nonprofit Mutual Benefit Health Care Service Plans.
a. Assets subject to a charitable trust obligation. If this application involves a conversion or restructuring of a nonprofit mutual benefit health care service plan with any or all of its assets subject to a charitable trust obligation, the applicant shall submit information pursuant to Item 5 or Item 6 above and, if applicant believes that partial assets are subject to a charitable trust obligation, the applicant shall fully disclose information which: (i) describes why less than all of its assets are not subject to any charitable trust obligation, (ii) explains whether any charitable trust obligation terminated for any assets previously held subject to a charitable trust obligation, and (iii) demonstrates how every noncharitable trust obligation will be satisfied.
b. Assets not subject to a charitable trust obligation. An applicant that is a nonprofit mutual benefit health care service plan must comply with Item 7. a. above unless it has established that none of its assets are subject to a charitable trust obligation. If the applicant believes that this application involves a conversion or restructuring of a nonprofit mutual benefit health care service plan with no assets subject to any charitable trust obligation, the applicant shall submit a copy of all its original and amended articles of incorporation and bylaws and fully disclose information which: (i) describes the proposed transaction, (ii) describes why all its assets are not subject to any charitable trust obligation, (iii) explains whether any charitable trust obligation terminated for any assets previously held subject to a charitable trust obligation, and (iv) demonstrates how every noncharitable trust obligation will be satisfied.
Date:
Signature of Authorized Officer
Title
NOTE
Authority cited: Sections 1344 and 1399.74, Health and Safety Code. Reference: Sections 1352, 1399.70, 1399.71, 1399.72, 1399.73, 1399.74 and 1399.75, Health and Safety Code.
HISTORY
1. Amendment of form paragraph 3, new form paragraphs 5 and 6 and new Note filed 6-20-96 as an emergency; operative 6-20-96 (Register 96, No. 25). A Certificate of Compliance must be transmitted to OAL by 10-18-96 or emergency language will be repealed by operation of law on the following day.
2. Amendment of form paragraph 3, new form paragraphs 5 and 6 and new Note refiled 10-15-96 as an emergency; operative 10-18-96 (Register 96, No. 42). A Certificate of Compliance must be transmitted to OAL by 2-12-97 or emergency language will be repealed by operation of law on the following day.
3. Certificate of Compliance as to 10-15-96 order, including new form paragraphs 7.-7.b., transmitted to OAL 2-3-97 and filed 2-24-97 (Register 97, No. 9).
4. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
5. Change without regulatory effect amending section filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.52.2. Change in Plan Personnel.
Pursuant to subdivision (c) of Section 1352 of the Act, a plan shall file an amendment to its applications in the form required by Section 1300.52, when there are any of the following changes in personnel of the plan, of any management company of the plan, or of any parent company of such plan or management company:
(a) There is an addition or deletion of a director, trustee, principal officer, general partner, general manager or principal management persons, or persons occupying similar positions or performing similar functions, or a substantial and material change in the duties of any such person.
(b) There is the addition or deletion of a limited partner, shareholder or owner of an equity interest in the plan, whose interest exceeds 5 percent of the total partnership interests, shares or equity interests, or there is a change in the interest of any partner, shareholder or owner of an equity interest exceeding 5 percent of the total partnership interests, shares or equity interests.
(c) There is the addition or deletion of a principal creditor, as defined in Section 1300.45, a material change in the terms of the obligation to a principal creditor, a material increase or decrease in the amount due a principal creditor other than (except in the case of a demand obligation) by the normal terms of the obligation, or a default in the obligation to a principal creditor.
§1300.52.3. Filings and Actions Relating to Charitable or Public Activities.
Note • History
(a) Amendments to a plan application or notices of material modifications filed pursuant to Section 1352 or any other reports or filings under the Act shall not be deemed to be notices or requests for approval or ruling pursuant to Article 2, Part 11, Division 2, Title 1 of the Corporations Code or special reports pursuant to Section 1300.84.7, nor shall any such notices or requests for approval or ruling or special reports be deemed to be amendments to a plan application or notices of material modifications of a plan or its operations pursuant to Section 1352 or other reports or filings under the Act. However, this section shall not prevent a plan from filing notices or requests pursuant to Article 2 (commencing with Section 10820), Part 11, Division 2, Title 1 of the Corporations Code and/or special reports pursuant to Section 1300.84.7 concurrently with materials being filed under Section 1352 and utilizing common exhibits, subject to the provisions of Section 1300.824(c).
(b) Orders and other actions of the Director pursuant to Section 1352 or other provision of the Act, and the effects thereof, are limited to the effects contemplated under the Act and are of no effect or consequence in connection with any other law administered by the Director. Similarly, actions of the Director under any other law are of no effect or consequence in relation to Section 1352 or other provision of the Act.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1352, Health and Safety Code.
HISTORY
1. New section filed 4-16-82; effective thirtieth day thereafter (Register 82, No. 16).
2. Change without regulatory effect amending subsection (b) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.52.4. Standards for Amendments and Notices of Material Modification.
Note • History
Notwithstanding anything to the contrary in Sections 1300.52, 1300.52.1, 1300.52.2, and 1300.52.3, the following standards shall apply to amendments and notices of material modification to a plan license application once a health care service plan has been issued its license. These standards shall apply to full-service health care service plans and specialized health care service plans.
(a) General Statement of Requirements.
(i) If a plan makes a change that (A) constitutes an amendment to its plan license application and (B) is not listed in subsection (d) of this Section 1300.52.4, then the plan shall file an amendment with the Department. If the plan makes a change that is listed in subsection (d) of this Section 1300.52.4, then the plan shall file a notice of material modification with the Department.
(ii) The plan shall include in any amendment or notice of material modification any document or other information specifically required by one of the items set forth in Section 1300.51, which is pertinent to the amendment or material modification. Other information may be required if it is determined by the Department to be necessary in order to make a finding under the Act that the amendment or material modification is in the public interest and consistent with the intent and purpose of the Act.
(b) Specific Standards for Amendments.
(i)(A) In the event of any change to one or more of the items specified in Section 1351 of the Act, the plan shall file an amendment to its plan license application within 30 days after the plan implements that change, unless the change requires the filing of an amendment pursuant to clause (ii) of this subsection (b) or a notice of material modification pursuant to subsection (d) of this Section 1300.52.4. A change that is the subject of an amendment required to be filed pursuant to this subsection shall become effective on the date implemented.
(B) Notwithstanding the immediately subsection (b)(i)(A) of Section 1300.52.4: (I) if the plan has not been continuously licensed under the Act for the preceding 18 months and has not had group contracts in effect at all times during that period, then, to the extent the amendment includes any new or modified plan contract, disclosure form, or evidence of coverage, the change shall not be effective until 30 calendar days after the date the amendment was filed with the Department; and (II) to the extent the amendment includes any new or modified plan contract, disclosure form, or evidence of coverage that relates to an individuals health care service plan contract, the change shall not be effective until 30 calendar days after the date the amendment was filed with the Department.
(ii) In the event of any change described in Section 1352(c) of the Act, the plan shall file an amendment in accordance with the requirements of Section 1300.52.2. A change that is the subject of an amendment required to be filed pursuant to this subsection (b)(ii) shall be effective on the date implemented.
(c) Limited Enforcement or Disciplinary Action in Specified Circumstances Regarding Amendments.
If the Department does not provide objections to a plan with regard to an amendment within 30 days after the plan files the amendment, the Department may require the plan to make changes to comply with the Act and the rules adopted under the Act. The Department shall not take any disciplinary action or begin any other enforcement action against the plan with regard to the implementation of the changes described in the amendment, unless the material or any portion of the material was previously disapproved or otherwise objected to in writing by the Director or the plan knew or should have known that the material or any portion of the material violated any provision of the Act or the rules promulgated thereunder.
(d) Specific Standards for Notices of Material Modification.
If a plan proposes to make any of the following changes, the plan shall file a notice of material modification with the Department.
(i) An expansion, or a contraction or reduction, of the plan's approved service area.
(ii) The offering of a new health care service plan contract by the plan in any service area if the plan proposes to use a network of providers that is materially different from the network used for any other plan contract currently being offered by the plan.
(iii) A merger, consolidation, acquisition of a controlling interest, or sale of the plan or of all or substantially all of the assets of the plan, directly, or indirectly.
(iv) The plan's initial offering of a plan contract for small employers, which requires the filing of a notice of material modification pursuant to Section 1357.15 of the Act. A subsequent change with regard to the plan's small employer plan contracts shall be filed as an amendment pursuant to subsection (b) of this Section 1300.52.4, unless the change otherwise would require the filing of a notice of material modification.
(v) The plan's initial offering of a point-of-service contract, which requires the filing of a notice of material modification pursuant to Section 1374.69 of the Act. A subsequent change with regard to the plan's point-of-service plan contracts shall be filed as an amendment pursuant to subsection (b) of this Section 1300.52.4 unless the change otherwise would require the filing of a notice of material modification.
(vi) A change of plan name, which requires the filing of a notice of material modification pursuant to Section 1300.66.
(vii) A change that would have a material effect on the plan or on its health care service plan operations.
NOTE
Authority cited: Section 1351, Health and Safety Code. Reference: Sections 1352 and 1352.1, Health and Safety Code.
HISTORY
1. New section filed 11-30-98; operative 11-30-98 pursuant to Government Code section 11343.4(d) (Register 98, No. 49).
2. Change without regulatory effect amending subsection (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
Article 4. Solicitors
§1300.57. Solicitor Application.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1357 and 1358, Health and Safety Code.
HISTORY
1. Amendment filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.57.1. Solicitor Firm Application by Person Not Licensed by Insurance Commissioner.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1357, Health and Safety Code.
HISTORY
1. Amendment filed4-27-79; effective thirtieth day thereafter (Register 79, No. 17).
2. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.57.2. Amendment to Solicitor Firm Application.
History
HISTORY
1. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.57.3. Fees Payable by Licensed Insurance Agents and Brokers.
History
HISTORY
1. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.57.4. Solicitor Financial Records Authorization.
Note • History
NOTE
Authority cited: Sections 1343 and 1344, Health and Safety Code. Reference: Section 1357, Health and Safety Code.
HISTORY
1. New section filed 11-9-77 as an emergency; effective upon filing (Register 77, No. 46).
2. Certificate of Compliance filed 2-6-78 (Register 78, No. 6).
3. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.59. Plan Assurances Prior to Solicitation.
Note • History
Prior to allowing any person to engage in acts of solicitation on its behalf, each plan shall reasonably assure itself that such person has sufficient knowledge of its organization, procedures, plan contracts, and the provisions of the Act and these rules to do so lawfully.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1359, Health and Safety Code.
HISTORY
1. Repealer and new section filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
History
HISTORY
1. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.59.2. Waiver of Examination Requirements.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1359, Health and Safety Code.
HISTORY
1. Amendment filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
Article 5. Advertising and Disclosure
§1300.61. Filing of Advertising and Disclosure Forms.
Note • History
(a) Two copies of a proposed advertisement shall be filed. An advertisement is “filed” within the meaning of Section 1361 of the Act when a true copy thereof, accurately showing the final appearance of the advertisement, is received. To minimize the expense of changes in advertising copy, it may be submitted in draft form for preliminary review subject to the later filing of a proof or final copy, and the later filing of a proof or final copy may be waived when the draft copy is presented in a manner reasonably representing the final appearance of the advertisement. The text of audio or audio/visual advertising should indicate any directions for presentation, including voice qualities and the juxtaposition of the visual materials with the text.
(b) The Director will not issue letters of nondisapproval of advertising. If the person submitting the advertisement requests an order shortening the 30-day waiting period under Section 1361 of the Act, such order will be issued when an appropriate showing of the need therefor is made.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1361, Health and Safety Code.
HISTORY
1. Change without regulatory effect amending subsection (b) and adding Note filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.61.1. Exempt Advertising.
History
HISTORY
1. Repealer filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.61.3. Deceptive Advertising.
Note • History
Without limitation upon the meaning of subdivision (a) of Section 1352.1 and subdivisions (a) and (c) of Section 1361 of the Act, an advertisement or other consumer information is untrue, misleading or deceptive if:
(a) It represents that reimbursement is provided in full for the charge for services, unless the payment by the plan fully satisfies the liability to the provider.
(b) It represents that reimbursement is provided for the customary charges for services, unless the actual experience of the plan is that there is no balance billed for covered services.
(c) It represents that the plan, solicitor firm or solicitor or any provider or other person associated therewith is licensed or regulated by the Department of Managed Health Care or other governmental agency, unless such statement is required by law or regulation or unless such statement is accompanied by a satisfactory statement which counters any inference that such licensing or regulation is an assurance of financial soundness or the quality or extent of services. The phrase “a federally qualified health maintenance organization” and equivalent terms shall not be deemed deceptive advertising when used to refer to an organization which is so qualified under the Health Maintenance Organization Act of 1973. The display, on a plan contract which supplements Medicare with hospital or medical coverage, of the particular emblem approved by the federal Department of Health and Human Services and indicating that such contract meets the certification requirements of 42 U.S.C. 1395ss and the regulations of the Health Care Financing Administration thereunder, or, in lieu of such emblem, of such information, if any, regarding certification as may be approved in writing as to form and content by the Director, shall not be deemed deceptive when (1) the Director has found that such contract complies with the provisions of the Act and these rules and by written notification has authorized the plan to so display such emblem or, in lieu of such emblem, such expressly approved information, if any, regarding certification and has not revoked such authorization, and (2) such contract, and any related disclosure form, evidence of coverage, printed material, and advertising, contains no untrue information regarding the emblem and does not otherwise violate this subsection.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1352.1, 1360 and 1361, Health and Safety Code.
HISTORY
1. New subsection (c) filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Amendment filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
3. Change without regulatory effect amending subsection (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
4. Change without regulatory effect amending subsection (c) filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
Note • History
(a) The disclosure form required under subdivision (a) of Section 1363 of the Act shall conform to the following requirements.
(1) The text shall be printed in at least 10-point block type. Titles and captions shall be in at least 12-point to 15-point bold face type.
(2) It shall be written in clear, concise, easily understood language.
(3) It should relate to one form of plan contract; however, disclosure forms offering alternative plans or options will be permitted if presented in a manner which clearly identifies the alternatives and their effect upon the contract.
(4) It shall be presented in an easily readable format.
(b) The disclosure form shall be arranged and captioned in the following manner, except as may otherwise be permitted by the Director.
(1) The name of the plan and, if necessary, a designation of the plan contract described in the form.
(2) The title of the form (e.g., “disclosure form,” “summary of contract provisions”).
(3) A statement in at least 10-point bold face type to the effect that the disclosure form is a summary only and that the plan contract itself should be consulted to determine the governing contractual provisions.
(4) A statement to the effect that a specimen copy of the plan contract will be furnished on request.
(5) The caption “Principal Benefits and Coverages,” followed by a description of such benefits and coverages.
(6) The caption “Principal Exclusions and Limitations on Benefits,” followed by a description of the principal exclusions, exceptions, reductions and limitations that apply, and arranged in a uniform manner with the preceding section of the form.
(7) The caption “Prepayments Fees” followed by a statement of the methods by which such premium may be paid; the full premium charge of the plan; and a statement of the authority to change the fees during the term of the contract.
(8) The caption “Other Charges,” followed by a description of each co-payment, co-insurance, or deductible requirement that may be incurred by the member or the member's family in obtaining coverage under the plan.
(9) The caption “Choice of Physicians and Providers,” followed by a description of the nature, extent and circumstances under which choice is permitted. This section shall include, if applicable, a subcaption “Liability of Subscriber or Enrollee for Payment” followed by a description of the financial liability which is, or may be, incurred by the subscriber, enrollee or a third party by reason of the exercise of such choice.
(10) If applicable, the caption “Reimbursement Provisions,” followed by a description of the circumstances under which reimbursements are made under the plan contract, the extent of reimbursement, and the method of claim for reimbursement.
(11) The caption “Facilities,” followed by a statement of the principal facilities available under the plan contract, including their location and a description of the services, provided. The hours of availability of both emergency and nonemergency services should be indicated, either specifically or by general description. However, if the Director approves in advance, a plan may provide a telephone number from which information as to the identity and location of provider facilities defined in subsection (i)(2) of Section 1300.45 may be obtained, in lieu of listing such provider facilities.
(12) The caption “Renewal Provisions,” followed by a statement of the terms under which the plan contract may be renewed by the group or the plan member, including any reservation by the plan of any right to change premiums or other plan contract provisions.
(13) In the case of group contracts, the caption “Individual Continuation of Benefits,” followed by a statement of the terms and conditions under which subscribers and enrollees may remain in the plan, as provided pursuant to Subdivision (g) of Section 1373 of the Act.
(14) The caption “Termination of Benefits,” followed by a statement of the terms and conditions for cancellation or termination of benefits, including a statement as to when benefits shall cease in the event of nonpayment of the prepaid or periodic charge and the effect of nonpayment upon a member who is hospitalized or undergoing treatment for an ongoing condition.
(c) In the event the receipt of benefits or reimbursements to subscribers or enrollees under the plan contract is subject to significant delays, based upon the current experience of the plan, the disclosure form may be required by the Director to disclose such facts.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1363, Health and Safety Code.
HISTORY
1. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Change without regulatory effect amending subsections (b), (b)(11) and (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.63.1. Evidence of Coverage.
Note • History
(a) Each plan shall furnish to each individual subscriber, and make available to group contract holders for dissemination to all persons eligible under the group contract, either an evidence of coverage or a copy of the plan contract, which shall conform to the requirements of this section. The Director may permit the evidence of coverage and the disclosure form prescribed by Section 1300.63 to be presented in a single document if the purposes of each are fulfilled.
(b) Except as may be otherwise permitted by the Director, the evidence of coverage shall conform to the requirements of subsection (a) of Section 1300.63 and the following requirements:
(1) It shall be clearly entitled “Evidence of Coverage.”
(2) The portions of the text specifying (1) limitations, exclusions, exceptions and reductions; (2) rights of cancellation; (3) restrictions on renewal or reinstatement; (4) rights of the health plan to change benefits; (5) subsequent providers; and (6) liability of members in the event of nonpayment by the health plan, shall be in type not less than 2 points larger than the text relating to other provisions and in no event less than 12 point type.
(3) It shall be divided into sections, each of which shall have a title identifying the nature of the information contained therein.
(4) The evidence of coverage when taken as a whole, with consideration being given to format, typography and language, must constitute a fair disclosure of the provisions of the health plan.
(c) The evidence of coverage shall contain at a minimum the following information:
(1) The name of the health plan, the principal address from which it conducts its business and its telephone number.
(2) The definitions for the words contained therein that have meanings other than those attributed to them by the public in general usage.
(3) The manner in which the member can determine who is or may be entitled to benefits.
(4) The time and date or occurrence upon which coverage takes effect including a specification of any applicable waiting periods.
(5) The time and date or occurrence upon which coverage will terminate.
(6) The conditions upon which cancellation may be effected by the health plan or by the member, and a statement that a subscriber or enrollee who alleges that an enrollment or subscription has been cancelled or not renewed because of the enrollee's or subscriber's health status or requirements for health care services may request a review of cancellation by the Director.
(7) The conditions for and any restrictions upon the member's right to renewal or reinstatement.
(8) The amount of the periodic payment to be made by the member, the time by which the payment must be made, and the address at or to which the payment shall be made, except that a member under group coverage may be referred to the group contract holder for information regarding any sums to be withheld from the member's salary or to be paid by the member to the employer or group contract holder.
(9) A complete statement of all benefits and coverages and the related limitations, exclusions, exceptions, reductions, copayments, and deductibles.
(10) A statement of any restriction on assignment of sums payable to the member by the health plan.
(11) The exact procedure for obtaining benefits including the procedure for filing claims. The procedure for filing claims must state the time by which the claim must be filed, the form in which it is to be filed and the address at or to which it shall be delivered or mailed.
(12) Any procedures required to be followed by the member in the event any dispute arises under the contract, including any requirement for arbitration.
(13) The address and telephone number designated by the health plan to which complaints from members are to be directed, and a description of the plan's grievance procedure.
(14) A statement to the effect that, by statute, every contract between the health plan and a provider shall provide that in the event the health plan fails to pay the provider, the member shall not be liable to the provider for any sums owed by the health plan.
(15) A statement to the effect that in the event the health plan fails to pay a noncontracting provider, the member may be liable to the noncontracting provider for the cost of the services.
(16) An appropriate statement to fulfill the requirement of Section 1300.69(i)(1), unless the plan undertakes to mail such information annually.
(17) A statement which shall be set forth in boldface type not less than 2 points larger than the type required by subsection (b)(2): “This evidence of coverage constitutes only a summary of the health plan. The health plan contract must be consulted to determine the exact terms and conditions of coverage.”
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1345, 1360 and 1363, Health and Safety Code.
HISTORY
1. Amendment of subsection (c)(16) filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Amendment of subsection (c) filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
3. Change without regulatory effect amending subsections (a), (b) and (c)(6) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.63.2. Combined Evidence of Coverage and Disclosure Form.
Note • History
Notwithstanding Sections 1300.63 and 1300.63.1 of these rules, a plan may combine the evidence of coverage and disclosure form into a single document if such plan complies with each of the following requirements:
(a) Each plan shall furnish to each individual subscriber, and make available to group contract holders for dissemination to all persons eligible under the group contract, either a single document consisting of a combined evidence of coverage and disclosure form or a copy of the plan contract, which shall conform to the requirements of this section.
(b) Except as may be otherwise permitted by the Director, the combined evidence of coverage and disclosure form shall conform to the following requirements:
(1) It shall be clearly entitled “Combined Evidence of Coverage and Disclosure Form.”
(2) The text shall be printed in at least ten point block type. Titles and captions shall be in at least twelve point to fifteen point boldface type.
(3) It shall be written in clear, concise, easily understood language.
(4) It should relate to one form of plan contract; however, combined evidence of coverage and disclosure forms offering alternative plans or options will be permitted if presented in a manner which clearly identifies the alternatives and their effect upon the contract.
(5) It shall be presented in an easily readable format.
(6) The combined evidence of coverage and disclosure form when taken as a whole, with consideration being given to format, typography and language, must constitute a fair disclosure of the provisions of the health plan.
(c) The combined evidence of coverage and disclosure form shall contain at a minimum the following information:
(1) The name of the health plan, the principal address from which it conducts its business and its telephone number.
(2) A statement that the specimen of the plan contract will be furnished on request.
(3) The definitions for the words contained therein that have meanings other than those attributed to them by the public in general usage.
(4) The manner in which the member can determine who is or may be entitled to benefits, except that a member under group coverage may be referred to the group contract holder for such information.
(5) The time and date or occurrence upon which coverage takes effect including a specification of any applicable waiting periods.
(6) The time and date or occurrence upon which coverage will terminate.
(7) The conditions upon which cancellation may be effected by the health plan or by the member, and a statement that a subscriber or enrollee who alleges that an enrollment or subscription has been cancelled or not renewed because of the enrollee's or subscriber's health status or requirements for health care services may request a review of cancellation by the Director.
(8) The conditions for and any restrictions upon the member's right to renewal or reinstatement.
(9) The caption “Prepayment Fees” followed by a statement of the methods by which such premium may be paid; the full premium charge of the plan; and a statement of the authority to change the fees during the term of the contract.
(10) The amount of the periodic payment to be made by the member, the time by which the payment must be made, and the address at or to which the payment shall be made, except that a member under group coverage may be referred to the group contract holder for information regarding any sums to be withheld from the member's salary or to be paid by the member to the employer or group contract holder.
(11) A complete statement of all benefits and coverages and the related limitations, exclusions, exceptions, reductions, copayments, and deductibles.
(12) The caption “Other Charges,” followed by a description of each copayment, coinsurance, or deductible requirement that may be incurred by the member or the member's family in obtaining coverage under the plan.
(13) A statement of any restriction on assignment of sums payable to the member by the health plan.
(14) The exact procedure for obtaining benefits including the procedure for filing claims. The procedure for filing claims must state the time by which the claim must be filed, the form in which it is to be filed, and the address at or to which it shall be delivered or mailed.
(15) Any procedures required to be followed by the member in the event any dispute arises under the contract, including any requirement for arbitration.
(16) The address and telephone number designated by the health plan to which complaints from members are to be directed, and a description of the plan's grievance procedure.
(17) The caption “Choice of Physicians and Providers,” followed by description of the nature, extent and circumstances under which choice is permitted. This section shall include, if applicable, a subcaption “Liability of Subscriber or Enrollee for Payment” followed by a description of the financial liability which is, or may be, incurred by the subscriber, enrollee or a third party by reason of the exercise of such choice.
(18) A statement to the effect that, by statute, every contract between the health plan and a provider shall provide that in the event the health plan fails to pay the provider, the member shall not be liable to the provider for any sums owed by the health plan.
(19) A statement to the effect that in the event the health plan fails to pay noncontracting providers, the member may be liable to the noncontracting provider for the cost of services.
(20) If applicable, the caption “Reimbursement Provisions,” followed by a description of the circumstances under which reimbursements are made under the plan contract, the extent of reimbursement, and the method of claim for reimbursement.
(21) The caption “Renewal Provisions,” followed by a statement of the terms under which the plan contract may be renewed by the group or the plan member, as appropriate, including any reservation by the plan of any right to change premiums or other plan contract provisions.
(22) The caption “Facilities,” followed by a statement of the principal facilities available under the plan contract, including their location and description of the services provided. The hours of availability of both emergency and non-emergency services should be indicated, either specifically or by general description. However, if the Director approves in advance, a plan may provide a telephone number from which information as to the identity and location of the provider facilities defined in subsection (i)(2) of Section 1300.45 of these rules may be obtained, in lieu of listing such provider facilities.
(23) In the case of group contracts, the caption “Individual Continuation of Benefits,” followed by a statement of the terms and conditions under which subscribers and enrollees may remain in the plan, as provided pursuant to subdivision (g) of Section 1373 of the Act.
(24) The caption “Termination of Benefits,” followed by a statement of the terms and conditions for cancellation or termination of benefits, including a statement as to when benefits shall cease in the event of nonpayment of the prepaid or periodic charge and the effect of nonpayment upon a member who is hospitalized or undergoing treatment for an ongoing condition.
(25) Any appropriate statement to fulfill the requirement of Section 1300.69(i)(1) of these rules, unless the plan undertakes to mail such information annually.
(26) In the event that receipt of benefits or reimbursements to subscribers or enrollees under the plan contract is subject to significant delays, based upon the current experience of the plan, the combined evidence of coverage and disclosure form may be required by the Director to disclose such facts.
(27) A statement which shall be set forth in boldface type not less than two points larger than the type required by subsection (b)(2): “This combined evidence of coverage and disclosure form constitutes only a summary of the health plan. The health plan contract must be consulted to determine the exact terms and conditions of coverage.”
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1345, 1360, 1363 and 1368, Health and Safety Code.
HISTORY
1. New section filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
2. Change without regulatory effect amending subsections (b), (c)(7), (c)(22) and (c)(26) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.63.3. Experimental Disclosure.
Note • History
Notwithstanding those provisions of Sections 1300.63, 1300.63.1, 1300.63.2, and 1300.67.4 which require the use of any particular type size, boldface type, caption, subcaption, heading, design, order, or format, the Director by order may approve, for experimental use, reasonable alternatives to such requirements for a disclosure form, evidence of coverage, combined evidence of coverage and disclosure form, or plan contract upon the written request of a plan, for such period and under such conditions as the Director may specify, subject to each of the following conditions:
(a) That the plan submits two draft copies of the document containing the proposed alternatives, one as proposed to be used and the other redlined to highlight the proposed changes, along with two copies of the related plan contract, at least 30 days prior to any use of the document, or such shorter period as the Director by order may allow.
(b) That the plan demonstrates to the satisfaction of the Director that the document containing the proposed alternatives furthers the purposes of the Act, otherwise complies with the Act and the rules thereunder, and will provide to actual or potential subscribers or enrollees (as the case may be) unobjectionable information at least as clear, concise, accurate, easily understood, and easily readable as could otherwise be achieved.
(c) That the plan submits a proof or final copy of the document at such time, not to exceed 30 days, prior to its initial use as may be specified by the Director.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1363, Health and Safety Code.
HISTORY
1. New section filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.63.50. Medicare Supplement Additional Disclosure.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1363, Health and Safety Code.
HISTORY
1. New section filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
2. Repealer and new table, amendment of subsection (a)(5)(A)8., and new subsection (a)(5)(A)9. filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
3. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.64.50. Medicare Supplement Application Information.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1364, Health and Safety Code.
HISTORY
1. New section filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
2. Amendment filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
3. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.64.51. Medicare Supplement “Buyer's Guide.”
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1364, Health and Safety Code.
HISTORY
1. New section filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
2. Amendment of subsections (a) and (b) filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
3. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.64.52. Standards for Marketing Medicare Supplement Contracts.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1346, 1364 and 1367.15, Health and Safety Code; 42 U.S.C. 1395ss.
HISTORY
1. New section filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.64.53. Reporting of Multiple Coverage.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1367.15 and 1384(d)(i), Health and Safety Code; 42 U.S.C. 1395ss.
HISTORY
1. New section filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.64.54. Replacement Contracts: Elimination of Waiting Periods.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1367.15 and 1384(d)(i), Health and Safety Code; 42 U.S.C. 1395ss.
HISTORY
1. New section filed 1-8-92; operative 1-1-92 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.64.55. Permitted Compensation Arrangements for the Sale of Medicare Supplement Contracts.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1346(i), 1367(h) and 1367.15, Health and Safety Code; 42 U.S.C. 1395ss.
HISTORY
1. New section filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
Article 6. Appeals on Cancellation
§1300.65. Cancellation of Enrollment.
Note • History
(a) For the purposes of subdivision (a)(3) of Section 1365 of the Act, “good cause” means a cause for cancellation or failure to renew which the Director has not found to be objectionable by regulation.
(b) In the event that the plan cancels or refuses to renew a plan contract, or a subscription or enrollment thereunder, the plan shall mail a notice of cancellation to the subscriber at the subscriber's address of record with the plan. However, in the event that the plan cancels or refuses to renew a group contract, the plan need not mail a notice of cancellation to each subscriber thereunder if:
(1) the plan contract requires the group contract holder to mail promptly any such notice to each subscriber,
(2) the plan mails or hand delivers a notice of cancellation to the group contract holder designated in the plan contract, and
(3) the plan demonstrates that the group contract holder promptly mailed a legible, true copy of the notice of cancellation to each subscriber at the subscriber's current address and promptly provided proof of such mailing and the date thereof to the plan. Unless the plan contract otherwise provides, a notice of cancellation pursuant to subdivision (a)(2) of Section 1365 of the Act may be effective upon mailing to the subscriber, and a notice of cancellation pursuant to subdivision (a)(3) may be effective 15 days after the notice is mailed to the subscriber. This subsection is not applicable to a loss of eligibility for Medi-Cal benefits.
(c) A notice of cancellation must be in writing and dated, and must state
(1) the cause for cancellation, with specific reference to the clause of the plan contract giving rise to the right of cancellation,
(2) that the cause for cancellation was not the enrollee's or subscriber's health status or requirements for health care services,
(3) the time when the cancellation is effective in accordance with the provisions of subsection (b) or Medi-Cal requirements, as appropriate, and
(4) that a subscriber or enrollee who alleges that an enrollment or subscription has been cancelled or not renewed because of the enrollee's or subscriber's health status or requirements for health care services may request a review of cancellation by the Director.
(d) A plan which refuses to renew a subscription or enrollment shall give notice to the person seeking such renewal substantially in the form and content required by subsection (c), except where nonrenewal or nonenrollment is based on avoidance of duplication of coverage where the subscriber or applicant has become eligible for Medi-Care benefits.
(e) The terms “cancellation” and “failure to renew,” for the purposes of Section 1365 of the Act, do not include a voluntary termination by a subscriber or the termination of a plan contract which does not contain a renewal provision.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1365, Health and Safety Code.
HISTORY
1. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Change without regulatory effect amending subsections (a) and (c)(4) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.65.1. Cancellation Complaint Form.
Note • History
(a) A request that the Director review cancellation of, or refusal to renew, an enrollment or subscription pursuant to subdivision (b) of Section 1365 of the Act shall be made in writing, signed by the subscriber or enrollee or the legal representative of the subscriber or enrollee and it shall be in the following form (or in letter form containing the information specified in the form below):
DEPARTMENT OF MANAGED HEALTH CARE
STATE OF CALIFORNIA
TO: Health Plan Division Date:
Department of Managed Care
320 West 4th Street, Suite 750
Los Angeles, CA 90013-1105
RE: COMPLAINT ON CANCELLATION OF,
OR REFUSAL TO RENEW, HEALTH CARE
SERVICE PLAN BENEFITS.
The undersigned requests that the Director review the cancellation or refusal to renew the subscription or enrollment for health plan benefits pursuant to Section 1365 of the Knox-Keene Health Care Service Plan Act of 1975, as follows:
1. Name of person whose benefits were cancelled or not renewed:
2. Name of subscriber, if different than “1” above:
3. Name of plan:
4. Subscriber or Enrollee Account or Identification Number:
5. If applicable, the Group Identification Number:
6. Date notice of cancellation or refusal to renew was received:
7. Attach copies of:
(a) The notice of cancellation or refusal to renew received from the plan.
(b) Any correspondence with the plan regarding such cancellation or refusal to renew.
8. State why such cancellation or refusal to renew is believed to be an improper action by the plan:
9. Are you aware of the existence of any grounds for cancellation or refusal to renew under the terms of the agreement with the plan?
10. Explain why you believe that the cause or causes for cancellation enumerated in the notice of cancellation received from the Plan are inadequate or untrue. Attach copies of any documents which are relevant to your explanation.
11. Does such cancellation or refusal to renew prevent or interfere with providing medical care to any person currently in need of such care?
12. Has the person named in item 1 above whose benefits were cancelled received any medical or health care since the cancellation? If so, what services have been received and how much did they cost?
Signature of Complainant
(b) Upon receipt of a complaint pursuant to subsection (b) of Section 1365 of the Act, the Director will immediately forward a copy of such complaint to the plan, together with a request that the plan furnish the Director with
(1) a copy of the notice of cancellation or refusal to renew,
(2) a copy of any correspondence relating thereto,
(3) a statement of the reason for such cancellation or refusal to renew and
(4) a response to the complainant's allegations pursuant to Item 9 of the complaint form in subsection (a). Such information shall be returned to the Director by the plan within 10 business days following its receipt of the Director's request.
(c) Following examination of the information provided pursuant to subsection (a) and (b), the Director will notify the complainant and the plan of the determination of whether or not a proper complaint exists under the provisions of subdivision (b) of Section 1365 of the Act.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1365, Health and Safety Code.
HISTORY
1. Amendment of subsection (a) filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Change without regulatory effect amending form filed 5-24-99 pursuant to section 100, title 1, California Code of Regulations (Register 99, No. 22).
3. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
4. Change without regulatory effect amending subsection (a) filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.66. Deceptive Plan Names.
Note • History
(a) A change of plan name is a “material modification” of the plan within the meaning of subdivision (b) of Section 1352 of the Act.
(b) A plan name will be considered deceptive if it suggests the quality of care furnished by the plan, or that full benefits are provided for health care or a specialized area of health care, or that the cost of benefits to members of the plan is lower than the cost of similar benefits purchased elsewhere, and in any such case the express or implied representation contained in the plan name is demonstrably untrue or is not supported by substantial evidence, at all times while such name is used by the plan. Nothing in this subsection limits or restricts the Director from a determination that a plan or solicitor firm name is deceptive for reasons other than those stated herein.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1366, Health and Safety Code.
HISTORY
1. Change without regulatory effect amending subsection (b) and adding Note filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
Article 7. Standards
§1300.67. Scope of Basic Health Care Services.
Note • History
The basic health care services required to be provided by a health care service plan to its enrollees shall include, where medically necessary, subject to any copayment, deductible, or limitation of which the Director may approve:
(a) Physician services, which shall be provided by physicians licensed to practice medicine or osteopathy in accordance with applicable California law. There shall also be provided consultation with and referral by physicians to other physicians.
(1) The plan may also include, when provided by the plan, consultation and referral (physician or, if permitted by law, patient initiated) to other health professionals who are defined as dentists, nurses, podiatrists, optometrists, physician's assistants, clinical psychologists, social workers, pharmacists, nutritionists, occupational therapists, physical therapists and other professionals engaged in the delivery of health services who are licensed to practice, are certified, or practice under authority of the plan, a medical group, or individual practice association or other authority authorized by applicable California law.
(b) Inpatient hospital services, which shall mean short-term general hospital services, including room with customary furnishings and equipment, meals (including special diets as medically necessary), general nursing care, use of operating room and related facilities, intensive care unit and services, drugs, medications, biologicals, anesthesia and oxygen services, diagnostic laboratory and x-ray services, special duty nursing as medically necessary, physical therapy, respiratory therapy, administration of blood and blood products, and other diagnostic, therapeutic and rehabilitative services as appropriate, and coordinated discharge planning including the planning of such continuing care as may be necessary, both medically and as a means of preventing possible early rehospitalization.
(c) Ambulatory care services, (outpatient hospital services) which shall include diagnostic and treatment services, physical therapy, speech therapy, occupational therapy services as appropriate, and those hospital services which can reasonably be provided on an ambulatory basis. Such services may be provided at a hospital, any other appropriate licensed facility, or any appropriate facility which is not required by law to be licensed, if the professionals delivering such services are licensed to practice, are certified, or practice under the authority of the plan, a medical group, or individual practice association or other authority authorized by applicable California law.
(d) Diagnostic laboratory services, diagnostic and therapeutic radiological services, and other diagnostic services, which shall include, but not be limited to, electrocardiography and electroencephalography.
(e) Home health services, which shall include, where medically appropriate, health services provided at the home of an enrollee as prescribed or directed by a physician or osteopath licensed to practice in California. Such home health services shall include diagnostic and treatment services which can reasonably be provided in the home, including nursing care, performed by a registered nurse, public health nurse, licensed vocational nurse or licensed home health aide.
(1) Home health services may also include such rehabilitation, physical, occupational or other therapy, as the physician shall determine to be medically appropriate.
(f) Preventive health services (including services for the detection of asymptomatic diseases), which shall include, under a physician's supervision,
(1) reasonable health appraisal examinations on a periodic basis;
(2) a variety of voluntary family planning services;
(3) prenatal care;
(4) vision and hearing testing for persons through age 16;
(5) immunizations for children in accordance with the recommendations of the American Academy of Pediatrics and immunizations for adults as recommended by the U.S. Public Health Service;
(6) venereal disease tests;
(7) cytology examinations on a reasonable periodic basis;
(8) effective health education services, including information regarding personal health behavior and health care, and recommendations re-- garding the optimal use of health care services provided by the plan or health care organizations affiliated with the plan.
(g)(1) Emergency health care services which shall be available and accessible to enrollees on a twenty-four hour a day, seven days a week, basis within the health care service plan area. Emergency health care services shall include ambulance services for the area served by the plan to transport the enrollee to the nearest twenty-four hour emergency facility with physician coverage, designated by the Health Care Service Plan.
(2) Coverage and payment for out-of-area emergencies or urgently needed services involving enrollees shall be provided on a reimbursement or fee-for-service basis and instructions to enrollees must be clear regarding procedures to be followed in securing such services or benefits. Emergency services defined in section 1317.1 include active labor. “Urgently needed services” are those services necessary to prevent serious deterioration of the health of an enrollee, resulting from an unforeseen illness, injury, or complication of an existing condition, including pregnancy, for which treatment cannot be delayed until the enrollee returns to the plan's service area. “Urgently needed services” includes maternity services necessary to prevent serious deterioration of the health of the enrollee or the enrollee's fetus, based on the enrollee's reasonable belief that she has a pregnancy-related condition for which treatment cannot be delayed until the enrollee returns to the plan's service area.
(h) Hospice services as set forth in Section 1300.68.2.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1317.1, 1345 and 1367, Health and Safety Code.
HISTORY
1. Amendment of subsection (c) filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Change without regulatory effect amending introductory paragraph filed 12-22-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 51).
3. New subsection (h) filed 6-26-2001; operative 7-26-2001 (Register 2001, No. 26).
4. Redesignation and amendment of former subsection (g) as new subsections (g)(1)-(2) filed 9-16-2003; operative 10-16-2003 (Register 2003, No. 38).
§1300.67.2.2. Timely Access to Non-Emergency Health Care Services.
Note • History
(a) Application
(1) All health care service plans that provide or arrange for the provision of hospital or physician services, including specialized mental health plans that provide physician or hospital services, or that provide mental health services pursuant to a contract with a full service plan, shall comply with the requirements of this section.
(2) Dental, vision, chiropractic, and acupuncture plans shall comply with subsections (c)(1), (3), (4), (7), (9) and (10), and subsections (d)(1) and (g)(1). Dental plans shall also comply with subsection (c)(6).
(3) The obligation of a plan to comply with this section shall not be waived when the plan delegates to its medical groups, independent practice associations, or other contracting entities any services or activities that the plan is required to perform. A plan's implementation of this section shall be consistent with the requirements of the Health Care Providers' Bill of Rights, and a material change in the obligations of a plan's contracting providers shall be considered a material change to the provider contract, within the meaning of subsections (b) and (g)(2) of Section 1375.7 of the Act.
(4) This section confirms requirements for plans to provide or arrange for the provision of access to health care services in a timely manner, and establishes additional metrics for measuring and monitoring the adequacy of a plan's contracted provider network to provide enrollees with timely access to needed health care services. This section does not:
(A) Establish professional standards of practice for health care providers;
(B) Establish requirements for the provision of emergency services; or
(C) Create a new cause of action or a new defense to liability for any person.
(b) Definitions. For purposes of this section, the following definitions apply.
(1) “Advanced access” means the provision, by an individual provider, or by the medical group or independent practice association to which an enrollee is assigned, of appointments with a primary care physician, or other qualified primary care provider such as a nurse practitioner or physician's assistant, within the same or next business day from the time an appointment is requested, and advance scheduling of appointments at a later date if the enrollee prefers not to accept the appointment offered within the same or next business day.
(2) “Appointment waiting time” means the time from the initial request for health care services by an enrollee or the enrollee's treating provider to the earliest date offered for the appointment for services inclusive of time for obtaining authorization from the plan or completing any other condition or requirement of the plan or its contracting providers.
(3) “Preventive care” means health care provided for prevention and early detection of disease, illness, injury or other health condition and, in the case of a full service plan includes but is not limited to all of the basic health care services required by subsection (b)(5) of Section 1345 of the Act, and Section 1300.67(f) of Title 28.
(4) “Provider group” has the meaning set forth in subsection (g) of Section 1373.65 of the Act.
(5) “Triage” or “screening” means the assessment of an enrollee's health concerns and symptoms via communication, with a physician, registered nurse, or other qualified health professional acting within his or her scope of practice and who is trained to screen or triage an enrollee who may need care, for the purpose of determining the urgency of the enrollee's need for care.
(6) “Triage or screening waiting time” means the time waiting to speak by telephone with a physician, registered nurse, or other qualified health professional acting within his or her scope of practice and who is trained to screen or triage an enrollee who may need care.
(7) “Urgent care” means health care for a condition which requires prompt attention, consistent with subsection (h)(2) of Section 1367.01 of the Act.
(c) Standards for Timely Access to Care.
(1) Plans shall provide or arrange for the provision of covered health care services in a timely manner appropriate for the nature of the enrollee's condition consistent with good professional practice. Plans shall establish and maintain provider networks, policies, procedures and quality assurance monitoring systems and processes sufficient to ensure compliance with this clinical appropriateness standard.
(2) Plans shall ensure that all plan and provider processes necessary to obtain covered health care services, including but not limited to prior authorization processes, are completed in a manner that assures the provision of covered health care services to enrollees in a timely manner appropriate for the enrollee's condition and in compliance with the requirements of this section.
(3) When it is necessary for a provider or an enrollee to reschedule an appointment, the appointment shall be promptly rescheduled in a manner that is appropriate for the enrollee's health care needs, and ensures continuity of care consistent with good professional practice, and consistent with the objectives of Section 1367.03 of the Act and the requirements of this section.
(4) Interpreter services required by Section 1367.04 of the Act and Section 1300.67.04 of Title 28 shall be coordinated with scheduled appointments for health care services in a manner that ensures the provision of interpreter services at the time of the appointment. This subsection does not modify the requirements established in Section 1300.67.04, or approved by the Department pursuant to Section 1300.67.04 for a plan's language assistance program.
(5) In addition to ensuring compliance with the clinical appropriateness standard set forth at subsection (c)(1), each plan shall ensure that its contracted provider network has adequate capacity and availability of licensed health care providers to offer enrollees appointments that meet the following timeframes:
(A) Urgent care appointments for services that do not require prior authorization: within 48 hours of the request for appointment, except as provided in (G);
(B) Urgent care appointments for services that require prior authorization: within 96 hours of the request for appointment, except as provided in (G);
(C) Non-urgent appointments for primary care: within ten business days of the request for appointment, except as provided in (G) and (H);
(D) Non-urgent appointments with specialist physicians: within fifteen business days of the request for appointment, except as provided in (G) and (H);
(E) Non-urgent appointments with a non-physician mental health care provider: within ten business days of the request for appointment, except as provided in (G) and (H);
(F) Non-urgent appointments for ancillary services for the diagnosis or treatment of injury, illness, or other health condition: within fifteen business days of the request for appointment, except as provided in (G) and (H);
(G) The applicable waiting time for a particular appointment may be extended if the referring or treating licensed health care provider, or the health professional providing triage or screening services, as applicable, acting within the scope of his or her practice and consistent with professionally recognized standards of practice, has determined and noted in the relevant record that a longer waiting time will not have a detrimental impact on the health of the enrollee;
(H) Preventive care services, as defined at subsection (b)(3), and periodic follow up care, including but not limited to, standing referrals to specialists for chronic conditions, periodic office visits to monitor and treat pregnancy, cardiac or mental health conditions, and laboratory and radiological monitoring for recurrence of disease, may be scheduled in advance consistent with professionally recognized standards of practice as determined by the treating licensed health care provider acting within the scope of his or her practice; and
(I) A plan may demonstrate compliance with the primary care time-elapsed standards established by this subsection through implementation of standards, processes and systems providing advanced access to primary care appointments, as defined at subsection (b)(1).
(6) In addition to ensuring compliance with the clinical appropriateness standard set forth at subsection (c)(1), each dental plan, and each full service plan offering coverage for dental services, shall ensure that contracted dental provider networks have adequate capacity and availability of licensed health care providers to offer enrollees appointments for covered dental services in accordance with the following requirements:
(A) Urgent appointments within the dental plan network shall be offered within 72 hours of the time of request for appointment, when consistent with the enrollee's individual needs and as required by professionally recognized standards of dental practice;
(B) Non-urgent appointments shall be offered within 36 business days of the request for appointment, except as provided in subsection (c)(6)(C); and
(C) Preventive dental care appointments shall be offered within 40 business days of the request for appointment.
(7) Plans shall ensure they have sufficient numbers of contracted providers to maintain compliance with the standards established by this section.
(A) This section does not modify the requirements regarding provider-to-enrollee ratio or geographic accessibility established by Sections 1300.51, 1300.67.2 or 1300.67.2.1 of Title 28.
(B) A plan operating in a service area that has a shortage of one or more types of providers shall ensure timely access to covered health care services as required by this section, including applicable time-elapsed standards, by referring enrollees to, or, in the case of a preferred provider network, by assisting enrollees to locate, available and accessible contracted providers in neighboring service areas consistent with patterns of practice for obtaining health care services in a timely manner appropriate for the enrollee's health needs. Plans shall arrange for the provision of specialty services from specialists outside the plan's contracted network if unavailable within the network, when medically necessary for the enrollee's condition. Enrollee costs for medically necessary referrals to non-network providers shall not exceed applicable co-payments, co-insurance and deductibles. This requirement does not prohibit a plan or its delegated provider group from accommodating an enrollee's preference to wait for a later appointment from a specific contracted provider.
(8) Plans shall provide or arrange for the provision, 24 hours per day, 7 days per week, of triage or screening services by telephone as defined at subsection (b)(5).
(A) Plans shall ensure that telephone triage or screening services are provided in a timely manner appropriate for the enrollee's condition, and that the triage or screening waiting time does not exceed 30 minutes.
(B) A plan may provide or arrange for the provision of telephone triage or screening services through one or more of the following means: plan-operated telephone triage or screening services consistent with subsection (b)(5); telephone medical advice services pursuant to Section 1348.8 of the Act; the plan's contracted primary care and mental health care provider network; or other method that provides triage or screening services consistent with the requirements of this subsection.
1. A plan that arranges for the provision of telephone triage or screening services through contracted primary care and mental health care providers shall require those providers to maintain a procedure for triaging or screening enrollee telephone calls, which, at a minimum, shall include the employment, during and after business hours, of a telephone answering machine and/or an answering service and/or office staff, that will inform the caller:
a. Regarding the length of wait for a return call from the provider; and
b. How the caller may obtain urgent or emergency care including, when applicable, how to contact another provider who has agreed to be on-call to triage or screen by phone, or if needed, deliver urgent or emergency care.
2. A plan that arranges for the provision of triage or screening services through contracted primary care and mental health care providers who are unable to meet the time-elapsed standards established in paragraph (8)(A) shall also provide or arrange for the provision of plan-contracted or operated triage or screening services, which shall, at a minimum, be made available to enrollees affected by that portion of the plan's network.
3. Unlicensed staff persons handling enrollee calls may ask questions on behalf of a licensed staff person in order to help ascertain the condition of an enrollee so that the enrollee can be referred to licensed staff. However, under no circumstances shall unlicensed staff persons use the answers to those questions in an attempt to assess, evaluate, advise, or make any decision regarding the condition of an enrollee or determine when an enrollee needs to be seen by a licensed medical professional.
(9) Dental, vision, chiropractic, and acupuncture plans shall ensure that contracted providers employ an answering service or a telephone answering machine during non-business hours, which provide instructions regarding how enrollees may obtain urgent or emergency care including, when applicable, how to contact another provider who has agreed to be on-call to triage or screen by phone, or if needed, deliver urgent or emergency care.
(10) Plans shall ensure that, during normal business hours, the waiting time for an enrollee to speak by telephone with a plan customer service representative knowledgeable and competent regarding the enrollee's questions and concerns shall not exceed ten minutes.
(d) Quality Assurance Processes. Each plan shall have written quality assurance systems, policies and procedures designed to ensure that the plan's provider network is sufficient to provide accessibility, availability and continuity of covered health care services as required by the Act and this section. In addition to the requirements established by Section 1300.70 of Title 28, a plan's quality assurance program shall address:
(1) Standards for the provision of covered services in a timely manner consistent with the requirements of this section.
(2) Compliance monitoring policies and procedures, filed for the Department's review and approval, designed to accurately measure the accessibility and availability of contracted providers, which shall include:
(A) Tracking and documenting network capacity and availability with respect to the standards set forth in subsection (c);
(B) Conducting an annual enrollee experience survey, which shall be conducted in accordance with valid and reliable survey methodology and designed to ascertain compliance with the standards set forth at subsection (c);
(C) Conducting an annual provider survey, which shall be conducted in accordance with valid and reliable survey methodology and designed to solicit, from physicians and non-physician mental health providers, perspective and concerns regarding compliance with the standards set forth at subsection (c);
(D) Reviewing and evaluating, on not less than a quarterly basis, the information available to the plan regarding accessibility, availability and continuity of care, including but not limited to information obtained through enrollee and provider surveys, enrollee grievances and appeals, and triage or screening services; and
(E) Verifying the advanced access programs reported by contracted providers, medical groups and independent practice associations to confirm that appointments are scheduled consistent with the definition of advanced access in subsection (b)(1).
(F) A plan that provides services through a preferred provider organization network may, for that portion of its network, demonstrate compliance with subsections (d)(2)(A) and (D) by monitoring, on not less than an annual basis: the number of PPO primary care and specialty physicians under contract with the plan in each county of the plan's service area; enrollee grievances and appeals regarding timely access; and the rates of compliance with the time-elapsed standards established in subsection (c)(5).
(3) A plan shall implement prompt investigation and corrective action when compliance monitoring discloses that the plan's provider network is not sufficient to ensure timely access as required by this section, including but not limited to taking all necessary and appropriate action to identify the cause(s) underlying identified timely access deficiencies and to bring its network into compliance. Plans shall give advance written notice to all contracted providers affected by a corrective action, and shall include: a description of the identified deficiencies, the rationale for the corrective action, and the name and telephone number of the person authorized to respond to provider concerns regarding the plan's corrective action.
(e) Enrollee Disclosure and Education
(1) Plans shall disclose in all evidences of coverage the availability of triage or screening services and how to obtain those services. Plans shall disclose annually, in plan newsletters or comparable enrollee communications, the plan's standards for timely access.
(2) The telephone number at which enrollees can access triage and screening services shall be included on enrollee membership cards. A plan or its delegated provider group may comply with this requirement through an additional selection in its automated customer service telephone answering system, where applicable, so long as the customer service number is included on the enrollee's membership card.
(f) Plans may file, by notice of material modification, a request for the Department's approval of alternative time-elapsed standards or alternatives to time-elapsed standards. A request for an alternative standard shall include:
(1) An explanation of the plan's clinical and operational reasons for requesting the alternative standard, together with information and documentation, including scientifically valid evidence (based on reliable and verifiable data), demonstrating that the proposed alternative standard is consistent with professionally recognized standards of practice and a description of the expected impact of the alternative standard on clinical outcomes, on access for enrollees, and on contracted health care providers;
(2) The burden shall be on the plan to demonstrate and substantiate why a proposed alternative standard is more appropriate than time elapsed standards. Plans that have received approval for an alternative standard shall file, on an annual basis, an amendment requesting approval for continued use of the alternative standard, and providing updated information and documentation to substantiate the continued need for the alternative standard; and
(3) In approving or disapproving a plan's proposed alternative standards the Department may consider all relevant factors, including but not limited to the factors set forth in subsections (d) and (e) of Section 1367.03 of the Act and subsection (c) of Section 1300.67.2.1 of Title 28.
(g) Filing, Implementation and Reporting Requirements.
(1) Not later than twelve months after the effective date of this section, plans shall implement the policies, procedures and systems necessary for compliance with the requirements of Section 1367.03 of the Act and this section. Not later than nine months after the effective date of this section, each plan shall file an amendment pursuant to Section 1352 of the Act disclosing how it will achieve compliance with the requirements of this section, which shall include substantiating documentation, including but not limited to, quality assurance policies and procedures, survey forms, subscriber and enrollee disclosures, and amendments to provider contracts. The amendment shall also include documentation sufficient to confirm the plan's compliance, as of the date of filing, with existing requirements regarding physician-to-enrollee ratios, including but not limited to updated Exhibits I-1 and I-4 to the plan's license application. If a plan asserts prior Department approval of alternative physician-to-enrollee ratios or an alternative method of demonstrating network adequacy, the filing shall contain confirming documentation. A plan may concurrently request approval of alternative physician-to-enrollee ratios or an alternative method of demonstrating network adequacy by filing a notice of material modification pursuant to section 1300.67.2.1 of Title 28.
(2) By March 31, 2012, and by March 31 of each year thereafter, plans shall file with the Department a report, pursuant to subsection (f)(2) of Section 1367.03 of the Act, regarding compliance during the immediately preceding year. The first reporting period shall be the calendar year ending December 31, 2011. The reports shall document the following information:
(A) The timely access standards set forth in the plan's policies and procedures including, as may be applicable, any alternative time-elapsed standards and alternatives to time-elapsed standards for which the plan obtained the Department's prior approval by Order;
(B) The rate of compliance, during the reporting period, with the time elapsed standards set forth in subsection (c)(5), separately reported for each of the plan's contracted provider groups located in each county of the plan's service area. A plan may develop data regarding rates of compliance through statistically reliable sampling methodology, including but not limited to provider and enrollee survey processes, or through provider reporting required pursuant to subsection (f)(2) of Section 1367.03 of the Act;
(C) Whether the plan identified, during the reporting period, (1) any incidents of noncompliance resulting in substantial harm to an enrollee or (2) any patterns of non-compliance and, if so, a description of the identified non-compliance and the plan's responsive investigation, determination and corrective action;
(D) A list of all provider groups and individual providers utilizing advanced access appointment scheduling;
(E) A description of the implementation and use by the plan and its contracting providers of triage, telemedicine, and health information technology to provide timely access to care;
(F) The results of the most recent annual enrollee and provider surveys and a comparison with the results of the prior year's survey, including a discussion of the relative change in survey results; and
(G) Information confirming the status of the plan's provider network and enrollment at the time of the report, which shall include, on a county-by-county basis, in a format approved by the Department:
1. The plan's enrollment in each product line; and
2. A complete list of the plan's contracted physicians, hospitals, and other contracted providers, including location, specialty and subspecialty qualifications, California license number and National Provider Identification Number, as applicable. Physician specialty designation shall specify board certification or eligibility consistent with the specialty designations recognized by the American Board of Medical Specialties.
3. The information required by paragraphs (g)(2)(G)(1) and (2) shall be included with the annual report until the Department implements a web-based application that provides for electronic submission via a web portal designated for the collection of plan network data. Upon the Department's implementation of the designated network data collection web portal, the information required by paragraphs (G)(1) and (2), shall be submitted directly to the web portal.
(3) In determining a plan's compliance or non-compliance with the requirements of this section, the Department will focus more upon patterns of non-compliance than isolated episodes of non-compliance and may consider all relevant factors, including but not limited to:
(A) The efforts by a plan to evade the standards, such as referring enrollees to providers who are not appropriate for an enrollee's condition;
(B) The nature and extent of a plan's efforts to avoid or correct non-compliance, including whether a plan has taken all necessary and appropriate action to identify the cause(s) underlying identified timely access deficiencies and to bring its network into compliance;
(C) The nature of physician practices, including group and individual practices, the nature of a plan's network, and the nature of the health care services offered;
(D) The nature and extent to which a single instance of non-compliance results in, or contributes to, serious injury or damages to an enrollee; and
(E) Other factors established in relevant provisions of law, and other factors that the Director deems appropriate in the public interest and consistent with the intent and purpose of the Act as applied to specific facts or circumstances.
NOTE
Authority cited: Sections 1344, 1346 and 1367.03, Health and Safety Code. Reference: Sections 1342, 1367, 1367.01, 1367.03, 1370, 1375.7 and 1380, Health and Safety Code.
HISTORY
1. New section filed 12-18-2009; operative 1-17-2010 (Register 2009, No. 51).
§1300.67.04. Language Assistance Programs.
Note • History
(a) Application.
(1) Every health care service plan, including specialized health care service plans (plans), shall comply with the requirements of this section. The requirements of this section shall not apply to plan contracts for the provision of services to Medi-Cal enrollees or to contracts between plans and the federal government for the provision of services to Medicare enrollees.
(2) If a plan has both Medi-Cal and non-Medi-Cal lines of business, then the plan will be in compliance with the requirements of this section as to its non-Medi-Cal lines of business if:
(A) The Medi-Cal standards for providing language assistance services, including standards for timeliness and proficiency of interpreters, are equivalent to or exceed the standards set forth in Section 1367.04 of the Act and this section;
(B) The plan applies the Medi-Cal standards for language assistance programs to the plan's non-Medi-Cal lines of business; and
(C) The Department of Managed Health Care (Department) determines, as described in Section 1367.04(h)(3) of the Act, that the plan is in compliance with the Medi-Cal standards.
(3) A plan that seeks the Department's determination of compliance as provided in subsection (a)(2) shall request such determination as part of its filing pursuant to subsection (e)(2) and provide documentation sufficient to support and verify the request to the Department's satisfaction. The Department's determination pursuant to subsection (a)(2) shall apply only to the enrollees in a plan's non-Medi-Cal lines of business to which the plan actually applies the plan's Medi-Cal program standards.
(b) Definitions.
(1) Demographic profile means, at a minimum, identification of an enrollee's preferred spoken and written language, race and ethnicity.
(2) Interpretation: the act of listening to something spoken or reading something written in one language (source language) and orally expressing it accurately and with appropriate cultural relevance into another language (target language).
(3) Limited English Proficient or LEP Enrollee: an enrollee who has an inability or a limited ability to speak, read, write, or understand the English language at a level that permits that individual to interact effectively with health care providers or plan employees.
(4) Point of Contact: an instance in which an enrollee accesses the services covered under the plan contract, including administrative and clinical services, and telephonic and in-person contacts.
(5) Threshold Language(s): the language(s) identified by a plan pursuant to Section 1367.04(b)(1)(A) of the Act.
(6) Translation: replacement of a written text from one language (source language) with an equivalent written text in another language (target language).
(7) Vital Documents: the following documents, when produced by the plan (plan-produced documents) including when the production or distribution is delegated by a plan to a contracting health care service provider or administrative services provider:
(A) Applications;
(B) Consent forms, including any form by which an enrollee authorizes or consents to any action by the plan;
(C) Letters containing important information regarding eligibility and participation criteria;
(D) Notices pertaining to the denial, reduction, modification, or termination of services and benefits, and the right to file a grievance or appeal;
(E) Notices advising LEP enrollees of the availability of free language assistance and other outreach materials that are provided to enrollees;
(F) A plan's explanation of benefits or similar claim processing information that is sent to an enrollee if the document requires a response from the enrollee; and
(G) Subject to subsection (c)(2)(F)(ii), the enrollee disclosures required by Section 1363(a)(1), (2) and (4) of the Act.
(c) Language Assistance Program Requirements.
Every plan shall develop and implement a language assistance program, which shall comply with the requirements and standards established by Section 1367.04 of the Act and this section. The language assistance program shall be documented in written policies and procedures, and shall address, at a minimum, the following four elements: standards for enrollee assessment; standards for providing language assistance services; standards for staff training; and standards for compliance monitoring.
(1) Enrollee Assessment. Every health care service plan and specialized health care service plan shall assess its enrollee population to develop a demographic profile and to survey the linguistic needs of individual enrollees. In assessing its enrollee population each plan shall, at a minimum:
(A) Develop a demographic profile of the plan's enrollee population for the purposes of calculating threshold languages and reporting to the Department pursuant to Section 1367.07 of the Act. All plans shall apply statistically valid methods for population analysis in developing the demographic profile and plans may utilize a variety of methods for collecting demographic data for this purpose, including census data, client utilization data from third parties, data from community agencies and third party enrollment processes;
(B) Survey its enrollees in a manner designed to identify the linguistic needs of each of the plan's enrollees, and record the information provided by a responding enrollee in the enrollee's file. Plans may utilize existing processes and methods to distribute the linguistic needs survey, including but not limited to, existing enrollment and renewal processes, subscriber newsletters, mailings and other communication processes. A plan may demonstrate compliance with the survey requirement by distributing to all subscribers, including all individual subscribers under group contracts, a disclosure explaining, in English and in the plan's threshold languages, the availability of free language assistance services and how to inform the plan and relevant providers regarding the preferred spoken and written languages of the subscriber and other enrollees under the subscriber contract; and
(C) Collect, summarize and document enrollee demographic profile data in a manner that enables the plan to maintain confidentiality of personal information and to disclose the information to the Department on request for regulatory purposes and to contracting providers on request for lawful purposes, including language assistance purposes and health care quality improvement purposes. This section is not intended to limit or expand existing law regarding confidentiality of medical records.
(2) Providing Language Assistance Services. Every plan shall develop language assistance program policies and procedures, which shall describe, at a minimum, the information outlined below.
(A) All points of contact where the need for language assistance may be reasonably anticipated.
(B) The types of resources needed to provide effective language assistance to the plan's enrollees.
(C) The plan's processes for informing enrollees of the availability of language assistance services at no charge to enrollees, and how to access language assistance services. At a minimum, these processes shall include the following:
(i) Processes to promote effective identification of LEP enrollee language assistance needs at points of contact, to ensure that LEP enrollees are informed at points of contact that interpretation services are available at no cost to the LEP enrollee, and to facilitate individual enrollee access to interpretation services at points of contact.
(ii) Processes for including the notice required by Section 1367.04(b)(1)(B)(v) with all vital documents, all enrollment materials and all correspondence, if any, from the plan confirming a new or renewed enrollment. If documents are distributed in an LEP enrollee's preferred written language the notice need not be included.
(iii) Processes for including statements, in English and in threshold languages, about the availability of free language assistance services and how to access them, in or with brochures, newsletters, outreach and marketing materials and other materials that are routinely disseminated to the plan's enrollees.
(D) Processes to ensure the plan's language assistance program conforms with the requirements of section 1300.68(b)(3) and (7) of these regulations, including standards to ensure that LEP enrollees receive information regarding their rights to file a grievance and seek an independent medical review in threshold languages and through oral interpretation.
(i) All plans shall ensure that grievance forms and procedures in threshold languages are made readily available to enrollees and to contracting providers for distribution to enrollees upon request.
(ii) All plans shall inform contracting providers that informational notices explaining how enrollees may contact their plan, file a complaint with their plan, obtain assistance from the Department and seek an independent medical review are available in non-English languages through the Department's web site. The notice and translations can be obtained online at www.hmohelp.ca.gov for downloading and printing. In addition, hard copies may be requested by submitting a written request to: Department of Managed Health Care, Attention: HMO Help Notices, 980 9th Street, Suite 500, Sacramento, CA 95814.
(E) Processes to ensure that contracting providers are informed regarding the plan's standards and mechanisms for providing language assistance services at no charge to enrollees, and to ensure that LEP language needs information collected by the plan is made available to contracting providers.
(F) Processes and standards for providing translation services, including, but not limited to:
(i) A list of the threshold languages identified by the plan;
(ii) A list of the types of standardized and enrollee-specific vital documents that must be translated and the applicable standards for making translated vital documents available to subscribers and enrollees. Plans need not translate subscriber contracts, evidences of coverage and other large disclosure forms and enrollee handbooks in their entirety, but may excerpt from large documents the disclosures specified at subsection (b)(7)(G) for translation in a format that permits cost-effective and timely production and distribution, so long as there is no loss of accuracy or meaning by doing so. A plan may demonstrate compliance regarding translation of the disclosures specified at subsection (b)(7)(G) if the plan provides a standardized matrix that lists the major categories of health care services covered under the plan's subscriber contracts, together with the corresponding copayments and coinsurance, and exclusions and limitations, and disclosing any applicable deductibles and lifetime maximums, using the same sequence as the uniform matrix described at Section 1363(b)(1) of the Act.
(iii) A description of how the plan will provide or arrange for the provision of translation of vital documents at no charge to enrollees in accordance with the requirements of Section 1367.04 of the Act and this section. This subsection is not intended to prohibit or discourage a plan from providing translation of vital documents into a greater number of languages than the threshold languages;
(iv) A requirement that non-English translations of vital documents must meet the same standards required for English language versions of those documents; and
(v) A requirement that, with respect to vital documents that are not standardized, but which contain enrollee-specific information, a plan shall provide the English version together with the Department-approved written notice of the availability of interpretation and translation services and, if a translation is requested, the plan shall provide the requested translation in accordance with the requirements of Section 1367.04 of the Act and this section.
(G) Processes and standards for providing individual enrollee access to interpretation services at points of contact at no charge, including, but not limited to:
(i) A list of the non-English languages likely to be encountered among the plan's enrollees.
(ii) A requirement that the plan shall provide LEP enrollees with interpretation services for information contained in plan-produced documents.
(iii) A requirement that qualified interpretation services be offered to LEP enrollees, at no cost to the enrollee, at all points of contact, including when an enrollee is accompanied by a family member or friend that can provide interpretation services. The offer of a qualified interpreter, and the enrollee's refusal if interpretation services are declined, shall be documented in the medical record or plan file, as applicable.
(iv) When an enrollee needs interpretation services at a point of contact that occurs in a hospital, facility or provider office subject to federal or state law that requires the hospital, facility or provider office to provide interpretation services, the plan is not relieved of its obligation to comply with the requirements of Section 1367.04 of the Act or this section. Full service plans shall have reasonable processes in place to ensure that LEP enrollees can obtain the plan's assistance in arranging for the provision of timely interpretation services at all points of contact as defined at subsection (b)(4). This subsection does not prohibit a plan from incorporating into its language assistance program a contracting hospital's language assistance program if: the hospital's language assistance program provides access to interpretation services consistent with the requirements of Section 1367.04 of the Act and this section; the plan monitors for deficiencies in delivery of interpretation services by the hospital; and the plan takes appropriate corrective action to address hospital deficiencies in delivery of interpretation services to the plan's enrollees. This subsection is not intended to limit or expand any existing state or federal law.
(v) A description of the arrangements the plan will make to provide or arrange for the provision of timely interpretation services at no charge to LEP enrollees at all points of contact where language assistance is needed. For purposes of this subsection “timely” means in a manner appropriate for the situation in which language assistance is needed. Interpretation services are not timely if delay results in the effective denial of the service, benefit, or right at issue. A plan's language assistance program shall specify quality assurance standards for timely delivery of language assistance services for emergency, urgent and routine health care services, and shall include standards for coordinating interpretation services with appointment scheduling.
(vi) The range of interpretation services that will be provided to enrollees as appropriate for the particular point of contact. The range of services may include, but is not limited to:
(aa) Arranging for the availability of bilingual plan or provider staff who are trained and competent in the skill of interpreting;
(bb) Hiring staff interpreters who are trained and competent in the skill of interpreting;
(cc) Contracting with an outside interpreter service for trained and competent interpreters;
(dd) Arranging formally for the services of voluntary community interpreters who are trained and competent in the skill of interpreting; and
(ee) Contracting for telephone, videoconferencing or other telecommunications supported language interpretation services.
(vii) As used in this section, “trained and competent in the skill of interpreting,” “qualified interpretation services” and “qualified interpreter” means that the interpreter meets the plan's proficiency standards established pursuant to subsection (c)(2)((H).
(H) The plan's policies and standards for ensuring the proficiency of the individuals providing translation and interpretation services. A plan may develop and apply appropriate criteria for ensuring the proficiency of translation and interpretation services or may adopt certification by an association acceptable to the Department at the time of certification. A plan's language assistance proficiency standards shall require:
(i) A documented and demonstrated proficiency in both English and the other language;
(ii) A fundamental knowledge in both languages of health care terminology and concepts relevant to health care delivery systems; and
(iii) Education and training in interpreting ethics, conduct and confidentiality. The Department will accept plan standards for interpreter ethics, conduct, and confidentiality that adopt and apply, in full, the standards promulgated by the California Healthcare Interpreters Association or the National Council on Interpreting in Healthcare.
(3) Staff training.
Every plan shall implement a system to provide adequate training regarding the plan's language assistance program to all plan staff who have routine contact with LEP enrollees. The training shall include instruction on:
(A) Knowledge of the plan's policies and procedures for language assistance;
(B) Working effectively with LEP enrollees;
(C) Working effectively with interpreters in person and through video, telephone and other media, as may be applicable; and
(D) Understanding the cultural diversity of the plan's enrollee population and sensitivity to cultural differences relevant to delivery of health care interpretation services.
(4) Compliance Monitoring.
(A) Every plan shall monitor its language assistance program, including delegated programs, and make modifications as necessary to ensure compliance with Section 1367.04 of the Act and this section.
(d) In reviewing a plan's proposed language assistance program, the Department will evaluate the totality of the plan's language assistance program to determine whether the program as a whole provides meaningful access for LEP enrollees, and may consider relevant operational and demographic factors, including but not limited to:
(1) Whether the plan is a full service plan or specialized health care service plan;
(2) The nature of the points of contact;
(3) The frequency with which particular languages are encountered;
(4) The type of provider network and methods of health care service delivery;
(5) The variations and character of a plan's service area;
(6) The availability of translation and interpretation services and professionals;
(7) The variations in cost of language assistance services and the impact on affordability of health care coverage; and
(8) A plan's implementation of best practices and utilization of existing and emerging technologies to increase access to language assistance services, such as video interpreting programs, language translation software, collaborating with other plans to share a pool of interpreters, and other methods and technologies.
(9) Specialized dental, vision, chiropractic, acupuncture and employee assistance program plans that demonstrate adequate availability and accessibility of qualified bilingual contracted providers and office staff to provide meaningful access to LEP enrollees, will be in compliance with the requirements of subsection (c)(2)(G)(iii) and (v). For the purposes of this subsection, specialized dental, vision, chiropractic, acupuncture and employee assistance program plans may demonstrate adequate availability and accessibility of competent and qualified bilingual providers and office staff if:
(A) The plan identifies within its provider directories those contracting providers who are themselves bilingual or who employ other bilingual providers and/or office staff, based on language capability disclosure forms signed by the bilingual providers and/or office staff, attesting to their fluency in languages other than English;
(B) The plan requires all contracting providers to provide quarterly updates regarding any changes in the language capabilities of currently employed providers and/or office staff by submitting new language capability disclosure forms, and the plan updates its provider directories accordingly, and consistent with Section 1367.26 of the Act; and
(C) The plan's quality assurance audits of contracting providers confirm and document the accuracy of provider language capability disclosure forms and attestations.
(e) Implementation.
(1) Within one year of the effective date of this section, every plan shall complete the initial enrollee assessment required by Section 1367.04 of the Act and this section. Every plan shall update its assessment of enrollee language needs and enrollee demographic profile at least once every three years following the initial assessment.
(2) By July 1, 2008, every plan shall file, in accordance with Section 1352 of the Act, an amendment to its quality assurance program providing its written language assistance program policies and procedures, together with information and documents sufficient to demonstrate compliance with the requirements and standards of Section 1367.04 of the Act and this section. The filing shall include the plan's Section 1367.04(b)(1)(B)(v) notices. All materials filed with the Department that contain documents in non-English languages shall include the following minimum supporting documentation:
(i) The English version of each non-English document
(ii) An attestation by the translator or, if applicable, by an authorized officer of the organization providing translator services, outlining the qualifications of the translator making the translation and affirming that the non-English translation is an accurate translation of the English version.
(3) By January 1, 2009 every plan shall have established and implemented a language assistance program in compliance with the requirements of Section 1367.04 of the Act and this section.
(4) Every contract between a health care provider and a plan, including a specialized plan, that is issued, amended, delivered or renewed on or after January 1, 2009, shall require compliance with the plan's language assistance program standards developed pursuant to Section 1367.04 of the Act and this section.
(A) A plan shall retain financial responsibility for the implementation of the language assistance program required by Section 1367.04 of the Act and this section, except to the extent that delegated financial responsibility has been separately negotiated and specifically documented in written contracts. This subsection does not create an exception to Section 1367 of the Act and delegation shall not constitute a waiver of the plan's obligation to provide language assistance services required by Section 1367.04 of the Act and this section.
(B) Delegation to contracting providers of any part of the plan's obligation to provide language assistance services required by Section 1367.04 of the Act and this section constitutes a material change to a provider contract subject to the requirements of Section 1375.7 of the Act.
(f) The Department will periodically review plan compliance with the standards and requirements of Section 1367.04 of the Act and this section by methods that may include, but are not limited to, the medical survey process, reviews of consumer grievances and complaints to the Department's HMO Help Center, and provider complaints submitted to the Department's provider complaint line. The Department may also periodically request that plans submit information and data regarding enrollee language needs and demographic profile.
NOTE
Authority cited: Sections 1344 and 1367.04, Health and Safety Code. Reference: Sections 1259, 1342, 1363, 1365.5, 1367, 1367.04, 1367.07, 1368, 1368.01, 1370 and 1375.7, Health and Safety Code.
HISTORY
1. New section filed 1-24-2007; operative 2-23-2007 (Register 2007, No. 4).
§1300.67.05. Acts of War Exclusions.
Note • History
(a) No health care service plan contract executed or amended on or after the effective date of this regulation shall limit or exclude health care services based on a determination that the need for the health care service arose as a result of an Act of War.
(1) The term “contract” includes but is not limited to health care service plan contracts with subscribers and health care service providers.
(2) The term “Act of War” includes any act or conduct, or the prevention of an act or conduct, resulting from war, declared or undeclared, terrorism, or warlike action by any individual, government, military, sovereign group, terrorist or other organization.
(b) This regulation does not preclude a health plan from coordinating coverage of benefits with other entities.
(c) Nothing in this section shall prevent the Director from finding any exclusion or limitation of health care service or other services covered by the contract objectionable on grounds other than those set forth herein.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1345 and 1367, Health and Safety Code.
HISTORY
1. New section filed 2-14-2002 as an emergency; operative 2-14-2002 (Register 2002, No. 7). A Certificate of Compliance must be transmitted to OAL by 6-14-2002 or emergency language will be repealed by operation of law on the following day.
2. Certificate of Compliance as to 2-14-2002 order, including amendment of subsection (a), transmitted to OAL 6-6-2002 and filed 7-17-2002 (Register 2002, No. 29).
3. Editorial correction of subsection (a) (Register 2002, No. 35).
§1300.67.1. Continuity of Care.
Note • History
Within each service area of a plan, basic health care services shall be provided in a manner which provides continuity of care, including but not limited to:
(a) The availability of primary care physicians, who will be responsible for coordinating the provision of health care services to each enrollee;
(b) The encouragement of each enrollee to select a primary physician;
(c) The maintenance and ready availability of medical records, with sharing within the plan of all pertinent information relating to the health care of each enrollee;
(d) The maintenance of staff, including health professionals, administrative and other supporting staff, directly or through an adequate referral system, sufficient to assure that health care services will be provided on a timely and appropriate basis to enrollees;
(e) An adequate system of documentation of referrals to physicians or other health professionals. The monitoring of the follow up of enrollees' health care documentation shall be the responsibility of the health care service plan and associated health professionals.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1367, Health and Safety Code.
HISTORY
1. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.67.1.3. Block Transfer Filings.
Note • History
(a) Definitions. As used in this section:
(1) “Affected Enrollee” means enrollees of the plan who are assigned to a Terminated Provider Group or a Terminated Hospital.
(2) “Alternate Hospital” means a hospital that will provide services to plan enrollees in place of a Terminated Hospital.
(3) “Block Transfer” means a transfer or redirection of two thousand (2,000) or more enrollees by a plan from a Terminated Provider Group or Terminated Hospital to one or more contracting providers that takes place as a result of the termination or non-renewal of a Provider Contract.
(4) “Enrollee Transfer Notice” means a written notice that is sent to enrollees who are assigned to a Terminated Provider group or Terminated Hospital.
(5) “Provider Contract” means a contract between a plan and one or more health care providers, through which the plan arranges to provide health care services for its enrollees.
(6) “Provider Group” means a medical group, an independent practice association, or any other similar organization providing services to enrollees of a plan who are assigned to that provider group.
(7) “Receiving Provider Group” means a provider group that will provide services to Affected Enrollees in place of the current Provider Group.
(8) “Terminated Hospital” means a general acute care hospital that will no longer maintain a Provider Contract with the plan following the termination or non-renewal of a Provider Contract.
(9) “Terminated Provider” means either a Terminated Provider Group or a Terminated Hospital.
(10) “Terminated Provider Group” means a Provider Group that will no longer maintain a Provider Contract with the plan following the termination or non-renewal of a Provider Contract.
(b) For any proposed Block Transfer, a plan shall file with the Department a Block Transfer filing that includes, at minimum, all the items of information described in this subsection (b). The Block Transfer filing must be submitted to the Department at least seventy-five (75) days prior to the termination or non-renewal of any Provider Contract with a Terminated Provider Group or a Terminated Hospital.
The Block Transfer filing must be submitted in an electronic format developed by the Department and made available at the Department's website at www.hmohelp.ca.gov and must include, at minimum, all of the following information as appropriate for the type of provider involved:
(1) A form of the written notice that the plan intends to send to Affected Enrollees. The Enrollee Transfer Notice must include:
(A) The name of the Terminated Provider Group or Terminated Hospital. The plan may also add the name of the assigned physician, where appropriate.
(B) A brief explanation of why the transfer is necessary due to the termination of the contract between the plan and the Terminated Provider.
(C) The date of the pending contract termination and transfer.
(D) An explanation to the Affected Enrollee outlining the Affected Enrollee's assignment to a new Provider Group, options for selecting a physician within a new Provider Group, and applicable timeframes to make a new Provider Group selection. The explanation must include a notification to the Affected Enrollee that he or she may select a different network provider by contacting the plan as outlined in the plan's written continuity of care policy and evidence of coverage or disclosure form.
(E) A statement that the plan will send the Affected Enrollee a new member information card with the name, address and telephone number of the Receiving Provider Group and assigned physician by a specified later date, which will occur prior to the date of the contract termination. Alternatively, the plan may notify the Affected Enrollee of the name, address and telephone number of the new Provider Group and assigned physician, or Alternate Hospital, to which the Affected Enrollee will be assigned in the absence of a selection made by the enrollee.
(F) A statement that the Affected Enrollee may contact the plan's customer service department to request completion of care for an ongoing course of treatment from a Terminated Provider. This statement may include either a statement outlining the specific conditions set forth in California Health and Safety Code section 1373.96(c), or an explanation to the Affected Enrollee that his or her eligibility is conditioned upon certain factors as outlined in the plan's written continuity of care policy and evidence of coverage or disclosure form.
(G) The telephone number through which the Affected Enrollee may contact the plan for a further explanation of his or her rights to completion of care, including the plan's written continuity of care policy; and a link that an Affected Enrollee may use to obtain of a downloadable copy of the policy from the plan's website.
(H) A statement informing any enrollee of a point of service product that the Affected Enrollee may be required to pay a larger portion of costs if he or she continues to use his or her current providers, if applicable to the particular Block Transfer.
(I) The following statement in at least 8-point font:
“If you have been receiving care from a health care provider, you may have a right to keep your provider for a designated time period. Please contact your HMO's customer service department, and if you have further questions, you are encouraged to contact the Department of Managed Health Care, which protects HMO consumers, by telephone at its toll-free number 1-888-HMO-2219, or at a TDD number for the hearing impaired at 1-877-688-9891, or online at www.hmohelp.ca.gov.”
The statement may be modified to include the health care service plan's name in place of the phrase “your HMO's.”
(J) The plan shall require all contracted providers to include the statutory language required by California Health and Safety Code section 1373.65(f) in all communications to Affected Enrollees that concern the termination of a provider or a Block Transfer.
(K) Compliance with all applicable language assistance statues and regulations, including Section 1367.04 and any regulations based upon Section 1367.04.
(2) For a Terminated Hospital contract the plan shall also submit the following information:
(A) A brief explanation of the cause of the hospital redirection including whether the contract termination or non-renewal was initiated by the plan, the hospital, or by a contracting Provider Group.
(B) A copy of the notice of termination sent or received by the plan.
(C) If the contract termination will affect 50,000 or more enrollees, the relevant portions of the Provider Contract(s) that relate to continuity of care and transition of care.
(D) Either of the following two options:
1. a list of counties in which Affected Enrollees reside and the corresponding number of Affected Enrollees for each county, or
2. a list of the zip codes in which Affected Enrollees reside and the corresponding number of Affected Enrollees for each zip code.
(E) The number of Affected Enrollees assigned to the Terminated Hospital, and the number to be reassigned to each Alternate Hospital, classified by type of product (for example, commercial, Medi-Cal, Healthy Families, etc.)
(F) The number of Affected Enrollees within a 15-mile radius of the Terminated Hospital.
(G) The date that the plan anticipates it will mail the Enrollee Transfer Notification.
(H) The proposed date or dates of transfer of Affected Enrollees. If the plan intends to transfer Affected Enrollees on various dates, please explain the reason for the different transfer dates.
(I) If additional governmental departments or agencies require approval of enrollee notices regarding the transfer, provide copies of each proposed notice as well as an explanation of the status of each required approval.
(J) The identity of the Terminated Hospital and Alternate Hospital including the contract renewal or termination date for each Alternate Hospital.
(K) A listing identifying any services that are available at the Terminated Hospital that are not available at an Alternate Hospital. The plan must discuss the arrangements it has made to ensure that enrollees have an opportunity to receive those services.
(L) Based upon the data made public on the Office of Statewide Health Planning and Development's website, for each of the proposed Alternate Hospitals, provide the available bed occupancy rate for the most recently completed calendar year. If the rate is at 80% or higher, please provide justification as to the sufficiency of the Alternate Hospital's capacity to serve additional plan enrollees.
(M) The number of bed days utilized by plan enrollees at the Terminated Hospital for the most recently completed calendar year.
(N) An analysis showing the driving distance between the proposed Alternate Hospital and the Terminated Hospital.
(O) Of the primary care providers to whom Affected enrollees are currently assigned, the number and percentage of primary care providers with active admitting privileges at the Alternate Hospital(s) and the number of Affected Enrollees assigned to these primary care providers and the number and percentage of primary care providers without active admitting privileges at the Alternate Hospital(s) and the number of Affected Enrollees assigned to these primary care providers.
(P) Explain the procedure by which an Affected Enrollee who is assigned to a primary care provider who does not have active admitting privileges to the Alternate Hospital(s) will receive needed hospital care.
(Q) Of the specialists available to Affected Enrollees with active admitting privileges at the Terminated Hospital, the number and percentage with active admitting privileges at the Alternate Hospital(s). If any of these specialists will be unable to admit to the Alternate Hospital(s), disclose the specialty involved, how many specialists of that specialty, if any, will still be available to admit the Alternate Hospital(s) and explain how Affected Enrollees will receive care for that specialty at a proposed Alternate Hospital if there are an insufficient number of remaining specialists with active admitting privileges.
(R) A disclosure of any anticipated increase in costs that will be incurred by Affected Enrollees of the plan's point of service products resulting from termination of the current hospital's contract if they continue to use the Terminated Provider.
(S) Confirmation that the plan's continuity of care program, as filed with the Department, will be implemented for any Affected Enrollees.
(3) For a Provider Group contract termination, the plan shall also submit the following information:
(A) A brief explanation of the cause or circumstances of the Provider Contract termination or non-renewal, including whether the contract termination or non-renewal was initiated by the plan or the Provider Group. If the Provider Contract termination is due to a provider closure, specify whether the provider closure is due to a bankruptcy, an insolvency, a sale, ceasing business operations or the closure of a specific office site.
(B) A copy of the notice of termination sent or received by the plan.
(C) If the contract termination will affect 50,000 or more enrollees, the relevant portions of the Provider Contract(s) that relate to continuity of care and transition of care.
(D) Either of the following two options:
(i) a list of counties in which Affected Enrollees reside and the corresponding number of Affected Enrollees for each county, or
(ii) a list of the zip codes in which Affected Enrollees reside and the corresponding number of Affected Enrollees for each zip code.
(E) A listing, classified by type of product (for example, commercial, Medi-Cal, Healthy Families, etc.) that specifies the number of Affected Enrollees assigned to the Terminated Provider.
(F) The date that the plan anticipates it will mail the Enrollee Transfer Notice.
(G) The proposed date or dates of transfer. If the plan intends to transfer Affected Enrollees on various dates, please explain the reason for the different transfer dates.
(H) The plan's estimate of the percentage of Affected Enrollees who will remain with the same primary care provider after the transfer to a Receiving Provider Group.
(I) If additional governmental departments or agencies require approval of enrollee notices regarding the transfer, please provide copies of each proposed notice as well as an explanation of the status of each required approval.
(J) A matrix of proposed Receiving Provider Groups that includes the following information:
1. the identity of the Receiving Provider Group(s), including its Risk Bearing Organization (RBO) number as assigned by the Department,
2. the number of Affected Enrollees being transferred to each Receiving Provider Group listed by type of product. If the plan gives the Affected Enrollees the choice of selecting a new provider, then the plan must provide the number of Affected Enrollees to be transferred to each receiving Provider Group by default if no selections are made by the Affected Enrollees,
3. a listing of all hospitals to which Receiving Provider Groups refer Affected Enrollees, if different from the Terminated Provider Group.
(K) Confirmation that the plan's continuity of care program, as filed with the Department, will be implemented for any Affected Enrollees.
(c) Timing of Notice Requirements. For any termination or non-renewal of a Provider Contract, a plan shall mail to all Affected Enrollees an Enrollee Transfer Notice that has been approved by the Department.
(1) The Enrollee Transfer Notice must be mailed to each Affected Enrollee at least sixty (60) days prior to the date of termination or non-renewal.
(d) Notice Mailing Requirements. The plan shall send an Enrollee Transfer Notice to Affected Enrollees as follows:
(1) For Affected Enrollees enrollees who are Block Transferred from a Terminated Provider Group -- the plan shall send the notice to all Affected Enrollees assigned to the Terminated Provider Group.
(2) For Affected Enrollees who are block transferred from a Terminated Hospital -- the plan shall send the notice to all Affected Enrollees who reside within 15 miles of the Terminated Hospital.
(e) If, for any reason, a plan is unable to send all Enrollee Transfer Notice required pursuant to subsection 1300.67.1.3(c) of Title 28, California Code of Regulations, at least sixty (60) days prior to the termination or non-renewal of a Provider Contract, the plan shall submit to the Department an application for a waiver of the 60-day requirement. The application for waiver must include an explanation of the plan's reasons for being unable to meet the 60-day notice requirement and its proposal to minimize any disruption that may be caused to Affected Enrollees by the reduced notice. A waiver application may be based upon the sudden closure of a contracted provider, a notice-timing conflict with another jurisdictional agency, or other circumstances for which good-cause exists. If the Department does not approve or disapprove the waiver request within seven (7) days of its receipt of the request, the waiver will be deemed to have been approved by the Department.
(f) If, after sending Enrollee Transfer Notices a plan reaches an agreement to renew or enter into a new Provider Contract or to not terminate their Provider Contract with a Terminated Provider to which the plan had assigned enrollees, then the plan shall promptly inform the Department and convey an additional enrollee notification, either by telephone or in writing, to each Affected Enrollee. The additional enrollee notification must include:
(1) A brief explanation of the fact that the plan has reached an agreement with the Affected Enrollee's previously assigned provider.
(2) An explanation to the enrollee regarding options for either returning to the previously assigned provider, keeping the newly assigned provider, or select another participating provider from the plan's contracting provider list.
(3) An explanation to the Affected Enrollee of the procedure by which the enrollee may contact the plan to express his or her desire to return to the previously assigned provider.
(4) If the additional enrollee notice is given in writing, then the notice must include the following statement in at least 8-point font:
“If you have any questions regarding this notice please contact [Plan Name] customer service department. If you have further concerns about your provider network, you are encouraged to contact the Department of Managed Health Care by telephone at its toll-free number 1-888-HMO-2219, or at TDD number for the hearing impaired at 1-877-688-9891, or online at www.hmohelp.ca.gov.”
(5) Compliance with all applicable language assistance statutes and regulations, including Section 1367.04 and any regulations based upon Section 1367.04.
NOTE
Authority cited: Sections 1342, 1344 and 1346, Health and Safety Code. Reference: Sections 1367.04 and 1373.65, Health and Safety Code.
HISTORY
1. New section filed 8-22-2005; operative 9-21-2005 (Register 2005, No. 34).
§1300.67.2. Accessibility of Services.
Within each service area of a plan, basic health care services and specialized health care services shall be readily available and accessible to each of the plan's enrollees;
(a) The location of facilities providing the primary health care services of the plan shall be within reasonable proximity of the business or personal residences of enrollees, and so located as to not result in unreasonable barriers to accessibility.
(b) Hours of operation and provision for after-hour services shall be reasonable;
(c) Emergency health care services shall be available and accessible within the service area twenty-four hours a day, seven days a week;
(d) The ratio of enrollees to staff, including health professionals, administrative and other supporting staff, directly or through referrals, shall be such as to reasonably assure that all services offered by the plan will be accessible to enrollees on an appropriate basis without delays detrimental to the health of the enrollees. There shall be at least one full-time equivalent physician to each one thousand two hundred (1,200) enrollees and there shall be approximately one full-time equivalent primary care physician for each two thousand (2,000) enrollees, or an alternative mechanism shall be provided by the plan to demonstrate an adequate ratio of physicians to enrollees;
(e) A plan shall provide accessibility to medically required specialists who are certified or eligible for certification by the appropriate specialty board, through staffing, contracting, or referral;
(f) Each health care service plan shall have a documented system for monitoring and evaluating accessibility of care, including a system for addressing problems that develop, which shall include, but is not limited to, waiting time and appointments;
(g) A section of the health education program shall be designated to inform enrollees regarding accessibility of service in accordance with the needs of such enrollees for such information regarding that plan or area.
Subject to subsections (a) and (b) of this section, a plan may rely on the standards of accessibility set forth in Item H of Section 1300.51 and in Section 1300.67.2.
§1300.67.2.1. Geographic Accessibility Standards.
Note • History
Subject to subsections (a) and (b) of this section, a plan may rely, for the purposes of satisfying the requirements for geographic accessibility, on the standards of accessibility set forth in Item H of Section 1300.51 and in Section 1300.67.2.
(a) If, given the facts and circumstances with regard to any portion of its service area, a plan's standards of accessibility adopted pursuant to Item H of Section 1300.51 and/or Section 1300.67.2 are unreasonably restrictive, or the service area is within a county with a population of 500,000 or fewer, and is within a county that, as of January 1, 2002, has two or fewer full service health care service plans in the commercial market, the plan may propose alternative standards of accessibility for that portion of its service area. The plan shall do so by including such alternative standards in writing in its plan license application or in a notice of material modification. The plan shall also include a description of the reasons justifying the less restrictive standards based on those facts and circumstances. If the Department rejects the plan's proposal, the Department shall inform the plan of the Department's reason for doing so.
(b) If, in its review of a plan license application or a notice of material modification, the Department believes the accessibility standards set forth in Item H of Section 1300.51 and/or Section 1300.67.2 are insufficiently prescribed or articulated or are inappropriate given the facts and circumstances with regard to a portion of a plan's service area, the Department shall inform the plan that the Department will not allow application of those standards to that portion of the plan's service area. The Department shall also inform the plan of the Department's reasons for rejecting the application of those standards.
(c) The facts and circumstances to be included in a discussion of the reasons justifying the standards of accessibility proposed by the plan pursuant to subsection (a) or (b) of this section shall include, to the extent relevant, but shall not necessarily be limited to the following:
(1) whether the plan contract involved is a group health care service plan contract or an individual health care service plan contract;
(2) whether the plan contract is a full-service health care service plan contract or a specialized health care service plan contract, and if the latter, whether emergency services need not be covered;
(3) the uniqueness of the services to be offered;
(4) whether the portion of the service area involved is urban or rural;
(5) population density in the portion of the service area, including whether the service area is within a county with a population of 500,000 or fewer;
(6) whether, as of January 1, 2002, the county containing the service area had two or fewer full service health care service plans providing coverage to the entire county in the commercial market;
(7) the distribution of enrollees in the portion of the service area;
(8) the availability and distribution of primary care physicians;
(9) the availability and distribution of other types of providers;
(10) the existence of exclusive contracts in the provider community or other barriers to entry;
(11) patterns of practice in the portion of the service area;
(12) driving times;
(13) waiting times for appointments;
(14) whether the plan or any other health care service plan currently has significant operations in that portion of the service area; and
(15) other standards of accessibility that the Director deems necessary or appropriate in the public interest and consistent with the intent and purpose of the Act as applied to specific facts or circumstances.
(d) At least 30 days before a health care service plan files a notice of material modification of its license with the department in order to withdraw from a county with a population of 500,000 or fewer, the health care service plan shall hold a public meeting at a time and place reasonably calculated to facilitate attendance by affected enrollees in the county from which it intends to withdraw, and shall do all of the following:
(1) Provide notice announcing the public meeting at least 30 days prior to the public meeting to all affected enrollees, health care providers with which it contracts, the members of the board of supervisors of the affected county, the members of the city councils of cities in the affected county, and the members of the Legislature who represent the affected county.
(2) Provide notice announcing the public meeting at least 15 days prior to the public meeting in a newspaper of general circulation within the affected county.
(3) At the public meeting, allow testimony, which may be limited to a certain length of time by the health care service plan, of all interested parties.
(4) File with the department for review, no less than 30 days prior to the date of mailing or publication, the notices required under subparagraphs (1) and (2).
(e) The department may require a health care service plan that has filed to withdraw from a portion of a county with a population of fewer than 500,000 to hold a hearing for affected enrollees.
(f) A representative of the department shall attend the public meeting described in this section.
NOTE
Authority cited: Sections 1344, 1351 and 1366.1, Health and Safety Code. Reference: Sections 1366.1, 1367 and 1367.2, Health and Safety Code.
HISTORY
1. New section filed 11-30-98; operative 11-30-98 pursuant to Government Code section 11343.4(d) (Register 98, No. 49).
2. Change without regulatory effect amending subsection (a) filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
3. Change without regulatory effect amending subsection (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
4. Amendment of section heading, section and Note filed 6-10-2004; operative 7-10-2004 (Register 2004, No. 24).
§1300.67.3. Standards for Plan Organization.
Note • History
(a) The organization of each plan shall provide the capability to furnish in a reasonable and efficient manner the health care services for which subscribers and enrollees have contracted. Such organization shall include:
(1) separation of medical services from fiscal and administrative management sufficient to assure the Director that medical decisions will not be unduly influenced by fiscal and administrative management,
(2) staffing in medical and other health services, and in fiscal and administrative services sufficient to result in the effective conduct of the plan's business, and
(3) written procedures for the conduct of the business of the plan, including the provision of health care services, so as to provide effective controls.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1367, Health and Safety Code.
HISTORY
1. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Change without regulatory effect amending subsection (a)(1) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.67.4. Subscriber and Group Contracts.
Note • History
(a) All subscriber and group contracts and endorsements and amendments shall be printed legibly in not less than 8-point type and shall include at least the following:
(1) The information required to be included on disclosure forms by Section 1363(a) of the Code and
(A) the information required to be included on disclosure forms by Section 1300.63 (except subsections (2), (3), (4) and (11) of subsection (b) thereof), and required to be included on evidences of coverage by subsections (b)(2) and (c) (except subsection (16) thereof) of Section 1300.63.1, or
(B) if the plan complies with the provisions of Section 1300.63.2, the information required to be included on combined evidences of coverage and disclosure forms by Section 1300.63.2 (except subsections (1) and (4) of subsection (b) and subsections (2), (25), and (27) of subsection (c) thereof).
(2) Definitions of all terms contained in the contract.
(A) Which are defined by the Act or Chapter 1 of Title 28 of the California Code of Regulations,
(B) Which are any of the following: “pre-existing condition,” “guaranteed renewable,” or “non-cancellable,” or,
(C) Which require definition in order to be understood by a reasonable person not possessing special knowledge of law, medicine, or plans;
(D) Which specifically describes the eligibility of persons as subscribers or enrollees.
(3) Appropriate captions, in boldface type, for the following provisions: limitations, exclusions, exceptions, reductions, deductibles, copayments and other provisions which may decrease or limit benefits to, or increase costs of, any subscriber or enrollee;
(A) A benefit afforded by the contract shall not be subject to any limitation, exclusion, exception, reduction, deductible, or copayment which renders the benefit illusory.
(4) In the same section describing any particular benefit(s), any provisions described in (3) above which are applicable only to any such particular benefit(s);
(5) Provisions relating to cancellation under an appropriate caption, in boldface type, which provisions shall include:
(A) A statement of the bases for cancellation, which shall conform to Section 1365(a) of the Act and these rules;
(B) A statement of the opportunity for review of certain cancellations by the Director as provided in Section 1365(b) of the Code;
(C) A statement that, in the event of cancellation by either the plan (except in the case of fraud or deception in the use of services or facilities of the plan or knowingly permitting such fraud or deception by another) or the other party, the plan shall within 30 days return to the other part the pro rata portion of the money paid to plan which corresponds to any unexpired period for which payment had been received together with amounts due on claims, if any, less any amounts due the plan;
(D) A statement of the time when a notice of cancellation becomes effective;
(E) A statement that receipt by the plan of the proper prepaid or periodic payment after cancellation of the contract for nonpayment shall reinstate the contract as though it had never been cancelled if such payment is received on or before the due date of the succeeding prepaid or periodic payment, provided, however, that the contract may specify one or more of the following methods by which the plan may avoid such reinstatement:
1. In the notice of cancellation, the plan notifies the other party that if payment is not received within 15 days of issuance of the notice of cancellation, a new application is required and the conditions under which a new contract will be issued or the original contract reinstated; or
2. If such payment is received more than 15 days after issuance of the notice of cancellation, the plan refunds such payment within 20 business days; or
3. If such payment is received more than 15 days after issuance of the notice of cancellation, the plan issues to the other party, within 20 business days of receipt of such payment, a new contract accompanied by written notice stating clearly those respects in which the new contract differs from the cancelled contract in benefits, coverage or otherwise;
(6) A provision prohibiting the plan from increasing the amount paid by the other party, except after a period of at least 30 days from and after the postage paid mailing to the other party at the other party's most current address of record with the plan;
(7) A provision prohibiting the plan from decreasing in any manner the benefits stated in the contract, except after a period of at least 30 days from and after the postage paid mailing to the other party at the other party's most current address of record with the plan;
(8) A provision requiring the plan to provide written notice within a reasonable time to the other party of any termination or breach of contract by, or inability to perform of, any contracting provider if the other party may be materially and adversely affected thereby;
(9) A provision that (i) the plan is subject to the requirements of Chapter 2.2 of Division 2 of the Code and of Chapter 1 of Title 28 of the California Code of Regulations, and (ii) any provision required to be in the contract by either of the above shall bind the plan whether or not provided in the contract.
(10) A provision that, upon termination of a provider contract, the plan shall be liable for covered services rendered by such provider (other than for copayments as defined in subdivision (g) of Section 1345) to a subscriber or enrollee who retains eligibility under the applicable plan contract or by operation of law under the care of such provider at the time of such termination until the services being rendered to the subscriber or enrollee by such provider are completed, unless the plan makes reasonable and medically appropriate provision for the assumption of such services by a contracting provider.
(11) In the case of a group contract, a reasonable provision requiring the group contract holder to mail promptly to each subscriber a legible, true copy of any notice of cancellation of the plan contract which may be received from the plan and to provide promptly to the plan proof of such mailing and the date thereof, if the plan wishes to obligate the group contract holder in connection with the obligations imposed on the plan by Section 1300.65.
(b) For the purposes of this section:
(1) “Other party” means (i) in the case of a group contract, the group representative designated in the contract, and (ii) in the case of an individual contract, the subscriber.
(2) Any express or implied requirement of notice to the other party, in the context of a group contact, requires notice to the group representative designated in the contract and, with respect to material matters, to subscribers and enrollees under the group contract; however, a plan may fulfill any obligation imposed by this section to notify subscribers and enrollees under a group contract if it provides notice to the group representative designated in the contract, and the group contract requires the group representative to disseminate such notice to subscribers and enrollees in the group by the next regular communication to the group but in no event later than 30 days after the receipt thereof.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1367 and 1379, Health and Safety Code.
HISTORY
1. New subsection (a)(10) filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Amendment of subsection (a)(5) filed 9-27-79; effective thirtieth day thereafter (Register 79, No. 39).
3. Amendment of subsection (a) filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
4. Amendment of subsections (a)(2)(A), (a)(6), (a)(7) and (a)(9) filed 12-26-91; operative 1-27-92 (Register 92, No. 12).
5. Change without regulatory effect amending subsection (a)(5)(B) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
6. Change without regulatory effect amending subsections (a)(2)(A) and (a)(9) filed 12-22-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 51).
§1300.67.8. Contracts with Providers.
Note • History
Written contracts must be executed between the plan and each provider of health care services which regularly furnishes services under the plan. All contracts with providers shall be subject to the following requirements:
(a) A written contract shall be prepared or arranged in a manner which permits confidential treatment by the Director of payment rendered or to be rendered to the provider without concealment or misunderstanding of other terms and provisions of the contract.
(b) The contract shall require that the provider maintain such records and provide such information to the plan or to the Director as may be necessary for compliance by the plan with the provisions of the Act and the rules thereunder, that such records will be retained by the provider for at least two years, and that such obligation is not terminated upon a termination of the agreement, whether by rescission or otherwise. (See Section 1300.75.1)
(c) That the plan shall have access at reasonable times upon demand to the books, records and papers of the provider relating to the health care services provided to subscribers and enrollees, to the cost thereof, to payments received by the provider from subscribers and enrollees of the plan (or from others on their behalf), and, unless the provider is compensated on a fee-for-service basis, to the financial condition of the provider.
(d) The contract shall prohibit surcharges for covered services and shall provide that whenever the plan receives notice of any such surcharge it shall take appropriate action.
(e) The contract shall contain provisions complying with Section 1379 of the Act and requiring that, upon termination of the contract of the provider for any cause, such provider shall comply with the provisions of subdivision (a)(10) of Section 1300.67.4.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1367, 1381 and 1385, Health and Safety Code.
HISTORY
1. Amendment filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Amendment of subsection (b) filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
3. Change without regulatory effect amending subsections (a)-(b) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
4. New subsections (f)-(f)(5) filed 10-20-2003; operative 11-19-2003 (Register 2003, No. 43).
5. Repealer of subsections (f)-(f)(5) filed 1-24-2007; operative 2-23-2007 (Register 2007, No. 4).
§1300.67.10. Discrimination Prohibited. [Repealed]
History
HISTORY
1. Repealer filed 12-26-91; operative 1-27-92 (Register 92, No. 12).
§1300.67.11. Disclosure of Conflicts of Interest.
Note • History
(a) A plan shall not enter into any transaction with a person currently named in Item F of its application under Section 1300.51 (or currently named pursuant to Items 7, 8, or 9 of that application as in effect prior to the effective date of Section 1300.51.3) unless, prior thereto, each of the following conditions is met:
(1) The material facts concerning the transaction and the person's interest therein are disclosed to the governing body of the plan.
(2) The transaction is approved by a disinterested majority of the governing body.
(3) Such facts and such approval are made a part of the minutes of such governing body or, if no minutes are required of such governing body, otherwise retained as a record of the plan.
(b) A plan shall promptly give written notice to the Director if a transaction is entered into otherwise than in conformity with the terms of this section.
(c) For the purposes of this section, “governing body” means the board of directors, all general partners, the sole proprietor, the board of trustees, and any other persons occupying a similar position or performing similar functions.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1351 and 1367(h), Health and Safety Code.
HISTORY
1. Amendment of subsection (a) filed 12-17-85; effective thirtieth day thereafter (Register 85, No. 51.
2. Change without regulatory effect amending subsection (b) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.67.12. Contracts with Solicitor Firms.
Note • History
A plan shall not permit a solicitor firm to solicit enrollments or subscriptions on its behalf except pursuant to a written contract which meets all of the following minimum requirements:
(a) All funds received by the solicitor firm for the account of the plan shall at all times be segregated from the assets of the solicitor firm and shall be promptly deposited to a trust account in a state or federal bank authorized to do business in this state and insured by an appropriate federal insuring agency. “Promptly deposited” means deposited no later than the business day following receipt by the solicitor firm.
(b) All funds received by the solicitor firm for the account of the plan shall be transmitted to the plan, or to a person designated in the contract, net of actual commissions earned under the particular contract within (5) five business days after such funds are received by the solicitor firm.
(c) The solicitor firm shall comply and shall cause its principal persons and employees to comply with all applicable provisions of the Act and the rules thereunder.
(d) The solicitor firm shall promptly notify the plan of the institution of any disciplinary proceedings against it or against any of its principal persons or employees relating to any license issued to any such person by the California Insurance Commissioner.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1367, Health and Safety Code.
HISTORY
1. Amendment filed 12-20-77 as an emergency; effective upon filing (Register 77, No. 52).
2. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.67.13. Coordination of Benefits (“COB”).
Note • History
(a)(1) This rule does not require the use of COB provisions in plan contracts. If a contract contains a COB provision, the provision must be consistent with the standard provision set forth in subdivision (b), as interpreted by the “Instructions” set forth in that subdivision. COB provisions, or provisions for the reduction of benefits otherwise payable because of other coverage by whatever name designated, which are not consistent with the standard provision set forth in subdivision (b), may not be used, except that plans of coverage designed to be supplementary over the subscriber's or enrollee's underlying basic plan of coverage may provide that coverage shall be excess to that specific subscriber's or enrollee's plan of basic coverage from whatever source provided.
(2) A COB provision may not relieve a plan of a duty otherwise arising from a plan contract to deliver any health care service to any subscriber or enrollee because the subscriber or enrollee may be or is entitled to coverage for the service by any other plan or insurer.
(3) A COB provision may not result in a delay in furnishing any reasonably necessary health care service to any subscriber or enrollee pursuant to a plan contract.
(b) Standard COB Provision:
(1) Benefits Subject to This Provision
All of the benefits provided under this Plan contract are subject to this provision.
Instructions
When the contract provides both integrated Major Medical Expense Benefits and the Basic Benefits, but the COB provision applies to all or some of the benefits, use appropriate alternate wording such as: “Only the Major Medical Expense Benefits provided under this contract are subject to this provision.”
(2) Definitions
(A) “Plan” means any plan providing benefits or services for or by reason of medical or dental care or treatment, which benefits or services are provided by (i) group, blanket or franchise insurance coverage, (ii) service plan contracts, group practice, individual practice and other prepayment coverage, (iii) any coverage under labor-management trusteed plans, union welfare plans, employer organization plans, or employee benefit organization plans, and (iv) any coverage under governmental programs, and any coverage required or provided by any statute.
The term “Plan” shall be construed separately with respect to each policy, contract, or other arrangement for benefits or services and separately with respect to that portion of any such policy, contract, or other arrangement which reserves the right to take the benefits or services of other Plans into consideration in determining its benefits and that portion which does not.
(B) “This Plan” means that portion of this contract which provides the benefits that are subject to this provision.
(C) “Allowable Expense” means any necessary, reasonable, and customary item of expense at least a portion of which is covered under at least one of the Plans covering the person for whom claim is made. When a Plan provides benefits in the form of services rather than cash payments, the reasonable cash value of each service rendered shall be deemed to be both an Allowable Expense and a benefit paid.
(D) “Claim Determination Period” means a calendar year.
Instructions
The definition of a “Plan” within the COB provision of group contracts enumerates the types of coverage which the Plan may consider in determining whether other coverage exists with respect to a specific claim. The definition:
1. May not include individual or family policies, or individual or family subscriber contracts, except as otherwise provided in this special instruction.
2. May include all group policies, group subscriber contracts, selected group disability insurance contracts issued pursuant to section 10270.97 of the Insurance Code and blanket insurance contracts, except blanket insurance contracts issued pursuant to section 10270.2(b) or (e) which contain nonduplication of benefits or excess policy provisions.
3. May not include any entitlements to Medi-Cal benefits under chapter 7 (commencing with section 14000) or chapter 8 (commencing with section 14500) of part 3 of division 9 of the Welfare and Institutions Code, or benefits under the California Crippled Children Services program under section 10020 of the Welfare and Institutions Code or any other coverage provided for or required by law when, by law, its benefits are excess to any private insurance or other non-governmental program.
4. May not include the medical payment benefits customarily included in the traditional automobile contracts.
5. May include “Medicare” or any other similar governmental benefits so long as it does not expand the definition of “Allowable Expenses” beyond the hospital, medical and surgical benefits as may be provided by the government program and so long as such benefits are not by law excess to this Plan.
(3) Effect on Benefits
(A) This provision shall apply in determining the benefits as to a person covered under this Plan for any Claim Determination Period if, for the Allowable Expenses incurred as to such person during such period, the sum of:
(i) the value of the benefits that would be provided by this Plan in the absence of this provision, and
(ii) the benefits that would be payable under all other plans in the absence therein of provisions of similar purpose to this provision would exceed such Allowable Expenses.
(B) As to any Claim Determination Period to which this provision is applicable, the benefits that would be provided under this Plan in the absence of this provision for the Allowable Expenses incurred as to such person during such Claim Determination Period shall be reduced to the extent necessary so that the sum of such reduced benefits and all the benefits payable for such Allowable Expenses under all other Plans, except as provided in paragraph (3)C., shall not exceed the total of such Allowable Expenses. Benefits payable under another Plan include the benefits that would have been payable had claim been made therefor.
(C) If
(i) another Plan which is involved in paragraph (3)B. and which contains a provision coordinating its benefits with those of this Plan would, according to its rules, determine its benefits after the benefits of this Plan have been determined, and
(ii) the rules set forth in paragraph (4) would require this Plan to determine its benefits before such other Plan, then the benefits of such other Plan will be ignored for the purposes of determining the benefits under this Plan.
(4) For the purposes of paragraph (3), use the first of the following rules establishing the order of determination which applies:
(A) The benefits of a Plan which covers the person on whose expenses claim is based other than as a dependent shall be determined before the benefits of a Plan which covers such person as a dependent, except that, if the person is also a Medicare beneficiary and as a result of the rules established by Title XVIII of the Social Security Act (42 USC 1395 et seq.) and implementing regulations, Medicare is (i) secondary to the Plan covering the person as a dependent and (ii) primary to the Plan covering the person as other than a dependent (e.g., a retired employee), then the benefits of the Plan covering the person as a dependent are determined before those of the Plan covering that person as other than a dependent.
(B) Except for cases of a person for whom claim is made as a dependent child whose parents are separated or divorced, the benefits of a Plan which covers the person on whose expenses claim is based as a dependent of a person whose date of birth, excluding year of birth, occurs earlier in a calendar year, shall be determined before the benefits of a Plan which covers such person as a dependent of a person whose date of birth, excluding year of birth, occurs later in a calendar year. If either Plan does not have the provisions of this subparagraph regarding dependents, which results either in each Plan determining its benefits before the other or in each Plan determining its benefits after the other, the provisions of this subparagraph shall not apply, and the rule set forth in the Plan which does not have the provisions of this subparagraph shall determine the order of the benefits.
(C) Except as provided in subparagraph (E), in the case of a person for whom claim is made as a dependent child whose parents are separated or divorced and the parent with custody of the child has not remarried, the benefits of a Plan which covers the child as a dependent of the parent with custody of the child will be determined before the benefits of a Plan which covers the child as a dependent of the parent without custody.
(D) Except as provided in subparagraph (E), in the case of a person for whom claim is made as a dependent child whose parents are divorced and the parent with custody of the child has remarried, the benefits of a Plan which covers the child as a dependent of the parent with custody shall be determined before the benefits of a Plan which covers that child as a dependent of the stepparent, and the benefits of a Plan which covers that child as a dependent of the stepparent will be determined before the benefits of a Plan which covers that child as a dependent of the parent without custody.
(E) In the case of a person for whom claim is made as a dependent child whose parents are separated or divorced, where there is a court decree which would otherwise establish financial responsibility for the medical, dental or other health care expenses with respect to the child, then, notwithstanding subparagraphs (C) and (D), the benefits of a Plan which covers the child as a dependent of the parent with such financial responsibility shall be determined before the benefits of any other Plan which covers the child as a dependent child.
(F) Except as provided in subparagraph (G), the benefits of a Plan covering the person for whose expenses claim is based as a laid-off or retired employee, or dependent of such person, shall be determined after the benefits of any other Plan covering such person as an employee, other than a laid-off or retired employee, or dependent of such person;
(G) If either Plan does not have a provision regarding laid-off or retired employees, which results in each Plan determining its benefits after the other, then the rule under subparagraph (F) shall not apply;
(H) If a person whose coverage is provided under a right of continuation pursuant to federal or state law also is covered under another Plan, the following shall be the order of benefit determination:
(1) First, the benefits of a Plan covering the person as an employee, member, or subscriber, or as that person's dependent;
(2) Second, the benefits under continuation coverage. If the other Plan does not have the rules described above, and if, as a result, the Plans do not agree on the order of benefits, the rule under this subparagraph is ignored.
(I) When subparagraphs (A) through (H) do not establish an order of benefit determination, the benefits of a Plan which has covered the person on whose expenses claim is based for the longer period of time shall be determined before the benefits of a Plan which has covered such person the shorter period of time.
(5) When this provision operates to reduce the total amount of benefits otherwise payable as to a person covered under this Plan during any Claim Determination Period, each benefit that would be payable in the absence of this provision shall be reduced proportionately, and such reduced amount shall be charged against any applicable benefit limit of this Plan.
Instructions
1. When a claim under a Plan with a COB provision involves another Plan which also has a COB provision, the carriers involved shall use the above rules to decide the order in which the benefits payable under the respective Plans will be determined.
2. In determining the length of time an individual has been covered under a given Plan, two successive Plans of a given group shall be deemed to be one continuous Plan so long as the claimant concerned was eligible for coverage within 24 hours after the prior Plan terminated. Thus, neither a change in the amount or scope of benefits provided by a Plan, a change in the carrier insuring the Plan, nor a change from one type of Plan to another (e.g., single employer to multiple employer Plan, or vice versa, or single employer to a Taft-Hartley Welfare Plan) would constitute the start of a new Plan for purposes of this instruction.
3. If a claimant's effective date of coverage under a given Plan is subsequent to the date the carrier first contracted to provide the Plan for the
group concerned (employer, union, association, etc.), then, in the absence of specific information to the contrary, the carrier shall assume, for purposes of this instruction, that the claimant's length of time covered under that Plan shall be measured from claimant's effective date coverage. If a claimant's effective date of coverage under a given Plan is the same as the date the carrier first contracted to provide the Plan for the group concerned, then the carrier shall require the group concerned to furnish the date the claimant first became covered under the earliest of any prior Plans the group may have had. If such date is not readily available, the date the claimant first became a member of the group shall be used as the date from which to determine the length of time his coverage under that Plan has been in force.
4. It is recognized that there may be existing group plans containing provisions under which the coverage is declared to be “excess” to all other coverages, or other COB provisions not consistent with this rule. In such cases, plans are urged to use the following claims administration procedures: A group plan should pay first if it would be primary under the COB order of benefits determination. In those cases where a group plan would normally be considered secondary, the plan should make every effort to coordinate in a secondary position with benefits available through any such “excess” plans. The plan should try to secure the necessary information from the “excess” plan.
(6) Right to Receive and Release Necessary Information. For the purpose of determining the applicability of and implementing the terms of this provision of this Plan or any provision of similar purpose of any other Plan, the Plan may release to or obtain from any insurance company or other organization or person any information, with respect to any person, which the Plan deems to be necessary for such purposes. Any person claiming benefits under this Plan shall furnish such information as may be necessary to implement this provision.
(7) Facility of Payment. Whenever payments which should have been made under this Plan in accordance with this provision have been made under any other Plans, the Plan shall have the right, exercisable alone and in its sole discretion, to pay over to any organizations making such other payments any amounts it shall determine to be warranted in order to satisfy the intent of this provision, and amounts so paid shall be deemed to be benefits paid under this Plan and, to the extent of such payments, the Plan shall be fully discharged from liability under this Plan.
(8) Right of Recovery. Whenever payments have been made by this Plan with respect to Allowable Expenses in a total amount, at any time, in excess of the maximum amount of payment necessary at that time to satisfy the intent of this provision, the Plan shall have the right to recover such payments, to the extent of such excess, from one or more of the following, as the Plan shall determine: any persons to or for or with respect to whom such payments were made, any insurers, service plans or any other organizations.
(c) Contracts in force on the effective date of this rule which contain an “excess” clause, “anti-duplication” provision, or any other provision by whatever name designated under which benefits would be reduced because of other existing coverages, shall be brought into compliance with this rule by the later of the next anniversary or renewal date of the group policy or contract, or the expiration of the applicable collectively bargained contract pursuant to which they are written, if any.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 10270.98, Insurance Code.
HISTORY
1. New section filed 5-9-80; effective thirtieth day thereafter (Register 80, No. 19).
2. Repealer of former COB regulation section 1300.67.13 and adoption of new COB regulation section 1300.67.13 filed 3-9-87; effective upon filing pursuant to Government Code section 11346.2(d). Regulation approved for consistency with CCR, title 10, sections 2232.50 through 2232.59, as required by Insurance Code section 10270.98 (Register 87, No. 11).
3. Editorial correction of printing error restoring correct wording of subsection (8) of Instructions (Register 91, No. 33).
4. Amendment of subsections (b)(4)-(b)(4)(E), new subsections (b)(4)(F)-(b)(4)(H)(2), subsection relettering, and amendment of newly designated subsection (b)(4)(I) filed 8-6-93; operative 9-7-93 (Register 93, No. 32).
5. Editorial correction of printing error in History 2 (Register 93, No. 32).
§1300.67.24. Outpatient Prescription Drug Copayments, Coinsurance, Deductibles, Limitations and Exclusions.
Note • History
(a) Every health care service plan that provides coverage for outpatient prescription drug benefits shall provide coverage for all medically necessary outpatient prescription drugs except as described in this section, subject to the requirements of Health and Safety Code section 1342.7(g).
(1) Outpatient prescription drugs are self-administered drugs approved by the Federal Food and Drug Administration for sale to the public through retail or mail-order pharmacies that require prescriptions and are not provided for use on an inpatient basis. For purposes of this section “inpatient basis” has the meaning indicated in Section 1300.67(b), and “self-administered” means those drugs that need not be administered in a clinical setting or by a licensed health care provider.
(2) Coverage for outpatient prescription drugs shall also include coverage for disposable devices that are medically necessary for the administration of a covered outpatient prescription drug, such as spacers and inhalers for the administration of aerosol outpatient prescription drugs, and syringes for self-injectible outpatient prescription drugs that are not dispensed in pre-filled syringes. For purposes of this section, the term “disposable” includes devices that may be used more than once before disposal. This section does not create an obligation for a plan to provide coverage for a durable medical equipment benefit.
(b) Standards for outpatient prescription drug benefit plans
(1) A prescription drug benefit offered by a plan shall comply with the requirements of the Knox-Keene Act and the regulations promulgated by the Director of the Department of Managed Health Care, including but not limited to Sections 1342, 1343.5, 1342.7, 1363, 1363.01, 1363.03, 1363.5, 1367(e), 1367(g), 1367(h), 1367.01, 1367.20, 1367.21, 1367.22 and 1367.24 of the Act and Section 1300.67.4(a)(3)(A) of these rules.
(2) All clinical aspects of a plan's prescription drug benefit shall be developed by qualified medical and pharmacy professionals in accordance with good professional practice. The plan shall establish and document an internal process for ongoing review by qualified medical and pharmacy professionals of the clinical aspects of the prescription drug benefit, including review of limitations and exclusions, and the safety, efficacy, and utilization of outpatient prescription drugs.
(3) Plans seeking to establish limitations or exclusions on outpatient prescription drug benefits shall do so consistent with up-to-date evidence-based outcomes and current published, peer-reviewed medical and pharmaceutical literature.
(4) A plan that provides coverage for prescription drugs through a mail order pharmacy shall have written policies and procedures documenting that the plan's mail order arrangements are in compliance with the requirements of the Act and this section, and applicable California and federal laws regarding pharmacists and pharmacy services. The mail order pharmacy process shall conform effectively and efficiently with a plan's processes for prior authorization for coverage of medically necessary drugs as required by the Act, and shall include standards for timely delivery and a contingency mechanism for providing the drug if a mail order provider fails to meet the delivery standards.
(5) In reviewing copayments, coinsurance, deductibles, limitations, or exclusions for compliance with Section 1367(e) and (h) of the Act, and Section 1300.67.4(a)(3)(A) of these rules, the Department's approval or disapproval may be based upon all relevant factors, including but not limited to:
(A) The type and number of enrollees affected;
(B) The clinical efficacy of the drug(s) proposed to be limited or excluded;
(C) The availability of therapeutic equivalents or other drugs medically necessary for treatment of health conditions;
(D) The specific health plan products to which the copayment, coinsurance, deductible, limitation, or exclusion will apply;
(E) The duration of the limitation or exclusion;
(F) The rationale for the copayment, coinsurance, deductible, limitation or exclusion;
(G) The projected effect of the copayment, coinsurance, deductible, limitation, or exclusion on the affordability and accessibility of coverage;
(H) The projected comparative clinical effect, including any potential risk of adverse health outcomes, based upon utilization data and review of peer-reviewed professional literature;
(I) The overall copayment structure of the product, including whether the copayment, coinsurance, or deductible contributes to the overall out-of-pocket maximum for the product;
(J) Information regarding similar copayments, coinsurance levels, deductibles, limitations, or exclusions previously approved by the Department;
(K) Evidence-based clinical studies and professional literature;
(L) The description of the copayment, coinsurance, deductible, limitation or exclusion as compared to other benefits and products in the marketplace;
(M) Any other historical, statistical, or other information that the submitting plan considers pertinent to the request for approval of the copayments, coinsurance level, deductibles, limitation, or exclusion.
(c) Copayments, Coinsurance and Deductibles
(1) A plan's prescription drug benefit shall provide that if the pharmacy's retail price for a prescription drug is less than the applicable copayment amount, the enrollee shall not be required to pay any more than the retail price.
(2) Proposed copayment structures or ranges, coinsurance, or deductibles submitted to the Director for approval shall be based upon a methodology that is fully described and documented, and that complies with the standards set forth in this Section. A plan may use actual cost data on prescription drugs or, for contracted services or products, nationally recognized data sources used by the plan in developing the contract rates.
(3) A copayment or percentage coinsurance shall not exceed 50 percent of the cost to the plan as described in subsection (c)(5) and (6). A percentage coinsurance shall meet one of the following additional requirements:
(A) Have a maximum dollar amount cap on the percentage coinsurance that will be charged for an individual prescription;
(B) Apply towards an annual out-of-pocket maximum for the product; or
(C) Apply towards an annual out-of-pocket maximum for the prescription drug benefit.
(4) In addition to compliance with this subsection (c), copayments and coinsurances shall comply with the standards identified at subsection (b), including that they shall be reasonable so as to allow access to medically necessary outpatient prescription drugs, and the Department's determination may be based on all relevant factors as provided in subsection (b)(5).
(5) The “cost to the plan” means the actual cost incurred by the plan or its contracting provider to acquire and dispense a covered outpatient prescription drug, without subtracting or otherwise considering any copayment or coinsurance amount to be paid by enrollees. The cost to the plan may include average cost calculations as described in this section, and shall include all discounts and other prospective cost and pricing arrangements, as applicable. Plans shall account for any rebates and other retrospective cost and pricing arrangements for outpatient prescription drugs by verifying that the rebates and other retrospective cost and pricing arrangements for outpatient prescription drugs are applied by the plan to reduce costs for the plan's subscribers.
(6) Compliance with the requirement not to exceed 50 percent of the actual cost to the plan may be met by various methods including the three methods described below. A plan may propose a different method, which shall be filed with the Department prior to implementation by the plan and supported by information and documentation sufficient to satisfy the Department as to the validity of the calculation methodology.
(A) Average Cost in Each Tier. This copayment represents the average plan cost per drug in a tier and is calculated in the following manner:
1. The copayment is for one tier in a multi-tier prescription drug benefit. (EXAMPLE: the Name Brand tier.)
2. Add together the plan's cost for all the drugs in that tier. (EXAMPLE: the Name Brand tier covers X drug which costs the plan $50 per prescription, Y drug which costs $100 per prescription, and Z drug which costs the plan $75 per prescription-added together for a total cost of $225.)
3. Divide the cost determined according to 2 above by the total number of drugs in that same tier. (EXAMPLE: there are 3 drugs in the Name Brand tier which cost the plan $225, $225/3 = $75.)
4. The copayment may not exceed 50 percent of the average cost of drugs in the tier to which it applies. (EXAMPLE: 50% of $75 = $37.50. The copayment for the Name Brand tier may not exceed $37.50.)
(B) Weighted Average Cost in Each Tier. This copayment is the same as the average per tier except that the prescriptions actually covered by the plan are used in the calculation.
1. The copayment is for one tier in a multi-tier prescription benefit. (EXAMPLE: the Name Brand tier.)
2. Calculate the number of prescriptions for drugs in that tier actually covered by the plan. (EXAMPLE: the plan covered the cost of 10 prescriptions in the Name Brand tier.)
3. Add together the cost for all the drugs covered in 2 above. (EXAMPLE: the plan covered three prescriptions for X drug (3 x $50= $150), three for Y drug (3 x $100 = $300) and four for Z drug (4 x $75 = $300). $150 + $300 + $300 = $750 total cost for prescriptions in that tier covered by the plan.)
4. Divide the total cost determined according to 3 above by the number of prescriptions from step 2. (EXAMPLE: $750/10 = $75.)
5. The copayment may not exceed 50 percent of the weighted average cost of drugs in the tier to which it applies. (EXAMPLE: 50% of $75 = $37.50. The copayment for the Name Brand tier may not exceed $37.50.)
(C) Weighted Average Cost Across All Tiers. This copayment is the same as the weighted average per tier except that there is one copayment calculated using the number of prescriptions for all tiers covered by the plan.
1. The copayment is for all tiers in a multi-tier prescription benefit. (EXAMPLE: the Name Brand tier and the Generic tier.)
2. Calculate the number of prescriptions for drugs in that tier actually covered by the plan. (EXAMPLE: Ten prescriptions under the Name Brand tier (three for X drug, three for Y drug and four for Z drug, ten prescriptions under the Generic tier (three for drug A, three for drug B and four for Drug C for a total of twenty drugs.)
3. Add together the cost for all the drugs covered in 2 above. (EXAMPLE: the ten Name Brand drugs cost $750 (from previous example) plus the Generic drugs, three for A drug (3 x $5 = $15), three for B drug (3 x $10 = $30) and four for C drug (4 x $15 = $60) (Generic total = $105) ($750 + $105 = $855 cost for all the drugs covered in the Name Brand and Generic tiers.)
4. Divide the total cost across tiers determined according to 3 above by the number of prescriptions from step 2. (EXAMPLE: $855/20 = $42.75)
5. The copayment may not exceed 50 percent of the weighted average cost of drugs in all the tiers in the prescription drug benefit to which it applies. (EXAMPLE: 50% of $42.75 = $21.38. The copayment for all tiers may not exceed $21.38.)
(d) Limitations
Plans that provide coverage for outpatient prescription drug benefits may apply the following limitations:
(1) A plan may impose prior authorization requirements on prescription drug benefits, consistent with the requirements of the Act and regulations.
(2) When there is more than one drug that is appropriate for the treatment of a medical condition, a plan may require step therapy. A plan that requires step therapy shall have an expeditious process in place to authorize exceptions to step therapy when medically necessary and to conform effectively and efficiently with continuity of care requirements of the Act and regulations. In circumstances where an enrollee is changing plans, the new plan may not require the enrollee to repeat step therapy when that enrollee is already being treated for a medical condition by a prescription drug provided that the drug is appropriately prescribed and is considered safe and effective for the enrollee's condition. Nothing in this section shall preclude the new plan from imposing a prior authorization requirement pursuant to Section 1367.24 for the continued coverage of a prescription drug prescribed pursuant to step therapy imposed by the former plan, or preclude the prescribing provider from prescribing another drug covered by the new plan that is medically appropriate for the enrollee. For purposes of this section, “step therapy” means a type of protocol that specifies the sequence in which different prescription drugs for a given medical condition and medically appropriate for a particular patient are to be prescribed.
(3) A plan shall provide coverage for the medically necessary dosage and quantity of the drug prescribed for the treatment of a medical condition consistent with professionally recognized standards of practice.
(A) A plan may limit the amount of the drug dispensed at any one time to a 30-day supply or, if the treatment is for less than 30 days, for the medically necessary amount of the drug.
(B) A plan may impose a requirement that maintenance drugs be dispensed in a two months or greater supply.
(C) A plan may establish a mandatory mail order process for maintenance drugs when dispensed in a three months supply or greater quantities, but shall not impose any fees or costs for mandatory mail order prescriptions other than the applicable copayment or coinsurance. A plan shall not require an enrollee to fill a prescription by mail if the prescribed drug is not available to be filled in that manner.
(D) For purposes of this section, “maintenance drugs” means those outpatient prescription drugs that are prescribed for the enrollee on a continual basis to treat a chronic condition.
(4) Plans may require enrollees who are prescribed drugs for smoking cessation to be enrolled in or to have completed a smoking cessation program, if covered by the plan prior to or concurrent with receiving the prescription drug.
(5) Other limitations that the Department may approve pursuant to Section 1342.7 of the Act and this section.
(e) Exclusions
Plans that provide coverage for outpatient prescription drug benefits are not required to provide coverage for prescription drugs that meet the following conditions:
(1) When prescribed for cosmetic purposes. For purposes of this section “cosmetic” means drugs solely prescribed for the purpose of altering or affecting normal structures of the body to improve appearance rather than function.
(2) When prescribed solely for the treatment of hair loss, sexual dysfunction, athletic performance, cosmetic purposes, anti-aging for cosmetic purposes, and mental performance. Drugs for mental performance shall not be excluded from coverage when they are used to treat diagnosed mental illness or medical conditions affecting memory, including, but not limited to, treatment of the conditions or symptoms of dementia or Alzheimer's disease.
(3) When prescribed solely for the purposes of losing weight, except when medically necessary for the treatment of morbid obesity. Plans may require enrollees who are prescribed drugs for morbid obesity to be enrolled in a comprehensive weight loss program, if covered by the plan, for a reasonable period of time prior to or concurrent with receiving the prescription drug.
(4) When prescribed solely for the purpose of shortening the duration of the common cold.
(5) Drugs that are available over the counter. A plan shall not exclude coverage of an entire class of prescription drugs when one drug within that class becomes available over the counter. A plan that seeks to exclude coverage for an entire class of drugs when more than one drug within that class become available over the counter, shall first file a notice of material modification and obtain the Department's prior approval in accordance with Section 1342.7 of the Act and this regulation.
(6) Replacement of lost or stolen drugs.
(7) Drugs when prescribed by non-contracting providers for non-covered procedures and which are not authorized by a plan or a plan provider except when coverage is otherwise required in the context of emergency services.
(8) Other categories of prescription drugs approved by the Department pursuant to Section 1342.7 of the Act and this section.
(f) Oversight of Plan and Provider Compliance
A plan shall have written policies and procedures for its outpatient prescription drug benefits, and quality assurance systems in place for the early identification and swift correction of problems in the accessibility and availability of outpatient prescription drug benefits. A contract between a health care service plan and a prescription drug benefit provider shall include provisions, terms and conditions sufficient to ensure that the standards and requirements of this regulation are met.
(g) Implementation
(1) Any exclusion or limitation on a prescription drug benefit that is not described at subsections (d) or (e) may not be applied to any plan's prescription drug benefit unless a plan has filed a notice of material modification with the Department and received approval by Order to apply the exclusion or limitation. The Order of approval may be issued subject to specified terms and conditions, or for specified periods, as the Department may determine are necessary and appropriate. Following issuance of an Order approving an exclusion or limitation, any other licensed plan may apply the same exclusion or limitation to its prescription drug benefit if it files an amendment with the Department not less than 30 days prior to implementation of the exclusion or limitation, and represents that it is exactly the same as that previously approved by Order, provides specific reference to the Order number and date issued, and addresses any specified terms and conditions upon such Order, as applicable.
(2) A plan may meet the material modification filing requirements of subsection (g)(1) with respect to exclusions and limitations contained in contracts issued, renewed or amended on or before January 1, 2007, by filing within six months of the effective date of this regulation a report disclosing and describing all such exclusions and limitations on prescription drug benefits covered under all subscriber contracts subject to the requirements of Section 1342.7 of the Act. The Department will provide an expeditious review of the exclusions and limitations disclosed in the report.
NOTE
Authority cited: Sections 1342.7, 1344 and 1346, Health and Safety Code. Reference: Sections 1342, 1342.7, 1343.5, 1363, 1363.01, 1363.03, 1363.5, 1367, 1367.01, 1367.215, 1367.24, 1367.25, 1367.45, 1367.51, 1374.72 and 1375.1, Health and Safety Code; see also SB 842. ch.791, Stats. 2002.
HISTORY
1. New section filed 11-3-2000 as an emergency; operative 11-3-2000 (Register 2000, No. 44). A Certificate of Compliance must be transmitted to OAL by 3-5-2001 or emergency language will be repealed by operation of law on the following day.
2. Certificate of Compliance as to 11-3-2000 order transmitted to OAL 3-5-2001 and filed 4-16-2001 (Register 2001, No. 16).
3. Amendment of section heading and repealer and new section and Note filed 6-26-2006; operative 7-26-2006 (Register 2006, No. 26).
§1300.67.50. Certain Medicare Supplement Contracts: Presumption of Unfairness.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1367 and 1384(d), Health and Safety Code.
HISTORY
1. New section filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
2. Amendment of subsections (a) and (c), new subsection (d)(4), renumbering with amendment to subsections (d)(5) and (d)(6) and amendment of NOTE filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
3. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.67.51. Medicare Supplement Contract Provisions.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1367, Health and Safety Code.
HISTORY
1. New section filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
2. Amendment of subsections (a), (b)(1), (b)(10)(A), (b)(10)(N), (c)(2), (c)(4)-(6), (d)(2) and new (d)(3.1)-(vii) filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
3. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.67.52. Medicare Supplement Additional Benefit Requirements.
Note • History
NOTE
Authority cited: Sections 1344, 1367 and 1367.15, Health and Safety Code. Reference: Sections 1344, 1367 and 1367.15, Health and Safety Code.
HISTORY
1. New section filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
2. New subsection (b) and subsection renumbering, repealer of subsection (e) and new subsections (f)-(h) filed 1-8-92; operative 1-1-92 (Register 92, No. 12).
3. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.67.53. Medicare Supplement Minimum Aggregate Benefits.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1367, Health and Safety Code.
HISTORY
1. New section filed 8-12-82; effective thirtieth day thereafter (Register 82, No. 33).
2. Amendment of subsections (a), (c), (d), new subsection (e) and relettering filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
3. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.67.55. Medicare Supplement Reporting Requirements.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1346(c),1352.1 and 1367.15, Health and Safety Code; 42 U.S.C. 1395u(h)(3)(B) and 42 U.S.C. 1395ss.
HISTORY
1. New section filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.67.56. Transitional Requirements for the Conversion of Medicare Supplement Contracts to Conform to Medicare Program Revisions.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1346(c) and 1367.15, Health and Safety Code; 42 U.S.C. 1395ss.
HISTORY
1. New section filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.67.57. Format For Notices of Changes in Coverage.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1367.15, Health and Safety Code; 42 U.S.C. 1395ss.
HISTORY
1. New section filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.67.58. Participating Physician or Supplier Claims Form Requirement. (Compliance with Section 4081 of the Omnibus Budget Reconciliation Act of 1987)
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1367(h) and 1367.15, Health and Safety Code; 42 U.S.C. 1395u(h)(3)(B) and 42 U.S.C. 1395ss.
HISTORY
1. New section filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
§1300.67.59. Format for Reporting Loss Ratio Experience.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1367.15 and 1384(d), Health and Safety Code; 42 U.S.C. 1395ss.
HISTORY
1. New section filed 11-26-91; operative 12-26-91 (Register 92, No. 10).
2. Change without regulatory effect repealing section filed 9-14-92 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 38).
Article 8. Self-Policing Procedures
§1300.67.60. Standing Referral to HIV/AIDS Specialist. [Renumbered]
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1344 and 1374.16, Health and Safety Code.
HISTORY
1. New section filed 12-17-2002; operative 1-16-2003 (Register 2002, No. 51).
2. Renumbering of former section 1300.67.60 to new section 1300.74.16 filed 1-10-2008; operative 2-9-2008 (Register 2008, No. 2).
Note • History
Every health care service plan shall establish a grievance system pursuant to the requirements of Section 1368 of the Act.
(a) The grievance system shall be established in writing and provide for procedures that will receive, review and resolve grievances within 30 calendar days of receipt by the plan, or any provider or entity with delegated authority to administer and resolve the plan's grievance system. The following definitions shall apply with respect to the regulations relating to grievance systems:
(1) “Grievance” means a written or oral expression of dissatisfaction regarding the plan and/or provider, including quality of care concerns, and shall include a complaint, dispute, request for reconsideration or appeal made by an enrollee or the enrollee's representative. Where the plan is unable to distinguish between a grievance and an inquiry, it shall be considered a grievance.
(2) “Complaint” is the same as “grievance.”
(3) “Complainant” is the same as “grievant,” and means the person who filed the grievance including the enrollee, a representative designated by the enrollee, or other individual with authority to act on behalf of the enrollee.
(4) “Resolved” means that the grievance has reached a final conclusion with respect to the enrollee's submitted grievance, and there are no pending enrollee appeals within the plan's grievance system, including entities with delegated authority.
(A) If the plan has multiple internal levels of grievance resolution or appeal, all levels must be completed within 30 calendar days of the plan's receipt of the grievance.
(B) Grievances that are not resolved within 30 calendar days, or grievances referred to the Department's complaint or independent medical review system, shall be reported as “pending” grievances pursuant to subsection (f) below. Grievances referred to external review processes, such as reviews of Medicare Managed Care determinations pursuant to 42 C.F.R. Part 422, or the Medi-Cal Fair Hearing process, shall also be reported pursuant to subsection (f) until the review and any required action by the plan resulting from the review is completed.
(b) The plan's grievance system shall include the following:
(1) An officer of the plan shall be designated as having primary responsibility for the plan's grievance system whether administered directly by the plan or delegated to another entity. The officer shall continuously review the operation of the grievance system to identify any emergent patterns of grievances. The system shall include the reporting procedures in order to improve plan policies and procedures.
(2) Each plan's obligation for notifying subscribers and enrollees about the plan's grievance system shall include information on the plan's procedures for filing and resolving grievances, and the telephone number and address for presenting a grievance. The notice shall also include information regarding the Department's review process, the independent medical review system, and the Department's toll-free telephone number and website address.
(3) The grievance system shall address the linguistic and cultural needs of its enrollee population as well as the needs of enrollees with disabilities. The system shall ensure all enrollees have access to and can fully participate in the grievance system by providing assistance for those with limited English proficiency or with a visual or other communicative impairment. Such assistance shall include, but is not limited to, translations of grievance procedures, forms, and plan responses to grievances, as well as access to interpreters, telephone relay systems and other devices that aid disabled individuals to communicate. Plans shall develop and file with the Department a policy describing how they ensure that their grievance system complies with this subsection within 90 days of the effective date of this regulation.
(4) The plan shall maintain a toll-free number, or a local telephone number in each service area, for the filing of grievances.
(5) A written record shall be made for each grievance received by the plan, including the date received, the plan representative recording the grievance, a summary or other document describing the grievance, and its disposition. The written record of grievances shall be reviewed periodically by the governing body of the plan, the public policy body created pursuant to section 1300.69, and by an officer of the plan or his designee. This review shall be thoroughly documented.
(6) The plan grievance system shall ensure that assistance in filing grievances shall be provided at each location where grievances may be submitted. A “patient advocate” or ombudsperson may be used.
(7) Grievance forms and a description of the grievance procedure shall be readily available at each facility of the plan, on the plan's website, and from each contracting provider's office or facility. Grievance forms shall be provided promptly upon request.
(8) The plan shall assure that there is no discrimination against an enrollee or subscriber (including cancellation of the contract) on the grounds that the complainant filed a grievance.
(9) The grievance system shall allow enrollees to file grievances for at least 180 calendar days following any incident or action that is the subject of the enrollee's dissatisfaction.
(c) Through periodic medical surveys under Section 1380 of the Act, the Department shall periodically review the plan's grievance system, including the records of grievances received by the plan, and assess the effectiveness of the plan policies and actions taken in response to grievances.
(d) The plan shall respond to grievances as follows:
(1) A grievance system shall provide for a written acknowledgment within five (5) calendar days of receipt, except as noted in subsection (d)(8). The acknowledgment will advise the complainant that the grievance has been received, the date of receipt, and provide the name of the plan representative, telephone number and address of the plan representative who may be contacted about the grievance.
(2) The grievance system shall provide for a prompt review of grievances by the management or supervisory staff responsible for the services or operations which are the subject of the grievance.
(3) The plan's resolution, containing a written response to the grievance shall be sent to the complainant within thirty (30) calendar days of receipt, except as noted in subsection (d)(8). The written response shall contain a clear and concise explanation of the plan's decision. Nothing in this regulation requires a plan to disclose information to the grievant that is otherwise confidential or privileged by law.
(4) For grievances involving delay, modification or denial of services based on a determination in whole or in part that the service is not medically necessary, the plan shall include in its written response, the reasons for its determination. The response shall clearly state the criteria, clinical guidelines or medical policies used in reaching the determination. The plan's response shall also advise the enrollee that the determination may be considered by the Department's independent medical review system. The response shall include an application for independent medical review and instructions, including the Department's toll-free telephone number for further information and an envelope addressed to the Department of Managed Health Care, HMO Help Center, 980 Ninth Street, 5th Floor, Sacramento, CA 95814.
(5) Plan responses to grievances involving a determination that the requested service is not a covered benefit shall specify the provision in the contract, evidence of coverage or member handbook that excludes the service. The response shall either identify the document and page where the provision is found, direct the grievant to the applicable section of the contract containing the provision, or provide a copy of the provision and explain in clear concise language how the exclusion applied to the specific health care service or benefit requested by the enrollee. In addition to the notice set forth at Section 1368.02(b) of the Act, the response shall also include a notice that if the enrollee believes the decision was denied on the grounds that it was not medically necessary, the Department should be contacted to determine whether the decision is eligible for an independent medical review.
(6) Copies of grievances and responses shall be maintained by the Plan for five years, and shall include a copy of all medical records, documents, evidence of coverage and other relevant information upon which the plan relied in reaching its decision.
(7) The Department's telephone number, the California Relay Service's telephone numbers, the plan's telephone number and the Department's Internet address shall be displayed in all of the plan's acknowledgments and responses to grievances in 12-point boldface type with the statement contained in subsection (b) of Section 1368.02 of the Act.
(8) Grievances received over the telephone that are not coverage disputes, disputed health care services involving medical necessity or experimental or investigational treatment, and that are resolved by the close of the next business day, are exempt from the requirement to send a written acknowledgment and response. The plan shall maintain a log of all such grievances containing the date of the call, the name of the complainant, member identification number, nature of the grievance, nature of resolution, and the plan representative's name who took the call and resolved the grievance. The information contained in this log shall be periodically reviewed by the plan as set forth in subsection (b).
(e) The plan's grievance system shall track and monitor grievances received by the plan, or any entity with delegated authority to receive or respond to grievances. The system shall:
(1) Monitor the number of grievances received and resolved; whether the grievance was resolved in favor of the enrollee or plan; and the number of grievances pending over 30 calendar days. The system shall track grievances under categories of Commercial, Medicare and Medi-Cal/other contracts. The system shall indicate whether an enrollee grievance is pending at: (1) the plan's internal grievance system; (2) the Department's consumer complaint process; (3) the Department's Independent Medical Review system; (4) an action filed or before a trial or appellate court; or (5) other dispute resolution process. Additionally, the system shall indicate whether an enrollee grievance has been submitted to: (1) the Medicare review and appeal system; (2) the Medi-Cal fair hearing process; or (3) arbitration.
(2) The system shall be able to indicate the total number of grievances received, pending and resolved in favor of the enrollee at all levels of grievance review and to describe the issue or issues raised in grievances as (1) coverage disputes, (2) disputes involving medical necessity, (3) complaints about the quality of care and (4) complaints about access to care (including complaints about the waiting time for appointments), and (5) complaints about the quality of service, and (6) other issues.
(f) Quarterly Reports
(1) All plans shall submit a quarterly report to the Department describing grievances that were or are pending and unresolved for 30 days or more. The report shall be prepared for the quarters ending March 31st, June 30th, September 30th and December 31st of each calendar year. The report shall also contain the number of grievances referred to external review processes, such as reconsiderations of Medicare Managed Care determinations pursuant to 42 C.F.R. Part 422, the Medi-Cal fair hearing process, the Department's complaint or Independent Medical Review system, or other external dispute resolution systems, known to the plan as of the last day of each quarter.
(2) The quarterly report shall include:
(A) The licensee's name, quarter and date of the report;
(B) The total number of grievances filed by enrollees that were or are pending and unresolved for more than 30 calendar days at any time during the quarter under the categories of Commercial, Medicare, and Medi-Cal/other products offered by the plan;
(C) A brief explanation of why the grievance was not resolved in 30 days, and indicate whether the grievance was or is pending at: (1) the plan's internal grievance system; (2) the Department's consumer complaint process; (3) the Department's Independent Medical Review system; (4) court; or (5) other dispute resolution processes. Alternatively, the plan shall indicate whether the grievance was or is submitted to: (1) the Medicare review and appeal system; (2) the Medi-Cal fair hearing process; or (3) arbitration.
(D) The nature of the unresolved grievances as (1) coverage disputes; (2) disputes involving medical necessity; (3) complaints about the quality of care; (4) complaints about access to care (including complaints about the waiting time for appointments); (5) complaints about the quality of service; and (6) other issues. All issues reasonably described in the grievance shall be separately categorized.
(E) The quarterly report shall not contain personal or confidential information with respect to any enrollee.
(3) The quarterly report shall be verified by an officer authorized to act on behalf of the plan. The report shall be submitted in writing or through electronic filing to the Department's Sacramento Office to the attention of the Filing Clerk no later than 30 days after each quarter. The quarterly report shall not be filed as an amendment to the plan application.
(4) The quarterly report shall be filed in the format specified in subsection (i).
(g) An enrollee may submit a grievance to the Department. The Department shall notify the plan, and within five (5) calendar days after notification, the plan shall provide the following information to the Department:
(1) A written response to the issues raised by the grievance.
(2) A copy of the plan's original response sent to the enrollee regarding the grievance.
(3) A complete and legible copy of all medical records related to the grievance. The plan shall inform the Department if medical records were not used by the plan in resolving the grievance.
(4) A copy of the cover page and all relevant pages of the enrollee's Evidence of Coverage (EOC), with the specific applicable sections underlined. If the plan relied solely on the EOC, the plan shall notify the Department of that fact.
(5) All other information used by the plan or relevant to the resolution of the grievance.
(6) The Department may request additional information or medical records from the plan. Within five (5) calendar days of receipt of the Department's request, the plan shall forward information and records that are maintained by the plan or any contracting provider. If requested information cannot be timely forwarded to the Department, the plan's response will describe the actions being taken to obtain the information or records and when receipt is expected.
(h) Nothing in this section shall preclude an enrollee from seeking assistance directly from the Department in cases involving an imminent or serious threat to the health of the enrollee or where the Department determines an earlier review is warranted. In such cases, the Department may require the plan and contracting providers to expedite the delivery of information.
The Department may consider the failure of a plan to timely provide the requested information as evidence in favor of the enrollee's position in the Department's review of grievances submitted under subsection (b) of Section 1368 of the Act.
(i)
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1368, Health and Safety Code.
HISTORY
1. Change without regulatory effect amending subsections (d), (f) and (g) filed 2-23-96 pursuant to section 100, title 1, California Code of Regulations (Register 96, No. 8).
2. Editorial correction of subsection (e) (Register 97, No. 19).
3. Amendment of section and new Note filed 9-18-98; operative 10-18-98 (Register 98, No. 38).
4. Amendment filed 5-30-2000 as an emergency; operative 5-30-2000 (Register 2000, No. 22). A Certificate of Compliance must be transmitted to OAL by 9-27-2000 or emergency language will be repealed by operation of law on the following day.
5. Amendment filed 8-14-2000 (Regulatory Action No. 00-0807-01E) as an emergency; operative 8-14-2000 (Register 2000, No. 33). A Certificate of Compliance must be transmitted to OAL by 12-12-2000 or emergency language will be repealed by operation of law on the following day.
6. Amendment filed 8-14-2000 (Regulatory Action No. 00-0807-02E) as an emergency; operative 8-14-2000 (Register 2000, No. 33). A Certificate of Compliance must be transmitted to OAL by 12-12-2000 or emergency language will be repealed by operation of law on the following day.
7. Editorial correction of History 5 and History 6 (Register 2001, No. 2).
8. Certificate of Compliance as to 8-14-2000 order (Regulatory Action No. 00-0807-01E) transmitted to OAL 11-29-2000 and filed 1-10-2001 (Register 2001, No. 2).
9. Certificate of Compliance as to 8-14-2000 order (Regulatory Action No. 00-0807-02E), including amendments, transmitted to OAL 11-29-2000 and filed 1-10-2001 (Register 2001, No. 2).
10. Repealer and new section filed 11-12-2002; operative 12-12-2002 (Register 2002, No. 46).
§1300.68.01. Expedited Review of Grievances.
Note • History
(a) Every plan shall include in its grievance system, procedures for the expedited review of grievances involving an imminent and serious threat to the health of the enrollee, including, but not limited to, severe pain, potential loss of life, limb or major bodily function (“urgent grievances”). At a minimum, plan procedures for urgent grievances shall include:
(1) Immediate notification to the complainant of the right to contact the Department regarding the grievance. The plan shall expedite its review of the grievance when the complainant, an authorized representative, or treating physician provides notice to the plan. Notice need not be in writing, but may be accomplished by a documented telephone call.
(2) A written statement to the Department and the complainant on the disposition or pending status of the urgent grievance within three (3) calendar days of receipt of the grievance by the Plan.
(3) Consideration by the plan of the enrollee's medical condition when determining the response time.
(4) No requirement that the enrollee participate in the plan's grievance process prior to applying to the Department for review of the urgent grievance.
(b) Each plan's grievance system shall allow for the Department to contact the plan regarding urgent grievances 24 hours a day, 7 days a week. During normal work hours, the plan shall respond to the Department within 30 minutes after initial contact from the Department. During non-work hours, the plan shall respond to the Department within 1 hour after initial contact from the Department.
(1) The system established by the plan shall provide for the availability of a plan representative with authority on the plan's behalf to resolve urgent grievances and authorize the provision of health care services covered under the enrollee's plan contract in a medically appropriate and timely manner. Such authority shall include making financial decisions for expenditure of funds on behalf of the plan without first having to obtain approval from supervisors or other superiors within the plan. Nothing in this subsection shall restrict the plan representative from consulting with other plan staff on urgent grievances.
(2) Plans shall provide the Department with the following information concerning urgent grievances:
(A) A description of the system established by the plan to resolve urgent grievances. The description shall include the system's provisions for scheduling qualified plan representatives, including back-up plan representatives as necessary, to be available twenty-four (24) hours a day, seven days a week to respond to Department contacts regarding urgent grievances. Provisions for scheduling shall include the names and titles of those plan representatives who will be available under the system, their telephone numbers, and, as applicable, pager numbers, answer service numbers, voice-mail numbers, e-mail addresses, or other means for contact.
(B) A description of how the Department may access the grievance system established by the plan.
(3) If the plan revises the system established pursuant to subsection (b), the plan shall notify the Department at least thirty (30) days in advance of implementing the revisions.
(c) The plan shall notify the Department before changing or modifying any benefit or services that relates to the urgent grievance submitted to the Department pursuant to subsection (b)(1)(A) of section 1368 of the Act if the enrollee or the enrollee's representative objects to the change or modification.
NOTE
Authority cited: Section 1344, Health and Safety Code; Reference: Sections 1368 and 1368.01, Health and Safety Code.
HISTORY
1. New section filed 5-30-2000 as an emergency; operative 5-30-2000 (Register 2000, No. 22). A Certificate of Compliance must be transmitted to OAL by 9-27-2000 or emergency language will be repealed by operation of law on the following day.
2. Repealer filed 8-14-2000 (Regulatory Action No. 00-0807-01E) as an emergency; operative 8-14-2000 (Register 2000, No. 33). A Certificate of Compliance must be transmitted to OAL by 12-12-2000 or emergency language will be repealed by operation of law on the following day.
3. New section filed 8-14-2000 (Regulatory Action No. 00-0807-02E) as an emergency; operative 8-14-2000 (Register 2000, No. 33). A Certificate of Compliance must be transmitted to OAL by 12-12-2000 or emergency language will be repealed by operation of law on the following day.
4. Editorial correction of History 2 and History 3 (Register 2001, No. 2).
5. Certificate of Compliance as to 8-14-2000 order (Regulatory Action No. 00-0807-01E) transmitted to OAL 11-29-2000 and filed 1-10-2001 (Register 2001, No. 2).
6. Certificate of Compliance as to 8-14-2000 order (Regulatory Action No. 00-0807-02E), including amendment, transmitted to OAL 11-29-2000 and filed 1-10-2001 (Register 2001, No. 2).
7. Repealer and new section filed 11-12-2002; operative 12-12-2002 (Register 2002, No. 46).
Note • History
(a) For purposes of this section, the following definitions shall apply:
(1) “Bereavement services” means those services available to the surviving family members for a period of at least one year after the death of the enrollee. These services shall include an assessment of the needs of the bereaved family and the development of a care plan that meets these needs, both prior to, and following the death of the enrollee.
(2) “Hospice service” or “hospice program” means a specialized form of interdisciplinary health care that is designed to provide palliative care, alleviate the physical, emotional, social and spiritual discomforts of an enrollee who is experiencing the last phases of life due to the existence of a terminal disease, to provide supportive care to the primary care giver and the family of the hospice patient, and which meets all of the following criteria;
(A) Considers the enrollee and the enrollee's family, in addition to the enrollee, as the unit of care.
(B) Utilizes an interdisciplinary team to assess the physical, medical, psychological, social and spiritual needs of the enrollee and the enrollee's family.
(C) Requires the interdisciplinary team to develop an overall plan of care and to provide coordinated care which emphasizes supportive services, including, but not limited to, home care, pain control, and short-term inpatient services. Short-term inpatient services are intended to ensure both continuity of care and appropriateness of services for those enrollees who cannot be managed at home because of acute complications or the temporary absence of a capable primary caregiver.
(D) Provides for the palliative medical treatment of pain and other symptoms associated with a terminal disease, but does not provide for efforts to cure the disease.
(E) Provides for bereavement services following the enrollee's death to assist the family to cope with social and emotional needs associated with the death of the enrollee.
(F) Actively utilizes volunteers in the delivery of hospice services.
(G) To the extent appropriate based on the medical needs of the enrollee, provides services in the enrollee's home or primary place of residence.
(3) “Hospice” or “Hospice Agency” means an entity which provides hospice services to terminally ill persons and holds a license, currently in effect, as a hospice pursuant to Health and Safety Code section 1747 or a home health agency with federal medicare certification pursuant to Health and Safety Code sections 1726 and 1747.1.
(4) “Home health aide services” means those services providing for the personal care of the terminally ill patient and the performance of related tasks in the patient's home in accordance with the plan of care in order to increase the level of comfort and to maintain personal hygiene and a safe, healthy environment for the patient. Home health aide services shall be provided by a person who is certified by the state Department of Health Services as a home health aide pursuant to Chapter 8 of Division 2 (Section 1725 et seq.) of the Health and Safety Code.
(5) “Homemaker services” means services that assist in the maintenance of a safe and healthy environment and services to enable the enrollee to carry out the treatment plan.
(6) “Interdisciplinary team” means the hospice care team that includes, but is not limited to, the enrollee and the patient's family, a physician and surgeon, a registered nurse, a social worker, a volunteer, and a spiritual caregiver.
(7) “Medical direction” means those services provided by a licensed physician and surgeon who is charged with the responsibility of acting as a consultant to the interdisciplinary team, a consultant to the enrollee's attending physician and surgeon, as requested, with regard to pain and symptom management, and liaison with physicians and surgeons in the community. For purposes of this section, the person providing these services shall be referred to as the “medical director.”
(8) “Plan of care” means a written plan developed by the attending physician and surgeon, the medical director or physician and surgeon designee, and the interdisciplinary team that addresses the needs of an enrollee and family admitted to the hospice program. The hospice shall retain overall responsibility for the development and maintenance of the plan of care and quality of services delivered. However, nothing in this section shall be construed to limit a health care service plan's obligations with respect to its QA program as required under Section 1300.70.
(9) “Skilled nursing services” means nursing services provided by or under the supervision of a registered nurse under a plan of care developed by the interdisciplinary team and the enrollee's physician and surgeon to an enrollee and his or her family that pertain to the palliative, supportive services required by an enrollee with a terminal illness. Skilled nursing services include, but are not limited to, enrollee assessment, evaluation and case management of the medical nursing needs of the enrollee, the performance of prescribed medical treatment for pain and symptom control, the provision of emotional support to both the enrollee and his or her family, and the instruction of caregivers in providing personal care to the enrollee. Skilled nursing services shall provide for the continuity of services for the enrollee and his or her family. Skilled nursing service shall be available on a 24-hour on-call basis.
(10) “Social service/counseling services” means those counseling and spiritual services that assist the enrollee and his or her family to minimize stresses and problems that arise from social, economic, psychological, or spiritual needs by utilizing appropriate community resources, and maximize positive aspects and opportunities for growth.
(11) “Terminal disease” or “terminal illness” means a medical condition resulting in a prognosis of life of one year or less, if the disease follows its natural course. This definition is not intended to limit the ability of health plans and hospices to develop and utilize comprehensive, evidence-based medical and psychosocial criteria or “best practice” guidelines for hospice referrals that are not dependent upon an estimated time of death, that are predictive of the need and appropriateness of palliative care and that are consistent with standards among palliative care professionals.
(12) “Volunteer services” means those service provided by trained hospice volunteers who have agreed to provide service under the direction of a hospice staff member who has been designated by the hospice to provide direction to hospice volunteers. Hospice volunteers may be used to provide support and companionship to the enrollee and his or her family during the remaining days of the enrollee's life and to the surviving family following the enrollee's death.
(b) Hospice services provided pursuant to the requirements of Section 1368.2 shall comply with the following requirements:
(1) Only an entity licensed pursuant to the California Hospice Licensure Act of 1990, (Health and Safety Code Section 1745, et seq.) or a licensed home health agency with federal medicare certification (Health and Safety Code sections 1726 and 1747.1) may provide hospice services to plan enrollees, except that an entity licensed as a hospice may arrange to provide hospice services required to be provided pursuant to this section with appropriately licensed individuals or entities.
(2) Plans are required to provide to enrollees with a “terminal illness”, through their contractual arrangements with hospices, the following services, at a minimum, when the enrollee qualifies for and chooses hospice care:
(A) Interdisciplinary team care with development and maintenance of an appropriate plan of care.
(B) Skilled nursing services, certified home health aide services and homemaker services under the supervision of a qualified registered nurse.
(C) Bereavement Services.
(D) Social services/counseling services with medical social services provided by a qualified social worker. Dietary counseling, by a qualified provider, shall also be provided when needed.
(E) Medical direction with the medical director being also responsible for meeting the general medical needs of the enrollees to the extent that these needs are not met by the attending physician.
(F) Volunteer services.
(G) Short-term inpatient care arrangements.
(H) The following shall be provided to the extent reasonable and necessary for the palliation and management of terminal illness and related conditions: pharmaceuticals, medical equipment and supplies.
(I) Physical therapy, occupational therapy, and speech-language pathology services for purposes of symptom control, or to enable the enrollee to maintain activities of daily living and basic functional skills.
(c) Covered services are to be made available on a 24 hour basis to the extent necessary to meet the needs of individuals for care that is reasonable and necessary for the palliation and management of terminal illness and related conditions.
(d) Special Coverage Requirements.
(1) Periods of Crisis:
Nursing care services must be covered on a continuous basis for as much as 24 hours a day during periods of crisis as necessary to maintain an enrollee at home. Hospitalization must be covered pursuant to 1300.68.2(b)(2)(G), when the interdisciplinary team makes the determination that inpatient skilled nursing care is required at a level that cannot be provided in the home. Either homemaker or home health aide services or both may be covered on a 24 hour continuous basis during periods of crisis but the care provided during these periods must be predominantly nursing care. A period of crisis is a period in which the enrollee requires continuous care to achieve palliation or management of acute medical symptoms.
(2) Respite Care:
Respite care is short-term inpatient care provided to the enrollee only when necessary to relieve the family members or other persons caring for the enrollee. Coverage of respite care may be limited to an occasional basis and to no more than five consecutive days at a time.
(e) Every plan shall include notice of the coverage specified in subdivisions (b), (c) and (d) in the plan's evidence of coverage and disclosure form on or after January 1, 2002.
(f) All contracts between plans and hospices must be in accordance with all federal and state hospice licensure requirements.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference cited: Section 1368.2, Health and Safety Code.
HISTORY
1. New section filed 6-26-2001; operative 7-26-2001 (Register 2001, No. 26).
§1300.69. Public Policy Participation by Subscribers.
Note • History
Unless a plan complies with the requirements of the Health Maintenance Organization Act of 1973 in affording subscribers and enrollees procedures to participate in establishing the public policy of the plan, as defined in Section 1369 of the Act, it shall comply with each of the following requirements:
(a) If the plan is a corporation, either:
(1) At least one-third of its governing board shall be subscribers and/or enrollees, or
(2) There shall be established a standing committee which shall be responsible for participating in establishing public policy of the plan as defined in Section 1369 of the Act, and whose recommendations and reports are regularly and timely reported to the governing board. The governing board shall act upon such recommendations and such action shall be recorded in the board's minutes. The membership of the standing committee shall comply with each of the following:
(A) At least 51% of the members shall be subscribers and/or enrollees,
(B) At least one member shall be a member of the governing board of the plan, and
(C) At least one member shall be a provider.
(b) If the plan is a partnership, trust or unincorporated association, there shall be established a standing committee of the governing body or executive committee of the plan, which committee shall be responsible for participation in establishing public policy of the plan as defined in Section 1369 of the Act and whose recommendations and reports are regularly and timely reported to the governing body or executive committee of the plan. The governing body or executive committee of the plan shall act upon such recommendations and such action shall be recorded in its minutes. The membership of the standing committee shall comply with each of the following:
(1) At least 51% of the members shall be subscribers and/or enrollees,
(2) At least one member shall also be a member of the governing body or executive committee of the plan, and
(3) At least one member shall be a provider.
(c) If the plan is a sole proprietorship, it shall establish a standing committee which shall be responsible for participation in establishing public policy of the plan as defined in Section 1369 of the Act and whose recommendations are reported regularly and timely to the sole proprietor. The sole proprietor shall act upon such recommendations and such action shall be recorded. The membership of the standing committee shall comply with each of the following:
(1) At least 51% of the members shall be subscribers and/or enrollees,
(2) The sole proprietor shall be a member, and
(3) At least one provider shall be a member.
(d) Those individuals who fulfill the requirements stated in this section for subscriber and/or enrollee membership upon the governing body or standing committee shall be persons who are not employees of the plan, providers of health care services, subcontractors to the plan or group contract brokers, or persons financially interested in the plan.
(e) Advisory committees do not meet the requirements of subsections (a), (b) or (c).
(f) Enrollees and subscribers participating in establishing public policy shall have access to information available from the plan regarding public policy, including financial information and information about the specific nature and volume of complaints received by the plan and their disposition.
(g) In connection with the selection of enrollee and subscriber members of any governing board or standing committee, the plan shall generally consider the makeup of its enrollee and subscriber population, including but not limited to factors such as ethnic extraction, demography, occupation and geography as well as identifiable and individual group participation. Any such selection or election of enrollee or subscriber members shall be conducted on a fair and reasonable basis. This subsection does not require the plan to maintain supporting statistical data.
(h) The public policy participation procedure shall be incorporated into the bylaws or other governing documents of the plan. The terms of subscriber and enrollee members of the public policy making body shall be of reasonable length and overlap so as to provide continuity and experience in representation. A standing committee shall meet at least quarterly.
(i) The plan shall (1) in each evidence of coverage or combined evidence of coverage and disclosure form, or at least annually by other means, furnish to its subscribers and enrollees a description of its system for their participation in establishing public policy, and (2) communicate material changes affecting public policy to subscribers and enrollees.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1369, Health and Safety Code.
HISTORY
1. Amendment of subsection (i) filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.70. Health Care Service Plan Quality Assurance Program.
Note • History
(a) Intent and Regulatory Purpose.
(1) The QA program must be directed by providers and must document that the quality of care provided is being reviewed, that problems are being identified, that effective action is taken to improve care where deficiencies are identified, and that follow-up is planned where indicated.
(2) This section is not intended to set forth a prescriptive approach to QA methodology. This section is intended to afford each plan flexibility in meeting Act quality of care requirements.
(3) A plan's QA program must address service elements, including accessibility, availability, and continuity of care. A plan's QA program must also monitor whether the provision and utilization of services meets professionally recognized standards of practice.
(4) The Department's assessment of a plan's QA program will focus on:
(A) the scope of QA activities within the organization;
(B) the structure of the program itself and its relationship to the plan's administrative structure;
(C) the operation of the QA program; and
(D) the level of activity of the program and its effectiveness in identifying and correcting deficiencies in care.
(b) Quality Assurance Program Structure and Requirements.
(1) Program Structure.
To meet the requirements of the Act which require plans to continuously review the quality of care provided, each plan's quality assurance program shall be designed to ensure that:
(A) a level of care which meets professionally recognized standards of practice is being delivered to all enrollees;
(B) quality of care problems are identified and corrected for all provider entities;
(C) physicians (or in the case of specialized plans, dentists, optometrists, psychologists or other appropriate licensed professionals) who provide care to the plan's enrollees are an integral part of the QA program;
(D) appropriate care which is consistent with professionally recognized standards of practice is not withheld or delayed for any reason, including a potential financial gain and/or incentive to the plan providers, and/or others; and
(E) the plan does not exert economic pressure to cause institutions to grant privileges to health care providers that would not otherwise be granted, nor to pressure health care providers or institutions to render care beyond the scope of their training or experience.
(2) Program Requirements.
In order to meet these obligations each plan's QA program shall meet all of the following requirements:
(A) There must be a written QA plan describing the goals and objectives of the program and organization arrangements, including staffing, the methodology for on-going monitoring and evaluation of health services, the scope of the program, and required levels of activity.
(B) Written documents shall delineate QA authority, function and responsibility, and provide evidence that the plan has established quality assurance activities and that the plan's governing body has approved the QA Program. To the extent that a plan's QA responsibilities are delegated within the plan or to a contracting provider, the plan documents shall provide evidence of an oversight mechanism for ensuring that delegated QA functions are adequately performed.
(C) The plan's governing body, its QA committee, if any, and any internal or contracting providers to whom QA responsibilities have been delegated, shall each meet on a quarterly basis, or more frequently if problems have been identified, to oversee their respective QA program responsibilities. Any delegated entity must maintain records of its QA activities and actions, and report to the plan on an appropriate basis and to the plan's governing body on a regularly scheduled basis, at least quarterly, which reports shall include findings and actions taken as a result of the QA program. The plan is responsible for establishing a program to monitor and evaluate the care provided by each contracting provider group to ensure that the care provided meets professionally recognized standards of practice. Reports to the plan's governing body shall be sufficiently detailed to include findings and actions taken as a result of the QA program
and to identify those internal or contracting provider components which the QA program has identified as presenting significant or chronic quality of care issues.
(D) Implementation of the QA program shall be supervised by a designated physician(s), or in the case of specialized plans, a designated dentist(s), optometrist(s), psychologist(s) or other licensed professional provider, as appropriate.
(E) Physician, dentist, optometrist, psychologist or other appropriate licensed professional participation in QA activity must be adequate to monitor the full scope of clinical services rendered, resolve problems and ensure that corrective action is taken when indicated. An appropriate range of specialist providers shall also be involved.
(F) There must be administrative and clinical staff support with sufficient knowledge and experience to assist in carrying out their assigned QA activities for the plan and delegated entities.
(G) Medical groups or other provider entities may have active quality assurance programs which the plan may use. In all instances, however, the plan must retain responsibility for reviewing the overall quality of care delivered to plan enrollees.
If QA activities are delegated to a participating provider to ensure that each provider has the capability to perform effective quality assurance activities, the plan must do the following:
(1) Inform each provider of the plan's QA program, of the scope of that provider's QA responsibilities, and how it will be monitored by the plan.
(2) Ascertain that each provider to which QA responsibilities have been delegated has an in-place mechanism to fulfill its responsibilities, including administrative capacity, technical expertise and budgetary resources.
(3) Have ongoing oversight procedures in place to ensure that providers are fulfilling all delegated QA responsibilities.
(4) Require that standards for evaluating that enrollees receive health care consistent with professionally recognized standards of practice are included in the provider's QA program, and be assured of the entity's continued adherence to these standards.
(5) Ensure that for each provider the quality assurance/utilization review mechanism will encompass provider referral and specialist care patterns of practice, including an assessment of timely access to specialists, ancillary support services, and appropriate preventive health services based on reasonable standards established by the plan and/or delegated providers.
(6) Ensure that health services include appropriate preventive health care measures consistent with professionally recognized standards of practice. There should be screening for conditions when professionally recognized standards of practice indicate that screening should be done.
(H) A plan that has capitation or risk-sharing contracts must:
1. Ensure that each contracting provider has the administrative and financial capacity to meet its contractual obligations; the plan shall have systems in place to monitor QA functions.
2. Have a mechanism to detect and correct under-service by an at-risk provider (as determined by its patient mix), including possible under utilization of specialist services and preventive health care services.
(I) Inpatient Care.
1. A plan must have a mechanism to oversee the quality of care provided in an inpatient setting to its enrollees which monitors that:
a. providers utilize equipment and facilities appropriate to the care; and
b. if hospital services are fully capitated that appropriate referral procedures are in place and utilized for services not customarily provided at that hospital.
2. The plan may delegate inpatient QA functions to hospitals, and may rely on the hospital's existing QA system to perform QA functions. If a plan does delegate QA responsibilities to a hospital, the plan must ascertain that the hospital's quality assurance procedure will specifically review hospital services provided to the plan's enrollees, and will review services provided by plan physicians within the hospital in the same manner as other physician services are reviewed.
(c) In addition to the internal quality of care review system, a plan shall design and implement reasonable procedures for continuously reviewing the performance of health care personnel, and the utilization of services and facilities, and cost. The reasonableness of the procedures and the adequacy of the implementation thereof shall be demonstrated to the to the Department.
NOTE
Authority cited: Sections 1344 and 1370, Health and Safety Code. Reference: Section 1370, Health and Safety Code.
HISTORY
1. Amendment filed 12-20-90; operative 1-19-91 (Register 91, No. 6).
2. Editorial correction of printing error (Register 91, No. 17).
§1300.70.4. Independent Medical Reviews Experimental and Investigational Therapies.
Note • History
(a) Enrollees of a health care service plan may request an independent medical review pursuant to sections 1370.4, 1374.30 through 1374.34 of the Act and section 1300.74.30 of title 28 when the plan has denied a therapy or medical service that would otherwise be covered based on the plan's determination that the therapy or medical service is experimental or investigational. This eligibility also applies to Medicare enrollees to the extent it does not conflict with federal law.
(b) At the time of the plan's denial of coverage for experimental or investigational therapy, or denial of urgent care or emergency services, as defined in section 1300.67(g)(2), the plan shall notify the enrollee of the ability to seek independent medical review.
(1) The notification must include, at a minimum, information on the independent medical review process, an application and envelope addressed to the Department, the physician certification form and the Department's toll-free information number.
(2) Pursuant to Health and Safety Code section 1368.03(a), the Department does not require that an enrollee participate in the plan's grievance system prior to seeking independent medical review.
(c) Included with the enrollee's application to the Department for independent medical review shall be a copy of the plan or contracted provider's written denial of the therapy or medical service based on the determination that the therapy or service is experimental or investigational.
(d) A certification from the enrollee's treating physician shall be included with the application for independent medical review. The physician's certification shall be on a form from the Department entitled, “Physician Certification Experimental/ Investigational Denials” (DMHC/IMR 110-11/27/00), or contain all of the following information:
(1) The enrollee has a condition as defined in Health and Safety Code section 1370.4(a)(1):
(2) Background information including the name of the enrollee and the health plan; the physician's name, specialty, board certification, address, telephone, and fax number; whether the physician is contracted with the plan; the enrollee's medical condition; and the specific drug, device, procedure, or other therapy recommended or requested for the enrollee's medical condition.
(3) For non-contracting physicians, the certification shall also include the following:
(A) The physician's license, board-certification or board eligibility to practice in the area appropriate to treat the enrollee's condition; and,
(B) Reference to, or copies of, two documents from the medical or scientific literature, specified in section 1370.4(d) of the Act.
(4) The following statement and physician's signature: “I certify that the requested therapy is likely to be more beneficial than any standard therapy. The information provided herein is true and correct;”
(5) Where expedited review is requested the certification shall include a statement that imminent and serious threat to the health of the enrollee exists pursuant to Health and Safety Code section 1374.31, or the proposed therapy would be significantly less effective if not promptly initiated; and
(6) Attachments, including any additional references or copies of medical and/or scientific literature considered relevant to the requested therapy and any other information relevant to the request.
(e) Incomplete applications will not be referred to an independent medical review organization. However, the Department may waive this requirement in exceptional or compelling circumstances where the need for a prompt determination precludes obtaining all information in writing. In cases accepted for an urgent review, the enrollee's physician must certify in writing, at a minimum, that the enrollee has a life-threatening or seriously debilitating condition, as defined in Health and Safety Code section 1370.4(a), that the requested therapy is likely to be more beneficial to the enrollee than any available standard therapy and describe the medical and scientific evidence relied upon in making the recommendation.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1370.4, Health and Safety Code.
HISTORY
1. New section filed 11-12-2002; operative 12-12-2002 (Register 2002, No. 46).
2. Amendment of subsections (a) and (b) filed 6-17-2005; operative 7-17-2005 (Register 2005, No. 24).
§1300.71. Claims Settlement Practices.
Note • History
(a) Definitions.
(1) “Automatically” means the payment of the interest due to the provider within five (5) working days of the payment of the claim without the need for any reminder or request by the provider.
(A) If the interest payment is not sent in the same envelope as the claim payment, the plan or the plan's capitated provider shall identify the specific claim or claims for which the interest payment is made, include a statement setting forth the method for calculating the interest on each claim and document the specific interest payment made for each claim.
(B) In the event that the interest due on an individual late claim payment is less than $2.00 at the time that the claim is paid, a plan or plan's capitated provider that pays claims (hereinafter referred to as “the plan's capitated provider”) may pay the interest on that claim along with interest on other such claims within ten (10) calendar days of the close of the calendar month in which the claim was paid, provided the plan or the plan's capitated provider includes with the interest payment a statement identifying the specific claims for which the interest is paid, setting forth the method for calculating interest on each claim and documenting the specific interest payment made for each claim.
(2) “Complete claim” means a claim or portion thereof, if separable, including attachments and supplemental information or documentation, which provides: “reasonably relevant information” as defined by section (a)(10), “information necessary to determine payer liability” as defined in section (a)(11 and:
(A) For emergency services and care provider claims as defined by section 1371.35(j):
(i) the information specified in section 1371.35(c) of the Health and Safety Code; and
(ii) any state-designated data requirements included in statutes or regulations.
(B) For institutional providers:
(i) the completed UB 92 data set or its successor format adopted by the National Uniform Billing Committee (NUBC), submitted on the designated paper or electronic format as adopted by the NUBC;
(ii) entries stated as mandatory by NUBC and required by federal statute and regulations; and
(iii) any state-designated data requirements included in statutes or regulations.
(C) For dentists and other professionals providing dental services:
(i) the form and data set approved by the American Dental Association;
(ii) Current Dental Terminology (CDT) codes and modifiers; and
(iii) any state-designated data requirements included in statutes or regulations.
(D) For physicians and other professional providers:
(i) the Centers for Medicare and Medicaid Services (CMS) Form 1500 or its successor adopted by the National Uniform Claim Committee (NUCC) submitted on the designated paper or electronic format;
(ii) Current Procedural Terminology (CPT) codes and modifiers and International Classification of Diseases (ICD-9CM) codes;
(iii) entries stated as mandatory by NUCC and required by federal statute and regulations; and
(iv) any state-designated data requirements included in statutes or regulations.
(E) For pharmacists:
(i) a universal claim form and data set approved by the National Council on Prescription Drug Programs; and
(ii) any state-designated data requirements included in statutes or regulations.
(F) For providers not otherwise specified in these regulations:
(i) A properly completed paper or electronic billing instrument submitted in accordance with the plan's or the plan's capitated provider's reasonable specifications; and
(ii) any state-designated data requirements included in statutes or regulations.
(3) “Reimbursement of a Claim” means:
(A) For contracted providers with a written contract, including in-network point-of-service (POS) and preferred provider organizations (PPO): the agreed upon contract rate;
(B) For contracted providers without a written contract and non-contracted providers,except those providing services described in paragraph (C) below: the payment of the reasonable and customary value for the health care services rendered based upon statistically credible information that is updated at least annually and takes into consideration:(1) the provider's training, qualifications, and length of time in practice; (ii) the nature of the services provided; (iii) the fees usually charged by the provider; (iv) prevailing provider rates charged in the general geographic area in which the services were rendered; (v) other aspects of the economics of the medical provider's practice that are relevant; and (vi) any unusual circumstances in the case; and
(C) For non-emergency services provided by non-contracted providers to PPO and POS enrollees: the amount set forth in the enrollee's Evidence of Coverage.
(4) “Date of contest,” “date of denial” or “date of notice” means the date of postmark or electronic mark accurately setting forth the date when the contest, denial or notice was electronically transmitted or deposited in the U.S. Mail or another mail or delivery service, correctly addressed to the claimant's office or other address of record with proper postage prepaid. This definition shall not affect the presumption of receipt of mail set forth in Evidence Code Section 641.
(5) “Date of payment” means the date of postmark or electronic mark accurately setting forth the date when the payment was electronically transmitted or deposited in the U.S. Mail or another mail or delivery service, correctly addressed to the claimant's office or other address of record. To the extent that a postmark or electronic mark is unavailable to confirm the date of payment, the Department may consider, when auditing claims payment compliance, the date the check is printed and the date the check is presented for payment. This definition shall not affect the presumption of receipt of mail set forth in Evidence Code Section 641.
(6) “Date of receipt” means the working day when a claim, by physical or electronic means, is first delivered to either the plan's specified claims payment office, post office box, or designated claims processor or to the plan's capitated provider for that claim. This definition shall not affect the presumption of receipt of mail set forth in Evidence Code section 641. In the situation where a claim is sent to the incorrect party, the “date of receipt” shall be the working day when the claim, by physical or electronic means, is first delivered to the correct party responsible for adjudicating the claim.
(7) “Date of Service,” for the purposes of evaluating claims submission and payment requirements under these regulations, means:
(A) For outpatient services and all emergency services and care: the date upon which the provider delivered separately billable health care services to the enrollee.
(B) For inpatient services: the date upon which the enrollee was discharged from the inpatient facility. However, a plan and a plan's capitated provider, at a minimum, shall accept separately billable claims for inpatient services on at least a bi-weekly basis.
(8) A “demonstrable and unjust payment pattern” or “unfair payment pattern” means any practice, policy or procedure that results in repeated delays in the adjudication and correct reimbursement of provider claims.
The following practices, policies and proceduresmay constitute a basis for a finding that the plan or the plan's capitated provider has engaged in a “demonstrable and unjust payment pattern” as set forth in section (s)(4):
(A) The imposition of a Claims Filing Deadline inconsistent with section (b)(1) in three (3) or more claims over the course of any three-month period;
(B) The failure to forward at least 95% of misdirected claims consistent with sections (b)(2)(A) and (B) over the course of any three-month period;
(C) The failure to accept a late claim consistent with section (b)(4) at least 95% of the time for the affected claims over the course of any three-month period;
(D) The failure to request reimbursement of an overpayment of a claim consistent with the provisions of sections (b)(5) and (d)(3), (4), (5) and (6) at least 95% of the time for the affected claims over the course of any three-month period;
(E) The failure to acknowledge the receipt of at least 95% of claims consistent with section (c) over the course of any three-month period;
(F) The failure to provide a provider with an accurate and clear written explanation of the specific reasons for denying, adjusting or contesting a claim consistent with section (d)(1) at least 95% of the time for the affected claims over the course of any three-month period;
(G) The inclusion of contract provisions in a provider contract that requires the provider to submit medical records that are not reasonably relevant, as defined by section (a)(10), for the adjudication of a claim on three (3) or more occasions over the course of any three month period;
(H) The failure to establish, upon the Department's written request, that requests for medical records more frequently than in three percent (3%) of the claims submitted to a plan or a plan's capitated provider by all providers over any 12-month period was reasonably necessary to determine payor liability for those claims consistent with the section (a)(2). The calculation of the 3% threshold and the limitation on requests for medical records shall not apply to claims involving emergency or unauthorized services or where the plan establishes reasonable grounds for suspecting possible fraud, misrepresentation or unfair billing practices;
(I) The failure to establish, upon the Department's written request, that requests for medical records more frequently than in twenty percent (20%) of the emergency services and care professional provider claims submitted to the plan's or the plan's capitated providers for emergency room service and care over any 12-month period was reasonably necessary to determine payor liability for those claims consistent with section (a)(2). The calculation of the 20% threshold and the limitation on requests for medical records shall not apply to claims where the plan demonstrates reasonable grounds for suspecting possible fraud, misrepresentation or unfair billing practices;
(J) The failure to include the mandated contractual provisions enumerated in section (e) in three (3) or more of its contracts with either claims processing organizations and/or with plan's capitated providers over the course of any three-month period;
(K) The failure to reimburse at least 95% of complete claims with the correct payment including the automatic payment of all interest and penalties due and owing over the course of any three-month period;
(L) The failure to contest or deny a claim, or portion thereof, within the timeframes of section (h) and sections 1371 or 1371.35 of the Act at least 95% of the time for the affected claims over the course of any three-month period;
(M) The failure to provide the Information for Contracting Providers and the Fee Schedule and Other Required Information disclosures required by sections (l) and (o) to three (3) or more contracted providers over the course of any three-month period;
(N) The failure to provide three (3) or more contracted providers the required notice for Modifications to the Information for Contracting Providers and to the Fee Schedule and Other Required Information consistent with section (m) over the course of any three month period;
(O) Requiring or allowing any provider to waive any protections or to assume any obligation of the plan inconsistent with section (p) on three (3) or more occasions over the course of any three month period;
(P) The failure to provide the required Notice to Provider of Dispute Resolution Mechanism(s) consistent with section 1300.71.38(b) at least 95% of the time for the affected claims over the course of any three-month period;
(Q) The imposition of a provider dispute filing deadline inconsistent with section 1300.71.38(d) in three (3) or more affected claims over the course of any three-month period;
(R) The failure to acknowledge the receipt of at least 95% of the provider disputes it receives consistent with section 1300.71.38(e) over the course of any three-month period;
(S) The failure to comply with the Time Period for Resolution and Written Determination enumerated in section 1300.71.38(f) at least 95% of the time over the course of any three-month period; and
(T) An attempt to rescind or modify an authorization for health care services after the provider renders the service in good faith and pursuant to the authorization, inconsistent with section 1371.8, on three (3) or more occasions over the course of any three-month period.
(9) “Health Maintenance Organization” or “HMO” means a full service health care service plan that maintains a line of business that meets the criteria of Section 1373.10(b)(1)-(3).
(10) “Reasonably relevant information” means the minimum amount of itemized, accurate and material information generated by or in the possession of the provider related to the billed services that enables a claims adjudicator with appropriate training, experience, and competence in timely and accurate claims processing to determine the nature, cost, if applicable, and extent of the plan's or the plan's capitated provider's liability, if any, and to comply with any governmental information requirements.
(11) “Information necessary to determine payer liability” means the minimum amount of material information in the possession of third parties related to a provider's billed services that is required by a claims adjudicator or other individuals with appropriate training, experience, and competence in timely and accurate claims processing to determine the nature, cost, if applicable, and extent of the plan's or the plan's capitated provider's liability, if any, and to comply with any governmental information requirements.
(12) “Plan” for the purposes of this section means a licensed health care service plan and its contracted claims processing organization.
(13) “Working days” means Monday through Friday, excluding recognized federal holidays.
(b) Claim Filing Deadline.
(1) Neither the plan nor the plan's capitated provider that pays claims shall impose a deadline for the receipt of a claim that is less than 90 days for contracted providers and 180 days for non-contracted providers after the date of service, except as required by any state or federal law or regulation. If a plan or a plan's capitated provider is not the primary payer under coordination of benefits, the plan or the plan's capitated provider shall not impose a deadline for submitting supplemental or coordination of benefits claims to any secondary payer that is less than 90 days from the date of payment or date of contest, denial or notice from the primary payer.
(2) If a claim is sent to a plan that has contracted with a capitated provider that is responsible for adjudicating the claim, then the plan shall do the following:
(A) For a provider claim involving emergency service and care, the plan shall forward the claim to the appropriate capitated provider within ten (10) working days of receipt of the claim that was incorrectly sent to the plan.
(B) For a provider claim that does not involve emergency service or care: (i) if the provider that filed the claim is contracted with the plan's capitated provider, the plan within ten (10) working days of the receipt of the claim shall either: (1) send the claimant a notice of denial, with instructions to bill the capitated provider or (2) forward the claim to the appropriate capitated provider; (ii) in all other cases, the plan within ten (10) working days of the receipt of the claim incorrectly sent to the plan shall forward the claim to the appropriate capitated provider.
(3) If a claim is sent to the plan's capitated provider and the plan is responsible for adjudicating the claim, the plan's capitated provider shall forward the claim to the plan within ten (10) working days of the receipt of the claim incorrectly sent to the plan's capitated provider.
(4) A plan or a plan's capitated provider that denies a claim because it was filed beyond the claim filing deadline, shall, upon provider's submission of a provider dispute pursuant to section 1300.71.38 and the demonstration of good cause for the delay, accept, and adjudicate the claim according to Health and Safety Code section 1371 or 1371.35, which ever is applicable, and these regulations.
(5) A plan or a plan's capitated provider shall not request reimbursement for the overpayment of a claim, including requests made pursuant to Health and Safety Code Section 1371.1, unless the plan or the plan's capitated provider sends a written request for reimbursement to the provider within 365 days of the Date of Payment on the over paid claim. The written notice shall include the information specified in section (d)(3). The 365-day time limit shall not apply if the overpayment was caused in whole or in part by fraud or misrepresentation on the part of the provider.
(c) Acknowledgement of Claims. The plan and the plan's capitated provider shall identify and acknowledge the receipt of each claim, whether or not complete, and disclose the recorded date of receipt as defined by section 1300.71(a)(6) in the same manner as the claim was submitted or provide an electronic means, by phone, website, or another mutually agreeable accessible method of notification, by which the provider may readily confirm the plan's or the plan's capitated provider's receipt of the claim and the recorded date of receipt as defined by 1300.71(a)(6) as follows:
(1) In the case of an electronic claim, identification and acknowledgement shall be provided within two (2) working days of the date of receipt of the claim by the office designated to receive the claim, or
(2) In the case of a paper claim, identification and acknowledgement shall be provided within fifteen (15) working days of the date of receipt of the claim by the office designated to receive the claim.
(A) If a claimant submits a claim to a plan or a plan's capitated provider using a claims clearinghouse, the plan's or the plan's capitated provider's identification and acknowledgement to the clearinghouse within the timeframes set forth in subparagraphs (1) or (2), above, whichever is applicable, shall constitute compliance with this section.
(d) Denying, Adjusting or Contesting a Claim and Reimbursement for the Overpayment of Claims.
(1) A plan or a plan's capitated provider shall not improperly deny, adjust, or contest a claim. For each claim that is either denied, adjusted or contested, the plan or the plan's capitated provider shall provide an accurate and clear written explanation of the specific reasons for the action taken within the timeframes specified in sections (g) and (h).
(2) In the event that the plan or the plan's capitated provider requests reasonably relevant information from a provider in addition to information that the provider submits with a claim, the plan or plan's capitated provider shall provide a clear, accurate and written explanation of the necessity for the request. If the plan or the plan's capitated provider subsequently denies the claim based on the provider's failure to provide the requested medical records or other information, any dispute arising from the denial of such claim shall be handled as a provider dispute pursuant to Section 1300.71.38 of title 28.
(3) If a plan or a plan's capitated provider determines that it has overpaid a claim, it shall notify the provider in writing through a separate notice clearly identifying the claim, the name of the patient, the date of service and including a clear explanation of the basis upon which the plan or the plan's capitated provider believes the amount paid on the claim was in excess of the amount due, including interest and penalties on the claim.
(4) If the provider contests the plan's or the plan's capitated provider's notice of reimbursement of the overpayment of a claim, the provider, within 30 working days of the receipt of the notice of overpayment of a claim, shall send written notice to the plan or the plan's capitated provider stating the basis upon which the provider believes that the claim was not over paid. The plan or the plan's capitated provider shall receive and process the contested notice of overpayment of a claim as a provider dispute pursuant to Section 1300.71.38 of title 28.
(5) If the provider does not contest the plan's or the plan's capitated provider's notice of reimbursement of the overpayment of a claim, the provider shall reimburse the plan or the plan's capitated provider within 30 working days of the receipt by the provider of the notice of overpayment of a claim.
(6) A plan or a plan's capitated provider may only offset an uncontested notice of reimbursement of the overpayment of a claim against a provider's current claim submission when: (i) the provider fails to reimburse the plan or the plan's capitated provider within the timeframe of section (5) above and (ii) the provider has entered into a written contract specifically authorizing the plan or the plan's capitated provider to offset an uncontested notice of overpayment of a claim from the contracted provider's current claim submissions. In the event that an overpayment of a claim or claims is offset against a provider's current claim or claims pursuant to this section, the plan or the plan's capitated provider shall provide the provider a detailed written explanation identifying the specific overpayment or payments that have been offset against the specific current claim or claims.
(e) Contracts for Claims Payment. A plan may contract with a claims processing organization for ministerial claims processing services or contract with capitated providers that pay claims, (“plan's capitated provider”) subject to the following conditions:
(1) The plan's contract with a claims processing organization or a capitated provider shall obligate the claims processing organization or the capitated provider to accept and adjudicate claims for health care services provided to plan enrollees in accordance with the provisions of sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.38, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28.
(2) The plan's contract with the capitated provider shall require that the capitated provider establish and maintain a fair, fast and cost-effective dispute resolution mechanism to process and resolve provider disputes in accordance with the provisions of sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.38, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28, unless the plan assumes this function.
(3) The plan's contract with a claims processing organization or a capitated provider shall require:
(i) the claims processing organization and the capitated provider to submit a Quarterly Claims Payment Performance Report (“Quarterly Claims Report”) to the plan within thirty (30) days of the close of each calendar quarter. The Quarterly Claims Report shall, at a minimum, disclose the claims processing organization's or the capitated provider's compliance status with sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28;
(ii) the capitated provider to include in its Quarterly Claims Report a tabulated record of each provider dispute it received, categorized by date of receipt, and including the identification of the provider, type of dispute, disposition, and working days to resolution, as to each provider dispute received. Each individual dispute contained in a provider's bundled notice of provider dispute shall be reported separately to the plan; and
(iii) that each Quarterly Claims Report be signed by and include the written verification of a principal officer, as defined by section 1300.45(o), of the claims processing organization or the capitated provider, stating that the report is true and correct to the best knowledge and belief of the principal officer.
(4) The plan's contract with a capitated provider shall require the capitated provider to make available to the plan and the Department all records, notes and documents regarding its provider dispute resolution mechanism(s) and the resolution of its provider disputes.
(5) The plan's contract with a capitated provider shall provide that any provider that submits a claim dispute to the plan's capitated provider's dispute resolution mechanism(s) involving an issue of medical necessity or utilization review shall have an unconditional right of appeal for that claim dispute to the plan's dispute resolution process for a de novo review and resolution for a period of 60 working days from the capitated provider's Date of Determination, pursuant to the provisions of section 1300.71.38(a)(4) of title 28.
(6) The plan's contract with a claims processing organization or the capitated provider shall include provisions authorizing the plan to assume responsibility for the processing and timely reimbursement of provider claims in the event that the claims processing organization or the capitated provider fails to timely and accurately reimburse its claims (including the payment of interest and penalties). The plan's obligation to assume responsibility for the processing and timely reimbursement of a capitated provider's provider claims may be altered to the extent that the capitated provider has established an approved corrective action plan consistent with section 1375.4(b)(4) of the Health and Safety Code.
(7) The plan's contract with the capitated provider shall include provisions authorizing a plan to assume responsibility for the administration of the capitated provider's dispute resolution mechanism(s) and for the timely resolution of provider disputes in the event that the capitated provider fails to timely resolve its provider disputes including the issuance of a written decision.
(8) The plan's contract with a claims processing organization or a capitated provider shall not relieve the plan of its obligations to comply with sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28.
(f) Disclosures.
(1) A plan or a plan's capitated provider, with the agreement of the contracted provider, may utilize alternate transmission methods to deliver any disclosure required by this regulation so long as the contracted provider can readily determine and verify that the required disclosures have been transmitted or are accessible and the transmission method complies with all applicable state and federal laws and regulations.
(2) To the extent that the Health Insurance Portability and Accountability Act of 1996, as amended, limits the plan's or the plan's capitated provider's ability to electronically transmit any required disclosures under this regulation, the plan or the plan's capitated provider shall supplement its electronic transmission with a paper communication that satisfies the disclosure requirements.
(g) Time for Reimbursement. A plan and a plan's capitated provider shall reimburse each complete claim, or portion thereof, whether in state or out of state, as soon as practical, but no later than thirty (30) working days after the date of receipt of the complete claim by the plan or the plan's capitated provider, or if the plan is a health maintenance organization, 45 working days after the date of receipt of the complete claim by the plan or the plan's capitated provider, unless the complete claim or portion thereof is contested or denied, as provided in subdivision (h).
(1) To the extent that a full service health care service plan that meets the definition of an HMO as set forth in paragraph 1300.71(a)(9) also maintains a PPO or POS line of business, the plan shall reimburse all claims relating to or arising out of non-HMO lines of business within thirty (30) working days.
(2) If a specialized health care service plan contracts with a plan that is a health maintenance organization to deliver, furnish or otherwise arrange for or provide health care services for that plan's enrollees, the specialized plan shall reimburse complete claims received for those services within thirty (30) working days.
(3) If a non-contracted provider disputes the appropriateness of a plan's or a plan's capitated provider's computation of the reasonable and customary value, determined in accordance with section (a)(3)(B), for the health care services rendered by the non-contracted provider, the plan or the plan's capitated provider shall receive and process the non-contracted provider's dispute as a provider dispute in accordance with section 1300.71.38.
(4) Every plan contract with a provider shall include a provision stating that except for applicable co-payments and deductibles, a provider shall not invoice or balance bill a plan's enrollee for the difference between the provider's billed charges and the reimbursement paid by the plan or the plan's capitated provider for any covered benefit.
(h) Time for Contesting or Denying Claims. A plan and a plan's capitated provider may contest or deny a claim, or portion thereof, by notifying the provider, in writing, that the claim is contested or denied, within thirty (30) working days after the date of receipt of the claim by the plan and the plan's capitated provider, or if the plan is a health maintenance organization, 45 working days after the date of receipt of the claim by the plan or the plan's capitated provider.
(1) To the extent that a full service health care service plan that meets the definition of an HMO as set forth in paragraph 1300.71(a)(9) also maintains a PPO or POS line of business, the plan shall contest or deny claims relating to or arising out of non-HMO lines of business within thirty (30) working days.
(2) If a specialized health care service plan contracts with a plan that is a health maintenance organization to deliver, furnish or otherwise arrange for or provide health care services for that plan's enrollees, the specialized plan shall contest or denied claims received for those services within thirty (30) working days.
(3) A request for information necessary to determine payer liability from a third party shall not extend the Time for Reimbursement or the Time for Contesting or Denying Claims as set forth in sections (g) and (h) of this regulation. Incomplete claims and claims for which “information necessary to determine payer liability” that has been requested, which are held or pended awaiting receipt of additional information shall be either contested or denied in writing within the timeframes set forth in this section. The denial or contest shall identify the individual or entity that was requested to submit information, the specific documents requested and the reason(s) why the information is necessary to determine payer liability
(i) Interest on the Late Payment of Claims.
(1) Late payment on a complete claim for emergency services and care, which is neither contested nor denied, shall automatically include the greater of $15 for each 12-month period or portion thereof on a non-prorated basis, or interest at the rate of 15 percent per annum for the period of time that the payment is late.
(2) Late payments on all other complete claims shall automatically include interest at the rate of 15 percent per annum for the period of time that the payment is late.
(j) Penalty for Failure to Automatically Include the Interest Due on a Late Claim Payment as set forth in section (i). A plan or a plan's capitated provider that fails to automatically include the interest due on a late claim payment shall pay the provider $10 for that late claim in addition to any amounts due pursuant to section (i).
(k) Late Notice or Frivolous Requests. If a plan or a plan's capitated provider fails to provide the claimant with written notice that a claim has been contested or denied within the allowable time period prescribed in section (h), or requests information from the provider that is not reasonably relevant or requests information from a third party that is in excess of the information necessary to determine payor liability as defined in section (a)(11), but ultimately pays the claim in whole or in part, the computation of interest or imposition of penalty pursuant to sections (i) and (j) shall begin with the first calendar day after the expiration of the Time for Reimbursement as defined in section (g).
(l) Information for Contracting Providers. On or before January 1, 2004, (unless the plan and/or the plan's capitated provider confirms in writing that current information is in the contracted provider's possession), initially upon contracting and in addition, upon the contracted provider's written request, the plan and the plan's capitated provider shall disclose to its contracting providers the following information in a paper or electronic format, which may include a website containing this information, or another mutually agreeable accessible format:
(1) Directions (including the mailing address, email address and facsimile number) for the electronic transmission (if available), physical delivery and mailing of claims, all claim submission requirements including a list of commonly required attachments, supplemental information and documentation consistent with section (a)(10), instructions for confirming the plan's or the plan's capitated provider's receipt of claims consistent with section (c), and a phone number for claims inquiries and filing information;
(2) The identity of the office responsible for receiving and resolving provider disputes;
(3) Directions (including the mailing address, email address and facsimile number) for the electronic transmission (if available), physical delivery, and mailing of provider disputes and all claim dispute requirements, the timeframe for the plan's and the plan's capitated provider's acknowledgement of the receipt of a provider dispute and a phone number for provider dispute inquiries and filing information; and
(4) Directions for filing substantially similar multiple claims disputes and other billing or contractual disputes in batches as a single provider dispute that includes a numbering scheme identifying each dispute contained in the bundled notice.
(m) Modifications to the Information for Contracting Providers and to the Fee Schedules and Other Required Information. A plan and a plan's capitated provider shall provide a minimum of 45 days prior written notice before instituting any changes, amendments or modifications in the disclosures made pursuant to paragraphs (l) and (o).
(n) Notice to the Department. Within 7 calendar days of a Department request, the plan and the plan's capitated providers shall provide a pro forma copy of the plan's and the plan's capitated provider's “Information to Contracting Providers” and “Modification to the Information for Contracting Providers.”
(o) Fee Schedules and Other Required Information. On or before January 1, 2004, (unless the plan and/or the plan's capitated provider confirms in writing that current information is in the contracted provider's possession), initially upon contracting, annually thereafter on or before the contract anniversary date, and in addition upon the contracted provider's written request, the plan and the plan's capitated provider shall disclose to contracting providers the following information in an electronic format:
(1) The complete fee schedule for the contracting provider consistent with the disclosures specified in section 1300.75.4.1(b); and
(2) The detailed payment policies and rules and non-standard coding methodologies used to adjudicate claims, which shall, unless otherwise prohibited by state law:
(A) when available, be consistent with Current Procedural Terminology (CPT), and standards accepted by nationally recognized medical societies and organizations, federal regulatory bodies and major credentialing organizations;
(B) clearly and accurately state what is covered by any global payment provisions for both professional and institutional services, any global payment provisions for all services necessary as part of a course of treatment in an institutional setting, and any other global arrangements such as per diem hospital payments, and
(C) at a minimum, clearly and accurately state the policies regarding the following: (i) consolidation of multiple services or charges, and payment adjustments due to coding changes, (ii) reimbursement for multiple procedures, (iii) reimbursement for assistant surgeons, (iv) reimbursement for the administration of immunizations and injectable medications, and (v) recognition of CPT modifiers.
The information disclosures required by this section shall be in sufficient detail and in an understandable format that does not disclose proprietary trade secret information or violate copyright law or patented processes, so that a reasonable person with sufficient training, experience and competence in claims processing can determine the payment to be made according to the terms of the contract.
A plan or a plan's capitated provider may disclose the Fee Schedules and Other Required Information mandated by this section through the use of a website so long as the plan or the plan's capitated provider provides written notice to the contracted provider at least 45 days prior to implementing a website transmission format or posting any changes to the information on the website.
(p) Waiver Prohibited. The plan and the plan's capitated provider shall not require or allow a provider to waive any right conferred upon the provider or any obligation imposed upon the plan by sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28, relating to claims processing or payment. Any contractual provision or other agreement purporting to constitute, create or result in such a waiver is null and void.
(q) Required Reports.
(1) Within 60 days of the close of each calendar quarter, the plan shall disclose to the Department in a single combined document: (A) any emerging patterns of claims payment deficiencies; (B) whether any of its claims processing organizations or capitated providers failed to timely and accurately reimburse 95% of its claims (including the payment of interest and penalties) consistent with sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28; and (C) the corrective action that has been undertaken over the preceding two quarters. The first report from the plan shall be due within 45 days after the close of the calendar quarter that ends 120 days after the effective date of these regulations.
(2) Within 15 days of the close of each calendar year, beginning with the 2004 calendar year, the plan shall submit to the Director, as part of the Annual Plan Claims Payment and Dispute Resolution Mechanism Report as specified in section 1367(h) of the Health and Safety Code and section 1300.71.38(k) of title 28, in an electronic format (to be supplied by the Department), information disclosing the claims payment compliance status of the plan and each of its claims processing organizations and capitated providers with each of sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28. The Annual Plan Claims Payment and Dispute Resolution Mechanism Report for 2004 shall include claims payment and dispute resolution data received from October 1, 2003 through September 30, 2004. Each subsequent Annual Plan Claims Payment and Dispute Resolution Mechanism Report shall include claims payment and dispute resolution data received for the last calendar quarter of the year preceding the reporting year and the first three calendar quarters for the reporting year.
(A) The claims payment compliance status portion of the Annual Plan Claims Payment and Dispute Resolution Mechanism Report shall: (i) be based upon the plan's claims processing organization's and the plan's capitated provider's Quarterly Claims Payment Performance Reports submitted to the plan and upon the audits and other compliance processes of the plan consistent with section 1300.71.38(m) and (ii) include a detailed, informative statement: (1) disclosing any established or documented patterns of claims payment deficiencies, (2) outlining the corrective action that has been undertaken, and (3) explaining how that information has been used to improve the plan's administrative capacity, plan-provider relations, claim payment procedures, quality assurance system (process) and quality of patient care (results). The information provided pursuant to this section shall be submitted with the Annual Plan Claims Payment and Dispute Resolution Mechanism Report and may be accompanied by a cover letter requesting confidential treatment pursuant to section 1007 of title 28.
(r) Confidentiality.
The claims payment compliance status portion of the plan's Annual Plan Claims Payment and Dispute Resolution Mechanism Report and the Quarterly disclosures pursuant to section (q)(1) to the Department shall be public information except for information disclosed pursuant to section (q)(2)(A)(ii), that the Director, pursuant to a plan's written request, determines should be maintained on a confidential basis.
(s) Review and Enforcement.
(1) The Department may review the plan's and the plan's capitated provider's claims processing system through periodic medical surveys and financial examinations under sections 1380, 1381 or 1382 of the Health and Safety Code, and when appropriate, through the investigation of complaints of demonstrate and unjust payment patterns.
(2) Failure of a plan to comply with the requirements of sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28 may constitute a basis for disciplinary action against the plan. The civil, criminal, and administrative remedies available to the Director under the Health and Safety Code and this regulation are not exclusive, and may be sought and employed in any combination deemed advisable by the Director to enforce the provisions of this regulation.
(3) Violations of the Health and Safety Code and this regulation are subject to enforcement action whether or not remediated, although a plan's identification and self-initiated remediation of deficiencies may be considered in determining the appropriate penalty.
(4) In making a determination that a plan's or a plan's capitated provider's practice, policy or procedure constitutes a “demonstrable and unjust payment pattern” or “unfair payment pattern,” the Director shall consider the documentation or justification for the implementation of the practice, policy or procedure and may consider the aggregate amount of money involved in the plan's or the plan's capitated provider's action or inaction; the number of claims adjudicated by the plan or plan's capitated provider during the time period in question, legitimate industry practices, whether there is evidence that the provider had engaged in an unfair billing practice, the potential impact of the payment practices on the delivery of health care or on provider practices; the plan's or the plan's capitated provider's intentions or knowledge of the violation(s); the speed and effectiveness of appropriate remedial measures implemented to ameliorate harm to providers or patients, or to preclude future violations; and any previous related or similar enforcement actions involving the plan or the plan's capitated provider.
(5) Within 30 days of receipt of notice that the Department is investigating whether the plan's or the plan's capitated provider's practice, policy or procedure constitutes a demonstrable and unjust payment pattern, the plan may submit a written response documenting that the practice, policy or procedure was a necessary and reasonable claims settlement practice and consistent with sections 1371, 1371.35 and 1371.37 of the Health and Safety Code and these regulations;
(6) In addition to the penalties that may be assessed pursuant to section (s)(2), a plan determined to be engaged in a Demonstrable and Unjust Payment Pattern may be subject to any combination of the following additional penalties:
(A) The imposition of an additional monetary penalty to reflect the serious nature of the demonstrable and unjust payment pattern;
(B) The imposition, for a period of up to three (3) years, of a requirement that the plan reimburse complete and accurate claims in a shorter time period than the time period prescribed in section (g) of this regulation and sections 1371 and 1371.35 of the Health and Safety Code; and
(C) The appointment of a claims monitor or conservator to supervise the plan's claim payment activities to insure timely compliance with claims payment obligations.
The plan shall be responsible for the payment of all costs incurred by the Department in any administrative and judicial actions, including the cost to monitor the plan's and the plan's capitated provider's compliance.
(t) Compliance. Plans and the plans' capitated providers shall be fully compliant with these regulations on or before January 1, 2004.
NOTE
Authority cited: Sections 1344, 1371.38, 1371.1 and 1371.8, Health and Safety Code. Reference: Sections 1367, 1370 and 1371.38, Health and Safety Code.
HISTORY
1. New section filed 7-24-2003; operative 8-23-2003 (Register 2003, No. 30). For prior history of title 10, section 1300.71, see Register 80, No. 19.
§1300.71.38. Fast, Fair and Cost-Effective Dispute Resolution Mechanism.
Note • History
All health care service plans and their capitated providers that pay claims (plan's capitated provider) shall establish a fast, fair and cost-effective dispute resolution mechanism to process and resolve contracted and non-contracted provider disputes. The plan and the plan's capitated provider may maintain separate dispute resolution mechanisms for contracted and non-contracted provider disputes and separate dispute resolution mechanisms for claims and other types of billing and contract disputes, provided that each mechanism complies with sections 1367(h), 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.36, 1371.37, 1371.4, and 1371.8 of the Health and Safety Code and sections 1300.71, 1300.71.38, 1300.71.4, and 1300.77.4 of title 28. Arbitration shall not be deemed a provider dispute or a provider dispute resolution mechanism for the purposes of this section.
(a) Definitions:
(1) “Contracted Provider Dispute” means a contracted provider's written notice to the plan or the plan's capitated provider challenging, appealing or requesting reconsideration of a claim (or a bundled group of substantially similar multiple claims that are individually numbered) that has been denied, adjusted or contested or seeking resolution of a billing determination or other contract dispute (or a bundled group of substantially similar multiple billing or other contractual disputes that are individually numbered) or disputing a request for reimbursement of an overpayment of a claim that contains, at a minimum, the following information: the provider's name; the provider's identification number; contact information; and:
(A) If the dispute concerns a claim or a request for reimbursement of an overpayment of a claim, a clear identification of the disputed item, the date of service and a clear explanation of the basis upon which the provider believes the payment amount, request for additional information, request for reimbursement for the overpayment of a claim, contest, denial, adjustment or other action is incorrect;
(B) If the dispute is not about a claim, a clear explanation of the issue and the provider's position thereon; and
(C) If the dispute involves an enrollee or group of enrollees: the name and identification number(s) of the enrollee or enrollees, a clear explanation of the disputed item, including the date of service and the provider's position thereon.
(2) “Non-Contracted Provider Dispute” means a non-contracted provider's written notice to the plan or the plan's capitated provider challenging, appealing or requesting reconsideration of a claim (or a bundled group of substantially similar claims that are individually numbered) that has been denied, adjusted or contested or disputing a request for reimbursement of an overpayment of a claim that contains, at a minimum, the following information: the provider's name, the provider's identification number, contact information and:
(A) If the dispute concerns a claim or a request for reimbursement of an overpayment of a claim, a clear identification of the disputed item, including the date of service, and a clear explanation of the basis upon which the provider believes the payment amount, request for additional information, contest, denial, request for reimbursement of an overpayment of a claim or other action is incorrect.
(B) If the dispute involves an enrollee or group of enrollees, the name and identification number(s) of the enrollee or enrollees, a clear explanation of the disputed item, including the date of service and the provider's position thereon.
(3) “Date of receipt” means the working day when the provider dispute or amended provider dispute, by physical or electronic means, is first delivered to the plan's or the plan's capitated provider's designated dispute resolution office or post office box. This definition shall not affect the presumption of receipt of mail set forth in Evidence Code section 641.
(4) “Date of Determination” means the date of postmark or electronic mark on the written provider dispute determination or amended provider dispute determination that is delivered, by physical or electronic means, to the claimant's office or other address of record. To the extent that a postmark or electronic mark is unavailable to confirm the Date of Determination, the Department may consider, when auditing the plan's or the plan's capitated provider's provider dispute mechanism, the date the check is printed for any monies determined to be due and owing the provider and date the check is presented for payment. This definition shall not affect the presumption of receipt of mail set forth in Evidence Code section 641.
(5) “Plan” for the purposes of this section means a licensed health care service plan and its contracted claims processing organization(s).
(b) Notice to Provider of Dispute Resolution Mechanism(s). Whenever the plan or the plan's capitated provider contests, adjusts or denies a claim, it shall inform the provider of the availability of the provider dispute resolution mechanism and the procedures for obtaining forms and instructions, including the mailing address, for filing a provider dispute.
(c) Submission of Provider Disputes. The plan and the plan's capitated provider shall establish written procedures for the submission, receipt, processing and resolution of contracted and non-contracted provider disputes that, at a minimum, provide that:
(1) Provider disputes be submitted utilizing the same number assigned to the original claim; thereafter the plan or the plan's capitated provider shall process and track the provider dispute in a manner that allows the plan, the plan's capitated provider, the provider and the Department to link the provider dispute with the number assigned to the original claim.
(2) Contracted Provider Disputes be submitted in a manner consistent with procedures disclosed in sections 1300.71(l)(1) -(4).
(3) Non-contracted Provider Disputes be submitted in a manner consistent with the directions for obtaining forms and instructions for filing a provider dispute attached to the plan's or the plan's capitated provider's notice that the subject claim has been denied, adjusted or contested or pursuant to the directions for filing Non-contracted Provider Disputes contained on the plan's or the plan's capitated provider's website.
(4) The plan shall resolve any provider dispute submitted on behalf of an enrollee or a group of enrollees treated by the provider in the plan's consumer grievance process and not in the plan's or the plan's capitated provider's dispute resolution mechanism. The plan may verify the enrollee's authorization to proceed with the grievance prior to submitting the complaint to the plan's consumer grievance process. When a provider submits a dispute on behalf of an enrollee or a group of enrollees, the provider shall be deemed to be joining with or assisting the enrollee within the meaning of section 1368 of the Health and Safety Code.
(d) Time Period for Submission.
(1) Neither the plan nor the plan's capitated provider that pays claims, except as required by any state or federal law or regulation, shall impose a deadline for the receipt of a provider dispute for an individual claim, billing dispute or other contractual dispute that is less than 365 days of plan's or the plan's capitated provider's action or, in the case of inaction, that is less than 365 days after the Time for Contesting or Denying Claims has expired. If the dispute relates to a demonstrable and unfair payment pattern by the plan or the plan's capitated provider, neither the plan nor the plan's capitated provider shall impose a deadline for the receipt of a dispute that is less than 365 days from the plan's or the plan's capitated provider's most recent action or in the case of inaction that is less than 365 days after the most recent Time for Contesting or Denying Claims has expired.
(2) The plan or the plan's capitated provider may return any provider dispute lacking the information enumerated in either section (a)(1) or (a)(2), if the information is in the possession of the provider and is not readily accessible to the plan or the plan's capitated provider. Along with any returned provider dispute, the plan or the plan's capitated provider shall clearly identify in writing the missing information necessary to resolve the dispute consistent with sections 1300.71(a)(10) and (11) and 1300.71(d)(1), (2) and (3). Except in situation where the claim documentation has been returned to the provider, no plan or a plan's capitated provider shall request the provider to resubmit claim information or supporting documentation that the provider previously submitted to the plan or the plan's capitated provider as part of the claims adjudication process.
(3) A provider may submit an amended provider dispute within thirty (30) working days of the date of receipt of a returned provider dispute setting forth the missing information.
(e) Time Period for Acknowledgment. A plan or a plan's capitated provider shall enter into its dispute resolution mechanism system(s) each provider dispute submission (whether or not complete), and shall identify and acknowledge the receipt of each provider dispute:
(1) In the case of an electronic provider dispute, the acknowledgement shall be provided within two (2) working days of the date of receipt of the electronic provider dispute by the office designated to receive provider disputes, or
(2) In the case of a paper provider dispute, the acknowledgement shall be provided within fifteen (15) working days of the date of receipt of the paper provider dispute by the office designated to receive provider disputes.
(f) Time Period for Resolution and Written Determination. The plan or the plan's capitated provider shall resolve each provider dispute or amended provider dispute, consistent with applicable state and federal law and the provisions of sections 1371, 1371.1, 1371.2, 1371.22, 1371.35, 1371.37, 1371.4 and 1371.8 of the Health and Safety Code and section 1300.71, 1300.71.38, 1300.71.4 and 1300.77.4 of title 28, and issue a written determination stating the pertinent facts and explaining the reasons for its determination within 45 working days after the date of receipt of the provider dispute or the amended provider dispute.
Copies of provider disputes and determinations, including all notes, documents and other information upon which the plan or the plan's capitated provider relied to reach its decision, and all reports and related information shall be retained for at least the period specified in section 1300.85.1 of title 28.
(g) Past Due Payments. If the provider dispute or amended provider dispute involves a claim and is determined in whole or in part in favor of the provider, the plan or the plan's capitated provider shall pay any outstanding monies determined to be due, and all interest and penalties required under sections 1371 and 1371.35 of the Health and Safety Code and section 1300.71 of title 28, within five (5) working days of the issuance of the Written Determination. Accrual of interest and penalties for the payment of these resolved provider disputes shall commence on the day following the expiration of “Time for Reimbursement” as forth in section 1300.71(g).
(h) Designation of Plan Officer. The plan and the plan's capitated provider shall each designate a principal officer, as defined by section 1300.45(o) of title 28, to be primarily responsible for the maintenance of their respective provider dispute resolution mechanism(s), for the review of its operations and for noting any emerging patterns of provider disputes to improve administrative capacity, plan-provider relations, claim payment procedures and patient care. The designated principal officer shall be responsible for preparing, the reports and disclosures as specified in sections 1300.71(e)(3) and (q) and 1300.71.38(k) of title 28.
(i) No Discrimination. The plan or the plan's capitated provider shall not discriminate or retaliate against a provider (including but not limited to the cancellation of the provider's contract) because the provider filed a contracted provider dispute or a non-contracted provider dispute.
(j) Dispute Resolution Costs. A provider dispute received under this section shall be received, handled and resolved by the plan and the plan's capitated provider without charge to the provider. Notwithstanding the foregoing, the plan and the plan's capitated provider shall have no obligation to reimburse a provider for any costs incurred in connection with utilizing the provider dispute resolution mechanism.
(k) Required Reports. Beginning with the 2004 calendar year and for each subsequent year, the plan shall submit to the Department no more than fifteen (15) days after the close of the calendar year, an “Annual Plan Claims Payment and Dispute Resolution Mechanism Report,” described in part in Section 1300.71(q) of this regulation, on an electronic form to be supplied by the Department Managed Health Care pursuant to section 1300.41.8 of title 28 containing the following, which shall be reported based upon the date of receipt of the provider dispute or amended provider dispute:
(1) Information on the number and types of providers using the dispute resolution mechanism;
(2) A summary of the disposition of all provider disputes, which shall include an informative description of the types, terms and resolution. Disputes contained in a bundled submission shall be reported separately as individual disputes. Information may be submitted in an aggregate format so long as all data entries are appropriately footnoted to provide full and fair disclosure; and
(3) A detailed, informative statement disclosing any emerging or established patterns of provider disputes and how that information has been used to improve the plan's administrative capacity, plan-provider relations, claim payment procedures, quality assurance system (process) and quality of patient care (results) and how the information has been used in the development of appropriate corrective action plans. The information provided pursuant to this paragraph shall be submitted with, but separately from the other portions of the Annual Plan Claims Payment and Dispute Resolution Mechanism Report and may be accompanied by a cover letter requesting confidential treatment pursuant section 1007 of title 28.
(4) The first report shall be due on or before January 15, 2005.
(l) Confidentiality.
(1) The plan's Annual Plan Claims Payment and Dispute Resolution Mechanism Report to the Department regarding its dispute resolution mechanism shall be public information except for information disclosed pursuant to section (k)(3) above, that the Director, pursuant to a plan's written request, determines should be maintained on a confidential basis.
(2) The plan's quarterly disclosures pursuant to section 1300.71(q)(1) shall be public information except for the information relating to the plan's corrective action strategies that the Director, pursuant to a plan's written request, determines should be maintained on a confidential basis.
(m) Review and Enforcement.
(1) The Department shall review the plan's and the plan's capitated provider's provider dispute resolution mechanism(s), including the records of provider disputes filed with the plan and remedial action taken pursuant to section 1300.71.38(m)(3), through medical surveys and financial examinations under sections 1380, 1381 or 1382 of the Health and Safety Code, and when appropriate, through the investigation of complaints of unfair provider dispute resolution mechanism(s).
(2) The failure of a plan to comply with the requirements of this regulation shall be a basis for disciplinary action against the plan. The civil, criminal, and administrative remedies available to the Director under the Health and Safety Code and this regulation are not exclusive, and may be sought and employed in any combination deemed advisable by the Director to enforce the provisions of this regulation.
(3) Violations of the Act and this regulation are subject to enforcement action whether or not remediated, although a plan's self-identification and self-initiated remediation of violations or deficiencies may be considered in determining the appropriate penalty.
NOTE
Authority cited: Sections 1344 and 1371.38, Health and Safety Code. Reference: Sections 1367, 1371 and 1371.38, Health and Safety Code.
HISTORY
1. New section filed 7-24-2003; operative 8-23-2003 (Register 2003, No. 30).
§1300.71.39. Unfair Billing Patterns.
Note • History
(a) Except for services subject to the requirements of Section 1367.11 of the Act, “unfair billing pattern” includes the practice, by a provider of emergency services, including but not limited to hospitals and hospital-based physicians such as radiologists, pathologists, anesthesiologists, and on-call specialists, of billing an enrollee of a health care service plan for amounts owed to the provider by the health care service plan or its capitated provider for the provision of emergency services.
(b) For purposes of this section:
(1) “Emergency services” means those services required to be covered by a health plan pursuant to Health & Safety Code sections 1345(b)(6), 1367(i), 1371.4, 1371.5 and Title 28, California Code of Regulations, sections 1300.67(g) and 1300.71.4.
(2) Co-payments, coinsurance and deductibles that are the financial responsibility of the enrollee are not amounts owed the provider by the health care service plan.
(3) “The plan's capitated provider” shall have the same meaning as that provided in section 1300.71(a).
NOTE
Authority cited: Sections 1344, 1371.39 and 1371.4, Health and Safety Code. Reference: Sections 1317.1, 1317.7, 1342, 1345, 1346, 1362.8, 1367, 1371, 1371.1, 1371.35, 1371.36, 1371.38, 1371.39, 1371.4, 1371.5 and 1379, Health and Safety Code.
HISTORY
1. New section filed 9-15-2008; operative 10-15-2008 (Register 2008, No. 38).
§1300.71.4. Emergency Medical Condition and Post-Stabilization Responsibilities for Medically Necessary Health Care Services.
Note • History
The following rules set forth emergency medical condition and post-stabilization responsibilities for medically necessary health care services after stabilization of an emergency medical condition and until an enrollee can be discharged or transferred. These rules do not apply to a specialized health care service plan contract that does not provide for medically necessary health care services following stabilization of an emergency condition.
(a) Prior to stabilization of an enrollee's emergency medical condition, or during periods of destabilization (after stabilization of an enrollee's emergency medical condition) when an enrollee requires immediate medically necessary health care services, a health care service plan shall pay for all medically necessary health care services rendered to an enrollee.
(b) In the case when an enrollee is stabilized but the health care provider believes that the enrollee requires additional medically necessary health care services and may not be discharged safely, the following applies:
(1) A health care service plan shall approve or disapprove a health care provider's request for authorization to provide necessary post-stabilization medical care within one half hour of the request.
(2) If a health care service plan fails to approve or disapprove a health care provider's request for authorization to provide necessary post-stabilization medical care within one half-hour of the request, the necessary post-stabilization medical care shall be deemed authorized. Notwithstanding the foregoing sentence, the health care service plan shall have the authority to disapprove payment for (A) the delivery of such necessary post-stabilization medical care or (B) the continuation of the delivery of such care; provided, that the health care service plan notifies the provider prior to the commencement of the delivery of such care or during the continuation of the delivery of such care (in which case, the plan shall not be obligated to pay for the continuation of such care from and after the time it provides such notice to the provider, subject to the remaining provisions of this paragraph) and in both cases the disruption of such care (taking into account the time necessary to effect the enrollee's transfer or discharge) does not have an adverse impact upon the efficacy of such care or the enrollee's medical condition.
(3) Notwithstanding the provisions of subsection (b) of this rule, a health care service plan shall pay for all medically necessary health care services provided to an enrollee which are necessary to maintain the enrollee's stabilized condition up to the time that the health care service plan effectuates the enrollee's transfer or the enrollee is discharged.
(c) In the case where a plan denies the request for authorization of post-stabilization medical care and elects to transfer an enrollee to another health care provider, the following applies:
(1) When a health care service plan responds to a health care provider's request for post-stabilization medical care authorization by informing the provider of the plan's decision to transfer the enrollee to another health care provider, the plan shall effectuate the transfer of the enrollee as soon as possible,
(2) A health care service plan shall pay for all medically necessary health care services provided to an enrollee to maintain the enrollee's stabilized condition up to the time that the health care service plan effectuates the enrollee's transfer.
(d) All requests for authorizations, and all responses to such requests for authorizations, of post-stabilization medically necessary health care services shall be fully documented. All provision of medically necessary health care services shall be fully documented. Documentation shall include, but not be limited to, the date and time of the request, the name of the health care provider making the request, and the name of the plan representative responding to the request.
NOTE
Authority cited: Sections 1344 and 1371.4(g) and (h), Health and Safety Code. Reference: Sections 1317.1 and 1371.4, Health and Safety Code.
HISTORY
1. New section filed 5-9-95 as an emergency; operative 5-9-95 (Register 95, No. 19). A Certificate of Compliance must be transmitted to OAL by 9-6-95 or emergency language will be repealed by operation of law on the following day.
2. New section refiled 9-5-95 as an emergency; operative 9-6-95 (Register 95, No. 36). A Certificate of Compliance must be transmitted to OAL by 1-4-96 or emergency language will be repealed by operation of law on the following day.
3. New section refiled 12-19-95 as an emergency; operative 1-4-96 (Register 95, No. 51). A Certificate of Compliance must be transmitted to OAL by 4-17-96 or emergency language will be repealed by operation of law on the following day.
4. Certificate of Compliance, including amendment of section and Note, transmitted to OAL 3-7-96 and filed 4-11-96 (Register 96, No. 15).
5. Editorial correction of first paragraph and subsections (b)(2), (c) and (c)(1) (Register 96, No. 23).
6. Editorial correction of first paragraph (Register 99, No. 26).
7. Amendment filed 6-24-99 as an emergency; operative 6-24-99 (Register 99, No. 26). A Certificate of Compliance must be transmitted to OAL by 10-22-99 or emergency language will be repealed by operation of law on the following day.
8. Certificate of Compliance as to 6-24-99 order transmitted to OAL 9-30-99 and filed 11-8-99 (Register 99, No. 46).
§1300.73.21. Arbitration and Settlement Agreements.
Note • History
(a) All health care service plans (plans) shall ensure that all arbitration decisions involving the plan and a current or former enrollee shall be provided to the Department as follows:
(1) Within thirty (30) days of receiving a written arbitration decision, the plan shall provide a copy of the complete arbitration decision to the Department. The complete arbitration decision shall have no part of the decision altered or redacted. The complete arbitration decision shall indicate the prevailing party, the amount and other relevant terms of any award, and the reasons for the decision.
(2) On a quarterly basis, plans shall provide the Department with redacted copies of all written arbitration decisions. The plan shall be responsible for redacting the written arbitration decisions ensuring that the names of the enrollee, the plan, witnesses, attorneys, providers, plan employees and health facilities have been removed from the decision. The redacted arbitration decisions will be available for public inspection on the Department's web page (www.dmhc.ca.gov).
(b) Every written arbitration decision, and every written settlement agreement resolving any dispute between a plan and a current or former enrollee shall contain the following language in bold, twelve (12) point type:
Nothing in this arbitration decision (or settlement agreement) prohibits or restricts the enrollee from discussing or reporting the underlying facts, results, terms and conditions of this decision (or settlement agreement) to the Department of Managed Health Care.
(c) All health care service contracts containing an arbitration clause; all arbitration agreements and decisions; and all settlement agreements resolving any dispute between a plan and a current or former enrollee, shall contain no language that expressly or impliedly prohibits the enrollee from discussing or reporting the underlying facts, outcome, results or decision with the Department.
(d) For purposes of this section, a “settlement agreement” shall be broadly construed to include any writing resolving a dispute between a plan and a current or former enrollee wherein the nature of the dispute relates to services, benefits, treatment or other rights and obligations created pursuant to the enrollee and plan's contract for health care coverage, and includes settlements reached in, but not limited to, a mediation, arbitration, or other alternative dispute resolution process, or any civil lawsuit.
NOTE
Authority Cited: Sections 1344, 1346 and 1373.21, Health and Safety Code. Reference: Sections 1373.19 and 1373.20, Health and Safety Code.
HISTORY
1. New section filed 8-19-2002; operative 9-18-2002 (Register 2002, No. 34).
§1300.74.16. Standing Referral to HIV/AIDS Specialist.
Note • History
(a) The definitions and requirements of this section are applicable only to standing referrals made pursuant to Section 1374.16 of the Act. Nothing in this section requires an enrollee to transfer to a different primary care provider or limits referral authorizations that are not subject to Section 1374.16 of the Act.
(b) For the purposes of this section “AIDS” means Acquired Immunodeficiency Syndrome.
(c) For the purposes of this section “category 1 continuing medical education” means:
(1) For physicians, continuing medical education courses recognized as qualifying for category 1 credit by the Medical Board of California;
(2) For nurse practitioners, continuing education contact hours recognized by the California Board of Registered Nursing;
(3) For physician assistants, continuing education units approved by the American Association of Physician Assistants or those described in either subsection (c)(1) or (c)(2), above.
(d) For the purposes of this section “HIV” means the Human Immunodeficiency Virus.
(e) For the purposes of this section an “HIV/AIDS specialist” means a physician who holds a valid, unrevoked and unsuspended certificate to practice medicine in the state of California who meets any one of the following four criteria:
(1) Is credentialed as an “HIV Specialist” by the American Academy of HIV Medicine; or
(2) Is board certified, or has earned a Certificate of Added Qualification, in the field of HIV medicine granted by a member board of the American Board of Medical Specialties, should a member board of that organization establish board certification, or a Certificate of Added Qualification, in the field of HIV medicine; or
(3) Is board certified in the field of infectious diseases by a member board of the American Board of Medical Specialties and meets the following qualifications:
(A) In the immediately preceding 12 months has clinically managed medical care to a minimum of 25 patients who are infected with HIV; and
(B) In the immediately preceding 12 months has successfully completed a minimum of 15 hours of category 1 continuing medical education in the prevention of HIV infection, combined with diagnosis, treatment, or both, of HIV-infected patients, including a minimum of 5 hours related to antiretroviral therapy per year; or
(4) Meets the following qualifications:
(A) In the immediately preceding 24 months has clinically managed medical care to a minimum of 20 patients who are infected with HIV; and
(B) Has completed any of the following:
1. In the immediately preceding 12 months has obtained board certification or recertification in the field of infectious diseases from a member board of the American Board of Medical Specialties; or
2. In the immediately preceding 12 months has successfully completed a minimum of 30 hours of category 1 continuing medical education in the prevention of HIV infection, combined with diagnosis, treatment, or both, of HIV-infected patients; or
3. In the immediately preceding 12 months has successfully completed a minimum of 15 hours of category 1 continuing medical education in the prevention of HIV infection, combined with diagnosis, treatment, or both, of HIV-infected patients and has successfully completed the HIV Medicine Competency Maintenance Examination administered by the American Academy of HIV medicine.
(f) When authorizing a standing referral to a specialist pursuant to Section 1374.16(a) of the Act for the purpose of the diagnosis or treatment of a condition requiring care by a physician with a specialized knowledge of HIV medicine, a health care service plan must refer the enrollee to an HIV/AIDS specialist. When authorizing a standing referral to a specialist for purposes of having that specialist coordinate the enrollee's health care pursuant to Section 1374.16(b) of the Act for an enrollee who is infected with HIV, a health care service plan must refer the enrollee to an HIV/AIDS specialist. The HIV/AIDS specialist may utilize the services of a nurse practitioner or physician assistant if:
(1) The nurse practitioner or physician assistant is under the supervision of an HIV/AIDS specialist; and
(2) The nurse practitioner or physician assistant meets the qualifications specified in subsection (e)(4); and
(3) The nurse practitioner or physician assistant and that provider's supervising HIV/AIDS specialist have the capacity to see an additional patient.
(g) Subsection (f) does not require a health care service plan to refer an enrollee to any provider who is not employed by or under contract with the health care service plan to provide health care services to its enrollees, unless there is no HIV/AIDS specialist, or appropriately qualified nurse practitioner or physician assistant under the supervision of an HIV/AIDS specialist, within the plan's network appropriate to provide care to the enrollee, as determined by the primary care physician in consultation with the plan medical director.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1344 and 1374.16, Health and Safety Code.
HISTORY
1. Renumbering of former section 1300.67.60 to new section 1300.74.16, including repealer of subsections (h)-(i), filed 1-10-2008; operative 2-9-2008 (Register 2008, No. 2).
§1300.74.30. Independent Medical Review System.
Note • History
(a) Plan enrollees may request independent medical review pursuant to this regulation for decisions that are eligible for independent medical review under Article 5.55 and section 1370.4 of the Act. The independent medical review process shall resolve decisions that deny, modify, or delay health care services, that deny reimbursement for urgent or emergency services or that involve experimental or investigational therapies. Specialized plans shall provide for independent medical reviews under this section if a covered service relates to the practice of medicine or is provided pursuant to a contract with a health plan providing medical, surgical and hospital services. The Department shall be the final arbiter when there is a question as to whether a dispute over a health care service is eligible for independent medical review, and whether extraordinary and compelling circumstances exist that waive the requirement that the enrollee first participate in the plan's grievance system.
(b) An enrollee may apply for an independent medical review under the conditions specified in Section 1374.30(j) of the Act. The Department may waive the requirement that the enrollee participate in the plan's grievance process if the Department determines that extraordinary and compelling circumstances exist, which include, but are not limited to, serious pain, the potential loss of life, limb or major bodily function, or the immediate, and serious deterioration of the health of the enrollee.
(c) In cases involving a claim for out of plan emergency or urgent services that a provider determined were medically necessary, the independent medical review shall determine whether the services were emergency or urgent services necessary to screen and stabilize the enrollee's condition. For purposes of this section “emergency services” are services for emergency medical conditions as defined in section 1300.71.4 of title 28, and “urgent services” are all services, except emergency services, where the enrollee has obtained the services without prior authorization from the plan, or from a contracting provider.
(d) Applications for independent medical review shall be submitted on a one-page form entitled Independent Medical Review Application (DMHC IMR 11/00), which is incorporated by reference, and shall be provided by the Department. The form shall contain a signed release from the enrollee, or a person authorized pursuant to law to act on behalf of the enrollee, authorizing release of medical and treatment information. Additionally, the enrollee may provide any relevant material or documentation with the application including, but not limited to:
(1) A copy of the adverse determination by the plan or contracting provider notifying the enrollee that the request for health care services was denied, delayed or modified, in whole or in part, based on the determination that the service was not medically necessary;
(2) Medical records, statements from the enrollee's provider or other documents establishing that the dispute is eligible for review;
(3) A copy of the grievance requesting the health care service or benefit filed with the plan or any entity with delegated authority to resolve grievances, and the response to the grievance, if any;
(4) If expedited review is requested for a decision eligible for independent medical review pursuant to Article 5.55 of the Act, the application shall include, a certification from the enrollee's physician or provider indicating that an imminent and serious threat to the health of the enrollee exists. If expedited review is requested for a decision eligible for independent medical review pursuant to section 1370.4 of the Act, the application shall include a certification from the enrollee's physician that the proposed therapy would be significantly less effective if not promptly initiated.
(e) If additional information is needed to complete an application or to determine the enrollee's eligibility for independent medical review, the Department shall advise the enrollee or the enrollee's representative, the enrollee's provider, the enrollee's health care plan or the enrollee's attending physician, as appropriate, by the most efficient means available.
(f) The Department shall evaluate complaints received under subsection (b) of Section 1368 of the Act and applications submitted under this regulation and determine whether the enrollee is eligible for an independent medical review. The Department's determination will consider all information provided to the Department, the enrollee's medical condition and the disputed health care service. If the Department determines that the case should not be referred to independent medical review, the request shall be considered a complaint under subsection (b) of Section 1368 and sections 1300.68 and 1300.68.01. The enrollee or the enrollee's representative, health plan and any involved provider shall be advised of the Department's determination.
(1) The request for independent medical review shall be filed with the Department within six months of the plan's written response to the enrollee's grievance. The six-month period does not begin to run until the enrollee, or the enrollee's representative, has been properly notified in writing of the plan's resolution of the grievance. Applications will not be rejected as untimely solely because the enrollee, the enrollee's provider, or the plan failed to submit supporting documentation. Requests for extensions or late applications shall be approved if a timely submission was reasonably impaired by inadequate notice of the independent medical review process or by the applicant's medical circumstances.
(2) An application will not be eligible for independent medical review if the enrollee's complaint has previously been submitted and reviewed by the Department. Exceptions may be approved if the application for independent medical review includes medical records and a statement from the enrollee's physician or provider demonstrating significant changes in the enrollee's medical condition or in medical therapies available have occurred since the Department's disposition of the complaint.
(3) Enrollees of Medi-Cal health care service plans are eligible for an independent medical review if the enrollee has not presented the disputed health care service for resolution by the Medi-Cal fair hearing process. Reviews shall be conducted in accordance with the statutes and regulations of the Medi-Cal program.
(4) This regulation applies to Medicare enrollees, to the extent the regulation does not conflict with federal law, including 42 USCS §1395w-26 (2004).
(g) Except for Medi-Cal enrollees, and Medicare enrollees exempted by federal law, as described at subsection (f)(4), the independent medical review system established pursuant to this section shall be the exclusive independent medical review process offered to enrollees for disputes involving the medical necessity of covered health care services. Nothing in this section shall preclude a health plan from offering other independent review processes for disputes that do not involve medical necessity.
(h) When the Department finds that a plan fails to advise an enrollee of the availability of independent medical review as required under Health and Safety Code section 1374.30(i), or engages in a practice of mischaracterizing determinations substantially based on medical necessity as coverage decisions, or otherwise interferes with the rights of enrollees to obtain independent medical review, the Department shall impose administrative penalties on the plan in accordance with the Act.
(i) The director shall notify the enrollee and the enrollee's health care plan if an application for independent medical review has been accepted within seven (7) calendar days of receipt of a completed application for a routine request and within 48 hours of receipt of a completed application for an expedited review. The notification shall identify the independent medical review organization, whether the review shall be conducted on an expedited or routine basis and other information deemed necessary by the Department. The director shall also transmit to the enrollee's health care plan a copy of the enrollee's signed release of medical and treatment information and copies of all other materials submitted with the enrollee's application.
(j) Following receipt of the Department's notification that an application for independent medical review has been assigned to an independent medical review organization, the plan shall provide the organization with all information that was considered in relation to the disputed health care service, the enrollee's grievance and the plan's determination. The plan shall forward all information to the medical review organization within three (3) business days for a regular review and within one (1) calendar day in the case of an expedited review.
(1) Unless otherwise advised in the notification or by the assigned review organization, the plan shall submit a complete set of the materials described below for the independent review organization.
(A) A copy of all correspondence from and received by the plan concerning the disputed health care service, including but not limited to, any enrollee grievance relating to the requested service;
(B) A complete and legible copy of all medical records and other information used by the plan in making its decision regarding the disputed health care service. An additional copy of medical records shall be submitted for each reviewer.
(C) A copy of the cover page of the evidence of coverage and complete pages with the referenced sections highlighted or underlined sections, if the evidence of coverage was referenced in the plan's resolution of the enrollee's grievance;
(D) The plan's response to any additional issues raised in the enrollee's application for independent medical review.
(2) The plan shall promptly provide the enrollee with an annotated list of all documents submitted to the independent medical review organization, together with information on how copies may be requested.
(k) Plans shall be responsible for providing additional information as follows:
(1) Any medical records or other relevant matters not available at the time of the Department's initial notification, or that result from the enrollee's on-going medical care or treatment for the medical condition or disease under review. Such matters shall be forwarded as soon as possible upon receipt by the health plan, not to exceed five (5) business days in routine cases or one (1) calendar day in expedited cases.
(2) Additional medical records or other information requested by the IMR organization shall be sent within five (5) business days in routine cases or one (1) calendar day in expedited cases. In expedited reviews, the health care plan shall immediately notify the enrollee and the enrollee's health care provider by telephone or facsimile to identify and request the necessary information, followed by written notification, when the request involves materials not in the possession of the plan or its contracting providers.
(l) Each assigned reviewer shall issue a separate written analysis of the case, explaining the determination made, using plain English where possible. The analysis shall describe how the determination relates to the enrollee's medical condition and history, relevant medical records and other documents considered, and references to the specific medical and scientific evidence listed in Sections 1370.4(d) or 1374.33(b) of the Act, as applicable. For requests made pursuant to Article 5.55 of the Act, reviewers shall determine whether the disputed service is medically necessary for the enrollee. For requests made pursuant to section 1370.4 of the Act, the reviewers shall determine whether the requested therapy is likely to be more beneficial for the enrollee then other available standard therapies, and whether the plan shall provide the requested therapy. Reviews based on section 1300.70.4 of these regulations shall also reference the medical and scientific evidence considered in assessing whether the requested health care service is likely to be more beneficial than other available standard therapies. The analysis may also discuss the risks and benefits considered by the reviewer in considering proposed and standard treatments.
(m) The Department, the enrollee, or his/her representative may withdraw a case from the independent review system at any time. The plan may seek withdrawal of the case from the review system by providing the disputed health care service, subject to the concurrence of the enrollee.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1370.4, 1374.30 and 1374.33, Health and Safety Code.
HISTORY
1. New section filed 2-18-2003; operative 3-20-2003 (Register 2003, No. 8).
2. New subsection (f)(4) and amendment of subsection (g) filed 7-25-2005; operative 8-24-2005 (Register 2005, No. 30).
§1300.74.72. Mental Health Parity.
Note • History
(a) The mental health services required for the diagnosis, and treatment of conditions set forth in Health and Safety Code section 1374.72 shall include, when medically necessary, all health care services required under the Act including, but not limited to, basic health care services within the meaning of Health and Safety Code sections 1345(b) and 1367(i), and section 1300.67 of Title 28. These basic health care services shall, at a minimum, include crisis intervention and stabilization, psychiatric inpatient hospital services, including voluntary psychiatric inpatient services, and services from licensed mental health providers including, but not limited to, psychiatrists and psychologists.
(b) A plan shall provide coverage for the diagnosis and medically necessary treatment of conditions set forth in Health and Safety Code section 1374.72 through health care providers within the meaning of Health and Safety Code section 1345(i) who are:
(1) acting within the scope of their licensure, and
(2) acting within their scope of competence, established by education, training and experience, to diagnose, and treat conditions set forth in Health and Safety Code section 1374.72.
(c) A diagnosis within the meaning of Health and Safety Code section 1374.72 shall be made in accordance with professionally recognized diagnostic criteria including, but not limited to, the diagnostic criteria set forth in the Diagnostic and Statistical Manual for Mental Disorders -- IV -- Text Revision (June 2000).
(d) A preliminary or initial diagnosis made by a primary care physician, mental health provider or pediatrician meeting the requirements of subsection (b) above, that an enrollee has one or more of the conditions set forth in Health and Safety Code section 1374.72, shall constitute the diagnosis for the length of time necessary to make a final diagnosis, whether or not the final diagnosis confirms the preliminary or initial diagnosis.
(e) “Pervasive Developmental Disorders” shall include Autistic Disorder, Rett's Disorder, Childhood Disintegrative Disorder, Asperger's Disorder and Pervasive Developmental Disorder Not Otherwise Specified (including Atypical Autism), in accordance with the Diagnostic and Statistical Manual for Mental Disorders -- IV -- Text Revision (June 2000).
(f) A plan's referral system shall provide enrollees timely access and ready referral, in a manner consistent with good professional practice, to mental health services for the purpose of diagnosis and medically necessary treatment of conditions set forth in Health and Safety Code section 1374.72 and for related health care services as appropriate upon referral from a primary care physician, mental health provider or pediatrician meeting the requirements of subsection (b) above.
(g) If a plan contracts with a specialized health care service plan for the purpose of providing Health and Safety Code section 1374.72 services, the following requirements shall apply:
(1) the specialized health care service plan shall maintain a telephone number that an enrollee may call during normal business hours to obtain information about benefits, providers, coverage and any other relevant information concerning an enrollee's mental health services;
(2) if the plan issues identification cards to enrollees, the identification cards shall include the telephone number required to be maintained above and a brief statement indicating that enrollees may call the telephone number for assistance about mental health services and coverage;
(3) the plan shall monitor the continuity and coordination of care that enrollees receive, and take action, when necessary, to assure continuity and coordination of care, in a manner consistent with professionally recognized evidence-based standards of practice, across the health care network;
(4) the plan shall monitor, as often as necessary, but not less frequently than once every year, the collaboration between medical and mental health providers including, but not limited to, the following:
(A) exchange of information,
(B) appropriate diagnosis, treatment and referral, and
(C) access to treatment and follow-up for enrollees with co-existing medical and mental health disorders;
(5) the plan shall retain full responsibility for assuring continuity and coordination of care, in accordance with the requirements of this subsection, notwithstanding that, by contract, it has obligated a specialized health care service plan to perform some or all of these activities.
(h) Nothing in this section shall be construed to mandate coverage of services that are not medically necessary or preclude a plan from performing utilization review in accordance with the Act.
(i) A plan shall include in its Evidence of Coverage or Combined Evidence of Coverage and Disclosure Form a list of mental conditions required to be covered pursuant to Health and Safety Code section 1374.72.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1345, 1367 and 1374.72, Health and Safety Code.
HISTORY
1. New section filed 9-23-2003; operative 10-23-2003 (Register 2003, No. 39).
§1300.74.73. Pervasive Developmental Disorder and Autism Coverage.
Note • History
Health plans subject to Section 1374.73 of the Act shall comply with this section.
(a) Requirements
(1) For health plans that provide hospital, medical or surgical coverage under contract with the Healthy Families Program or the Board of Administration of the California Public Employees' Retirement System, section 1374.73 of the Act does not affect, reduce or limit the obligation to provide coverage for the diagnosis and medically necessary treatment of pervasive developmental disorder (PDD) and autism, including medically necessary behavioral health treatment, pursuant to Health and Safety Code section 1374.72.
(2) Nothing in subdivision (a)(1) of this section shall be construed to mandate coverage of services that are not medically necessary or preclude a plan from performing utilization review in accordance with the Act.
(3) Each health plan that is subject to the requirements of section 1374.73 of the Act shall submit a report to the Department no later than December 31, 2012, demonstrating that the health plan has an adequate network of qualified autism service providers, qualified autism service professionals and/or qualified autism service paraprofessionals. The required report shall include the following information:
(A) The name of each qualified autism service provider entity or organization/group, listed by county and zip code. For each identified qualified autism service provider entity or organization/group, state the following information:
1. The number of individual qualified autism service providers available to the entity or organization/group;
2. The number of qualified autism service professionals available to the entity or organization/group; and,
3. The number of qualified autism service paraprofessionals available to the entity or organization/group.
(B) The number of the health plan's individual qualified autism service providers, listed by county and zip code. For each qualified autism service provider identified, state the following information:
1. The number of qualified autism service professionals available to the qualified autism service provider pursuant to Health and Safety Code section 1374.73(c)(4)(B); and,
2. The number of qualified autism service paraprofessionals available to the qualified autism service provider pursuant to Health and Safety Code section 1374.73(c)(5)(A).
(C) A description of how the health plan is determining provider network adequacy, including how geographic accessibility and timely access for health plan enrollees to medically necessary PDD and autism health care services is being met. This information should include:
1. Data describing the adequacy of the health plan's provider network for each region or service area, including utilization data and information on the health plan's enrollee population, such as age, gender and other relevant factors used by the health plan; and,
2. A description of the health plan's system for monitoring and evaluating provider network adequacy in each region or service area.
(D) Upon request, the health plan shall submit within 30 calendar days any additional information the Director may request to determine the adequacy of the plan's network to ensure that health plan enrollees are receiving medically necessary PDD and autism health care services, including timely screening, diagnosis, evaluation and treatment.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1345, 1367, 1374.72 and 1374.73, Health and Safety Code.
HISTORY
1. New section filed 9-6-2012 as an emergency; operative 9-6-2012 (Register 2012, No. 36). A Certificate of Compliance must be transmitted to OAL by 3-5-2013 or emergency language will be repealed by operation of law on the following day.
Article 9. Financial Responsibility
§1300.75. Agreements with Subsequent Providers. [Repealed]
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Stats. 1978, Ch. 285.
HISTORY
1. Repealer filed 9-27-79; effective thirtieth day thereafter (Register 79, No. 39).
§1300.75.1. Fiscal Soundness, Insurance, and Other Arrangements.
Note • History
(a) A plan shall demonstrate fiscal soundness and assumption of full financial risk as follows:
(1) Demonstrate through its history of operations and through projections (which shall be supported by a statement as to the facts and assumptions upon which they are based) that the plan's arrangements for health care services and the schedule of its rates and charges are financially sound, and provide for the achievement and maintenance of a positive cash flow, including provisions for retirement of existing and proposed indebtedness.
(2) Demonstrate that its working capital is adequate, including provisions for contingencies.
(3) Demonstrate an approach to the risk of insolvency which allows for the continuation of benefits for the duration of the contract period for which payment has been made, the continuation of benefits to subscribers and enrollees who are confined on the date of insolvency in an in-patient facility until their discharge, and payments to unaffiliated providers for services rendered.
(b) As a part of its program pursuant to subsection (a), a plan may obtain insurance or make other arrangements:
(1) For the cost of providing to any member covered health care services the aggregate value of which exceeds $5,000 in any year;
(2) For the cost of covered health care services provided to its members other than through the plan because medical necessity required their provision before they could be secured through the plan; and
(3) For not more than 90 percent of the amount by which its costs for any of its fiscal years exceed 115 percent of its income for such fiscal year.
(c) In passing upon a plan's showing pursuant to this section, the Director will consider all relevant factors, including but not limited to:
(1) The method of compensating providers and the terms of provider contracts, especially as to the obligations of providers to subscribers and enrollees in the event of plan insolvency.
(2) The methods by which the plan controls and monitors the utilization of health care services.
(3) The administrative expenses (actual and projected) of the plan and especially as to new or expanding plans, the fiscal soundness of its program to acquire and service an expanded subscriber population.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1375.1, Health and Safety Code.
HISTORY
1. Repealer and new section filed 9-27-79; effective thirtieth day thereafter (Register 79, No. 39).
2. Amendment filed 12-8-82; effective thirtieth day thereafter (Register 82, No. 50).
3. Change without regulatory effect amending subsection (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.75.2. Plan As Subsequent Provider. [Repealed]
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Stats. 1978, Ch. 285.
HISTORY
1. Repealer filed 9-27-79; effective thirtieth day thereafter (Register 79, No. 39).
§1300.75.3. Subsequent Provider Exemption. [Repealed]
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Stats. 1978, Ch. 285.
HISTORY
1. Repealer filed 9-27-79; effective thirtieth day thereafter (Register 79, No. 39).
Note • History
As used in these Solvency Regulations:
(a) “External party” means the Department of Managed Health Care or its designated agent, which may be contracted or appointed to fulfill the functions stated in these Solvency Regulations. Whenever these Solvency Regulations reference the Department of Managed Health Care that reference means the Department of Managed Health Care (Department) or its designated agent.
(b) “Organization” means a risk-bearing organization as defined in Health and Safety Code Section 1375.4(g).
(c) “Plan” means full-service health care service plan, as defined by Health and Safety Code section 1345(f).
(d) “Risk arrangement” is defined to include both “risk-sharing arrangement” and “risk-shifting arrangement,” which are defined as follows:
(1) “Risk-sharing arrangement” means any compensation arrangement between an organization and a plan under which the organization shares the risk of financial gain or loss with the plan.
(2) “Risk-shifting arrangement” means a contractual arrangement between an organization and a plan under which the plan pays the organization on a fixed, periodic or capitated basis, and the financial risk for the cost of services provided pursuant to the contractual arrangement is assumed by the organization.
(e) “Solvency Regulations” means sections 1300.75.4 through 1300.75.4.8 of Title 28 of the California Code of Regulations.
(f) “Cash-to-claims ratio” is an organization's cash, readily available marketable securities and receivables, excluding all risk pool, risk-sharing, incentive payment program and pay-for-performance receivables, reasonably anticipated to be collected within 60 days divided by the organization's unpaid claims (claims payable and incurred but not reported [IBNR] claims) liability.
(g) “Corrective action plan” (CAP) means a plan reflected in a document containing requirements for correcting and monitoring an organization's efforts to correct any financial solvency deficiencies in the Grading Criteria or other financial or other claims payment deficiencies, determined through the Department's review or audit process, indicating that the organization may lack the capacity to meets its contractual obligations consistent with the requirements of section 1300.70(b)(2)(H)(1) of Title 28, California Code of Regulations.
(h) “Grading Criteria” means the four grading/reviewing criteria specified in Health and Safety Code sections 1375.4(b)(1)(A)(i), (ii), (iii), and (iv) and the cash-to-claims ratio as defined in subsection (f) above.
(i) “In a manner that does not adversely affect the integrity of the contract negotiation process” means the disclosure of an organization's financial data submissions in a format that does not impair the organization's ability to negotiate its contracts for the delivery of health care services or does not allow a contracting party to calculate: (1) an organization's precise profit/loss margins on any line of business, or (2) the rates that the organization has negotiated with any contracting entity or vendor during a prior accounting period.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Section 1375.4, Health and Safety Code.
HISTORY
1. New section filed 3-22-2001 as an emergency; operative 3-22-2001 (Register 2001, No. 12). A Certificate of Compliance must be transmitted to OAL by 7-20-2001 or emergency language will be repealed by operation of law on the following day.
2. Certificate of Compliance as to 3-22-2001 order, including amendment of subsection (d)(1), transmitted to OAL 7-20-2001 and filed 8-31-2001 (Register 2001, No. 35).
3. Amendment of first paragraph and subsections (a)-(e) and new subsections (f)-(i) filed 8-10-2005; operative 9-9-2005 (Register 2005, No. 32).
4. Change without regulatory effect amending subsection (i) filed 12-14-2005 pursuant to section 100, title 1, California Code of Regulations (Register 2005, No. 50).
§1300.75.4.1. Risk Arrangement Disclosure.
Note • History
(a) Every contract involving a risk arrangement between a plan and an organization shall require the plan to do all of the following:
(1) Disclose through electronic transmission (or in writing, if agreeable to both the organization and the plan) to the organization, on a monthly basis, beginning with the month of May, 2001, within 10 calendar days of the beginning of each report month, the following information for each enrollee assigned to the organization: member identification number, name, birth date, gender, address (including zip code), plan contract selected, employer group identification, the identity of any other third party coverage, if known to the health plan, enrollment/disenrollment dates, medical group/IPA number, provider effective date, type of change to coverage, co-payment, deductible, the amount of capitation to be paid per enrollee per month, and the primary care physician when the selection of a primary care physician is required by the plan.
(2) Disclose through electronic transmission (or in writing, if agreeable to both the organization and the plan) to the organization, on a monthly basis, beginning with the month of May, 2001, within 10 calendar days of the beginning of each report month, the names, member identification numbers, and total numbers of enrollees added or terminated under each benefit plan contract served by the organization.
(3) If the information provided in paragraphs (1) and (2) is provided in more than one report, the plan will disclose through electronic transmission (or in writing, if agreeable to both the organization and the plan) to the organization, on a quarterly basis, within 45 calendar days of the close of each quarter, a reconciliation of the variances between the information provided in paragraphs (1) and (2) above. Beginning no later than January 1, 2002, if the information in paragraphs (1) and (2) is provided in more than one report, all reports shall be processed as of the same date.
(4) On or before October 1, 2001, and annually thereafter on the contract anniversary date, disclose to the organization, for the purpose of assisting the organization to be informed regarding the financial risk assumed under the contract, the following information for each and every type of risk arrangement (Medicare+Choice, Medi-Cal, traditional commercial, Point of Service, small group, and individual plans) under the contract:
(A) a matrix of responsibility for medical expenses (physician, institutional, ancillary, and pharmacy) which will be allocated to the organization, facility, or the plan under the risk arrangement;
(B) expected/projected utilization rates and unit costs for each major expense service group (inpatient, outpatient, primary care physician, specialist, pharmacy, home health, durable medical equipment (DME), ambulance and other), the source of the data and the actuarial methods employed in determining the utilization rates and unit costs by benefit plan type for the type of risk arrangement; and
(C) all factors used to adjust payments or risk-sharing targets, including but not limited to the following: age, sex, localized geographic area, family size, experience rated, and benefit plan design, including copayment/deductible levels.
(5) Beginning with the first quarter of calendar year 2001, disclose through electronic transmission (or in writing, if agreeable to both the organization and the plan) to the organization, on a quarterly basis, within 45 calendar days of the close of each quarter, a detailed description of each and every amount (including expenses and income) that is sufficient to allow verification of the amounts allocated to the organization and to the plan under each and every risk-sharing arrangement. Where applicable, the following information, at a minimum, shall be provided: 1. the total number of member months; 2. the total budget allocation for the member months; 3. the total expenses paid during the period; 4. a description of the incurred but not reported (IBNR) claims methodology used for incurred expenses during the period; and 5. a description of each and every amount of expense allocated to the risk arrangement by member identification number, date of service, description of service by claim codes, net payment and date of payment.
(6) For all risk-sharing arrangements, provide the organization with a preliminary payment report consistent with the requirements of paragraph (5) no later than 150 days and payment no later than 180 days after the close of the organization's contract year, or the contract termination date, whichever occurs first.
(b) In addition to the disclosures required by subsection (a) of this regulation, every contract involving a risk-sharing arrangement between a plan and an organization shall require the plan to disclose, on or before October 1, 2001, and annually thereafter on the contract anniversary date, the amount of payment for each and every service to be provided under the contract, including any fee schedules or other factors or units used in determining the fees for each and every service. To the extent that reimbursement is made pursuant to a specified fee schedule, the contract shall incorporate that fee schedule by reference, and further specify the Medicare RBRVS year if RBRVS is the methodology used for fee schedule development. For any proprietary fee schedule, the contract must include sufficient detail that payment amounts related to that fee schedule can be accurately predicted.
(c) In addition to the disclosures required by subsection (a) of this regulation, every contract involving a risk-shifting arrangement between a plan and an organization shall require the plan to disclose, on or before October 1, 2001, and annually thereafter on the contract anniversary date, in the case of capitated payment, the amount to be paid per enrollee per month. For any deductions that the plan may take from any capitation payment, details sufficient to allow the organization to verify the accuracy and appropriateness of the deduction shall be provided.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Section 1375.4, Health and Safety Code.
HISTORY
1. New section filed 3-22-2001 as an emergency; operative 3-22-2001 (Register 2001, No. 12). A Certificate of Compliance must be transmitted to OAL by 7-20-2001 or emergency language will be repealed by operation of law on the following day.
2. Certificate of Compliance as to 3-22-2001 order, including amendment section, transmitted to OAL 7-20-2001 and filed 8-31-2001 (Register 2001, No. 35).
§1300.75.4.2. Organization Information.
Note • History
Every contract involving a risk arrangement between a plan and an organization shall require the organization to do the following:
(a) Beginning January 1, 2006 maintain at all times a minimum “cash-to-claims ratio,” as defined in section 1300.75.4(f), of 0.60 that shall be increased according to the following schedule:
(1) Beginning on July 1, 2006 the minimum cash-to-claims ratio shall be 0.65; and
(2) Beginning on January 1, 2007 and thereafter the minimum cash-to-claims ratio shall be 0.75.
(b) Quarterly Financial Survey. For each quarter beginning on or after July 1, 2005 submit to the Department, not more than forty-five (45) days after the close of each quarter of the fiscal year, a quarterly financial survey report in an electronic format to be supplied by the Department of Managed Health Care (Department) pursuant to section 1300.41.8 of Title 28, California Code of Regulations, containing all of the following:
(1) For organizations serving at least 10,000 covered lives under all risk arrangements as of December 31 of the preceding calendar year:
(A) Financial survey report (including a balance sheet, an income statement, and a statement of cash flows), or in the case of a nonprofit entity comparable financial statements and supporting schedule information (including but not limited to, aging of receivable information), reflecting the results of operations for the immediately preceding quarter, prepared in accordance with generally accepted accounting principles (GAAP) and the identification of the individual or office in the organization designated to receive public inquiries. Financial survey reports of an organization required pursuant to these rules shall be on a combining basis with an affiliate, if the organization or such affiliate is legally or financially responsible for the payment of the organization's claims. Any affiliated entity included in this report shall be separately identified reported in a combining schedule format. For the purposes of this section, an organization's use: 1. of a “sponsoring organization” arrangement to reduce its liabilities for the purposes of calculating tangible net equity and working capital or 2. an affiliated entity to provide claims processing services shall not be construed to automatically create a legal or financial obligation to pay the claims liability for the health care services for enrollees.
(B) A statement as to what percentage of completed claims the organization has timely reimbursed, contested, or denied during the quarter in accordance with the requirements of Health and Safety Code sections 1371, and 1371.35, section 1300.71 of Title 28 of the California Code of Regulations, and any other applicable state and federal laws and regulations. If less than 95% of all complete claims have been reimbursed, contested or denied on a timely basis, the statement shall be accompanied by a report that describes the reasons why the claims adjudication process is not meeting the requirements of applicable law, any action taken to correct the deficiency, and any results of that action. This claims payment report is for the purpose of monitoring the financial solvency of the organization and is not intended to change or alter existing state and federal laws and regulations relating to claims payment settlement practices and timeliness.
(C) A statement as to whether or not: 1. the organization has estimated and documented, on a monthly basis, its liability for IBNR claims, pursuant to a method specified in section 1300.77.2, and 2. the estimates are the basis for the quarterly financial survey report submitted under these Solvency Regulations. If the estimated and documented liability has not met the requirements of section 1300.77.2 in any way, a statement shall be included in the quarterly financial survey report that describes in detail the following with respect to each deficiency: the nature of the deficiency, the reasons for the deficiency, the action taken to correct the deficiency, and the results of that action. An organization failing: a. to estimate and document, on a monthly basis, its liability for IBNR claims or b. to maintain its books and records on an accrual accounting basis shall be deemed to have failed to maintain, at all times, positive tangible net equity (TNE) and positive working capital as set forth in subsection (D) below.
(D)1. A statement as to whether or not the organization has at all times during the quarter maintained positive TNE, as defined in section 1300.76(e) of Title 28 California Code of Regulations; and has at all times during the quarter maintained positive working capital, calculated in a manner consistent with GAAP. If either the required TNE or the required working capital has not been maintained at all times, a statement shall be included in the quarterly financial survey report that describes in detail the following, with respect to each deficiency: the nature of the deficiency, the reasons for the deficiency, any action taken to correct the deficiency, and any results of that action.
2. The organization may reduce its liabilities or increase its cash for purposes of calculating its TNE, working capital and cash-to-claims ratio in a manner allowed by Health and Safety Code section 1375.4(b)(1)(B) so long as the sponsoring organization has filed with the Department: a. its audited annual financial statements within 120 days of the end of the sponsoring organization's fiscal year and b. a copy of the written guarantee meeting the requirements of Health and Safety Code section 1375.4(b)(1)(B). For purposes of Health and Safety Code section 1375.4(b)(1)(B), a sponsoring organization shall have a TNE of at least twice the total of all amounts that it has guaranteed to all persons and entities, or a lesser amount in situations where the organization can demonstrate to the Director's satisfaction and written approval that a lesser amount of TNE is sufficient. If an organization has a sponsoring organization, the organization shall provide information to the Department demonstrating the capacity of the sponsoring organization to guarantee the organization's debts, as well as the nature and scope of the guarantee provided, consistent with Health and Safety Code section 1375.4(b)(1)(B).
(E) For the quarter beginning on or after January 1, 2006, a statement as to whether or not the organization has, at all times during the quarter, maintained a cash-to-claims ratio as required in section (a), calculated in a manner consistent with GAAP. If the required cash-to-claims ratio has not been maintained at all times, a statement shall be included in the quarterly financial survey report that describes in detail the following with respect to the deficiency: the nature of the deficiency, the reasons for the deficiency, any action taken to correct the deficiency, and any results of that action.
(2) For organizations serving less than 10,000 covered lives under all risk arrangements as of December 31 of the preceding calendar year:
(A) The disclosure statement(s) set forth in sections (b)(1)(B), (C), (D) and (E) above.
(B) In the event an organization serving less than 10,000 covered lives under all risk arrangements: 1. fails to satisfactorily demonstrate its compliance with the Grading Criteria; 2. experiences an event that materially alters the organization's ability to remain compliant with the Grading Criteria; 3. is found, by the external party's review or audit activities, to potentially lack sufficient financial capacity to continue to accept financial risk for the delivery of health care services consistent with the requirements of section 1300.70(b)(2)(H)(1); or 4. is found, through the Department's HMO Help Center, medical audits and surveys, or any other source, to be delaying referrals, authorizations, or access to basic health care services based on financial considerations, the organization shall, within 30 calendar days of the Department's written request, begin submitting complete quarterly financial survey reports pursuant to section 1300.75.4.2(b)(1).
(c) Annual Financial Survey.
(1) Regardless of the number of covered lives served under all risk arrangements, submit to the Department, not more than one hundred fifty (150) days after the close of the organization's fiscal year beginning on or after January 1, 2005, and not more than one hundred fifty (150) days after the close of each of the organization's subsequent fiscal years, an annual financial survey report in an electronic format to be supplied by the Department pursuant to section 1300.41.8 of Title 28 California Code of Regulations, based upon the organization's annual audited financial statement prepared in accordance with generally accepted auditing standards, and containing all of the following:
(2) Annual financial survey report, based upon the organization's annual audited financial statements (including at least a balance sheet, an income statement, a statement of cash flows, and footnote disclosures), or in the case of a nonprofit entity, comparable financial statements, and supporting schedule information, (including, but not limited, to aging of receivable information and debt maturity information), for the immediately preceding fiscal year, prepared by the independent certified public accountant in accordance with GAAP.
(3) Financial survey reports of an organization required pursuant to these Solvency Regulations shall be on a combining basis with an affiliate if the organization or such affiliate is legally or financially responsible for the payment of the organization's claims. Any affiliated entity included in the report shall be separately identified. For the purposes of this section, an organization's use of: (A) a “sponsoring organization” arrangement to reduce its liabilities for the purposes of calculating TNE and working capital or (B) an affiliated entity to provide claims processing services shall not be construed to automatically create a legal or financial obligation to pay claims liability for health care services for enrollees.
1. When combined financial statements are required by this regulation, the independent accountant's report or opinion must address all the entities included in the combined financial statements. If the accountant's report or opinion makes reference to the fact that another auditor performed a part of the examination, the organization shall also file the report or opinion issued by the other auditor.
2. For purposes of determining the independence of the certified public accountant, the regulations of the California State Board of Accountancy (Division 1, sections 1 through 99.2, Title 16, California Code of Regulations), shall apply.
(4) The opinion of the independent certified public accountant indicating: (A) whether the organization's annual audited financial statements present fairly, in all material respects, the financial position of the organization, and whether the financial statements were prepared in accordance with GAAP. If the opinion is qualified in any way, the survey report shall include an explanation regarding the nature of the qualification.
(5) A statement as to whether or not the organization has estimated and documented, on a monthly basis, its liability for IBNR claims, pursuant to a method specified in section 1300.77.2, and that these estimates are the basis for the financial survey reports submitted under these Solvency Regulations. If the estimated and documented liability has not met the requirements of section 1300.77.2, a statement shall be included in the annual financial survey report that describes in detail the following with respect to each deficiency: the nature of the deficiency, the reasons for the deficiency, the action taken to correct the deficiency, and the results of that action. An organization failing: (A) to estimate and document, on a monthly basis, its liability for IBNR claims, or (B) to maintain its books and records on an accrual accounting basis, shall be deemed to have failed to maintain, at all times, positive TNE and positive working capital as set forth in subsection (6)(A) below.
(6)(A) A statement as to whether or not the organization has, at all times during the year, maintained positive TNE, as defined in section 1300.76(e); and has, at all times during the year, maintained positive working capital, calculated in a manner consistent with GAAP. If either the required TNE or the required working capital has not been maintained at all times, a statement shall be included in the annual financial survey report that describes in detail the following with respect to each deficiency: the nature of the deficiency, the reasons for the deficiency, any action taken to correct the deficiency, and any results of that action.
(B) The organization may reduce its liabilities for purposes of calculating its TNE and working capital in a manner allowed by Health and Safety Code section 1375.4(b)(1)(B), so long as the sponsoring organization has filed, with the Department: 1. its audited annual financial statements within 120 days of the end of the sponsoring organization's fiscal year and 2. a copy of the written guarantee meeting the requirements of Health and Safety Code section 1375.4(b)(1)(B). For purposes of Health and Safety Code section 1375.4(b)(1)(B), a sponsoring organization shall have a TNE of at least twice the total of all amounts that it has guaranteed to all persons and entities, or a lesser amount in situations where the organization can demonstrate to the Director's satisfaction and written approval that a lesser amount of TNE is sufficient. If an organization has a sponsoring organization, the organization shall provide information to the Department demonstrating the capacity of the sponsoring organization to guarantee the organization's debts as well as the nature and scope of the guarantee provided consistent with Health and Safety Code section 1375.4(b)(1)(B).
(7) For the fiscal year beginning on or after January 1, 2006, a statement as to whether or not the organization has at all times during the year maintained a cash-to-claims ratio as required in section (a), calculated in a manner consistent with GAAP. If the required cash-to-claims ratio has not been maintained at all times, a statement shall be included in the quarterly financial survey report that describes in detail the following with respect to the deficiency: the nature of the deficiency, the reasons for the deficiency, any action taken to correct the deficiency, and any results of that action.
(8) A statement as to whether the organization maintains reinsurance and/or professional stop-loss coverage.
(9) The annual financial survey report shall include, as an attachment, a copy of the complete annual audited financial statement, including footnotes and the certificate or opinion of the independent certified public accountant.
(d) Statement of Organization Survey. Submit to the external party, a “Statement of Organization,” in an electronic format, prepared by the Department, to be filed along with the annual financial survey report, which shall include the following information, as of December 31 of each calendar year prior to the filing:
(1) Name and address of the organization;
(2) A financial and public contact person, with title, address, telephone number, fax number, and e-mail address;
(3) A list of all health plans with which the organization maintains risk arrangements;
(4) Whether the organization is an Independent Practice Association (IPA), Medical Group, Foundation, other entity, or some combination thereof. If the organization is a foundation, identify each and every medical group within the foundation, and whether any of those medical groups independently qualifies as a risk-bearing organization as defined in Health and Safety Code section 1375.4(g);
(5) Whether the organization is a professional corporation, partnership, not-for-profit corporation, sole proprietor, or other form of business;
(6) The name, business address and principal officer of each of the organization's affiliates as defined in Title 28, California Code of Regulations, section 1300.45(c)(1) and (2);
(7) Whether the organization is partially or wholly owned by a hospital or hospital system;
(8) A matrix listing all major categories of medical care offered by the organization, including, but not limited to, anesthesiology, cardiology, orthopedics, ophthalmology, oncology, obstetrics/gynecology and radiology.
(A) Next to each listed category in the matrix, a disclosure of the primary compensation model (salary, fee-for-service, capitation, other) used by the organization to compensate the majority of providers of that category of care;
(9) An approximation of the number of enrollees served by the organization under a risk arrangement, pursuant to a list of ranges developed by the Department;
(10) Any Management Services Organization (MSO) that the organization contracts with for administrative services;
(11) The total number of contracted physicians in employment and/or contractual arrangements with the organization;
(12) Disclosure of the organization's primary service area (excluding out-of-area tertiary facilities and providers) by California county or counties;
(13) The identification of the organization's address, telephone number and website link, if available, where providers may access written information and instructions for filing of provider disputes with the organization's Dispute Resolution Mechanism consistent with requirements of section 1300.71.38 of Title 28, California Code of Regulations; and,
(14) Provide any other information that the Director deems reasonable and necessary, as permitted by law, to understand the operational structure and finances of the organization.
(e) Submit a written verification for each report made under subsections (b), (c), and (d) of this section stating that the report is true and correct to the best knowledge and belief of a principal officer of the organization, and signed by a principal officer, as defined by section 1300.45(o) of Title 28, California Code of Regulations.
(f) Notify the Department and each contracting health plan no later than five (5) business days after discovering that the organization has experienced any event that materially alters its financial situation or threatens its solvency.
(g) Permit the Department to make any examination that it deems reasonable and necessary to implement Health and Safety Code section 1375.4, and provide to the Department, upon request, any books or records deemed relevant or useful to implementing this section for inspection and copying, as permitted by law.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Section 1375.4, Health and Safety Code.
HISTORY
1. New section filed 8-10-2005; operative 9-9-2005 (Register 2005, No. 32). For prior history, see Register 2002, No. 28.
Note • History
(a) Plan Quarterly Survey. Every plan that contracts with an organization shall, by May 15, 2001, and not more than forty-five (45) days after the close of each subsequent calendar quarter, submit a quarterly survey report in an electronic format to the Director listing all its contracting organizations, including their names, addresses, contact persons, telephone numbers, and number of enrollees assigned to the organization as of the last day of the quarter being reported.
(b) Plan Annual Survey. Along with the quarterly report due May 15, 2001, and for the report due by May 15 of each subsequent year (i.e., an annual reporting period), every plan shall submit an annual survey report in an electronic format to the Director, containing the following information, as of December 31 of the prior calendar year, for each organization with which the plan has a risk arrangement:
(1) For the plan's commercial, Medicare+Choice, and Medi-Cal product lines, the report shall disclose, in a separate matrix for each product line, the allocation of risk between the plan, the organization, and the facility by major expense category. For each of the plan's commercial, Medicare+Choice, and Medi-Cal product lines, the report shall disclose the number of covered lives and the counties primarily served by the organization.
(2) The report shall disclose whether the plan provides stop-loss insurance to the organization, and if so, the nature of any and all stop-loss arrangements.
(c) Each quarterly and annual survey report and matrix submitted to the Department shall include a written verification stating that the plan has complied with all the risk arrangement disclosure requirements of section 1300.75.4.1 and that the survey report or matrix is true and correct to the best knowledge and belief of a principal officer of the plan, and signed by a principal officer, as defined by regulation 1300.45(o) of Title 28 of the California Code of Regulations.
(d) Upon request, the plan shall provide any additional information that the Director may from time to time require to understand the type, amount, or appropriateness, of the financial risk assumed by the plan's contracting organizations.
(e) Every plan that contracts with an organization shall have adequate procedures in place to ensure that the plan notifies the Department of Managed Health Care or its designated agent no later than five (5) business days from discovering that any of its contracting organizations experienced any event which materially alters the organization's financial situation, or threatens its solvency.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Section 1375.4, Health and Safety Code.
HISTORY
1. New section filed 3-22-2001 as an emergency; operative 3-22-2001 (Register 2001, No. 12). A Certificate of Compliance must be transmitted to OAL by 7-20-2001 or emergency language will be repealed by operation of law on the following day.
2. Certificate of Compliance as to 3-22-2001 order, including amendment section, transmitted to OAL 7-20-2001 and filed 8-31-2001 (Register 2001, No. 35).
§1300.75.4.4. Confidentiality.
Note • History
(a) Financial and other records produced, disclosed or otherwise made available by an organization pursuant to Health and Safety Code section 1375.4, and to these Solvency Regulations shall be received and maintained on a confidential basis and protected from public disclosure, unless the Director makes a specific finding that the information can be released in a manner that does not adversely affect the integrity of the contract negotiation process; except that the organization's annual audited financial statement as required by section 1300.75.4.2(c) shall be permanently maintained on a confidential basis.
(b) The Director has determined that the disclosure of the following information in the format provided below will not adversely affect the integrity of an organization's contract negotiation process and, therefore, will be made available to the public as follows:
(1) Within 120 days following each reporting period due date, the Department of Managed Health Care (Department) will make the following information available, on its website, for public inspection:
(A) A list of all provider organizations currently identified as risk-bearing organizations;
(B) A list of all risk-bearing organizations that have submitted substantially complete financial survey forms, if required, and whether the risk-bearing organization's submission reflects that the organization has met or not met each of the Grading Criteria, as follows:
1. The designation of “met” to be assigned for each Grading Criteria met by the organization;
2. The designation of “not met” to be assigned for each Grading Criteria not met by the organization;
3. The disclosure of whether the organization has implemented and is compliant with a final CAP designed to remedy any deficiencies reported in the Grading Criteria;
4. The relative working capital of each organization, consistent with section 1300.75.4(h), presented as a ratio of current assets divided by current liabilities;
5. The relative tangible net equity (TNE) of each organization, consistent with section 1300.75.4(h), presented as a ratio of tangible net assets divided by total liabilities;
6. Claims payment timeliness in a percentage format, consistent with section 1300.75.4.(h), reflecting the amount of claims that the organization is paying on a timely basis; and,
7. To the extent feasible, each financial item described in paragraphs 1. through 5. shall be presented for both the current and the four previous reporting periods, following the effective date of these regulations.
(C) A list of all “non-compliant” organizations that fail to substantially comply with the reporting obligations, including the submission of the financial survey reports specified in section 1300.75.4.2 of Title 28, California Code of Regulations; and
(D) All information contained in the Statement of Organization of a risk-bearing organization, except responses to sections 1300.75.4.2(d)(8)(A), (d)(14) and financial documentation provided pursuant to section 1300.75.4.2 (d)(4); and
(E) Comparative, aggregated data on all organizations, and information that enables consumers to assess an organization's relative financial viability in a format that does not identify any individual organizations and consistent with section 1300.75.4.4 of Title 28, California Code of Regulations.
(c) Information received and maintained on a confidential basis pursuant to this section may be disclosed by the Director under the following circumstances:
(1) To other local, state or federal regulatory or law-enforcement agencies in accordance with the law;
(2) When necessary or appropriate in any proceeding or investigation conducted by the Department to enforce the provisions of the Knox-Keene Act;
(3) In the event that an organization publicly questions or challenges the Department's decision to approve or disapprove an organization's proposed CAP submitted in accordance with section 1300.75.4.8 of Title 28 of the California Code of Regulations, the Department may release the relevant portions of the organization's financial information to explain the Department's decision; and,
(4) Upon a determination by the Director, pursuant to Health and Safety Code section 1375.4(b)(7), that the justification for the confidential treatment no longer exists, provided that the information that is disclosed is at least two (2) years old.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Section 1375.4, Health and Safety Code.
HISTORY
1. New section filed 8-10-2005; operative 9-9-2005 (Register 2005, No. 32). For prior history, see Register 2002, No. 28.
§1300.75.4.5. Plan Compliance.
Note • History
(a) Every plan that maintains a risk arrangement with an organization shall have adequate procedures in place to ensure:
(1) That plan personnel review all reports and financial information made available pursuant to Health and Safety Code section 1375.4 and these Solvency Regulations as part of the plan's responsibility to evaluate and ensure the financial viability of its arrangements consistent with section 1300.70(b)(2)(H)(1) of Title 28, California Code of Regulations;
(2) That appropriate action(s) are taken following the Department's written notification to an organization's contracting health plan(s) that:
(A) The organization has failed to substantially comply with the reporting obligations specified in section 1300.75.4.2 of Title 28, California Code of Regulations, by failing to file a required periodic financial and organizational information disclosure, including the filing of an annual financial survey report based upon an audited financial statement prepared in accordance with generally accepted accounting principles (GAAP), or by failing to include significant portions of information on a required periodic financial organizational information disclosure;
(B) The organization has refused to permit the activities of the Department as specified in Health and Safety Code section 1375.4 or in these Solvency Regulations; or,
(C) The organization has failed to substantially comply with the requirements of a final CAP for a period of more than 90 days, as determined by the Department.
(3) Appropriate action shall include, but is not limited to, a prohibition on the assignment or addition of any additional enrollees to the risk arrangement with that organization without the prior written approval of the Director. The prohibition on assignments of additional enrollees to an organization pursuant to subsection (2) shall not apply to dependents of enrollees who are already under the risk-arrangement with the organization or to enrollees who selected the organization during an open enrollment or other selection period that was prior to the effective date of the prohibition on the assignment of additional enrollees. The prohibition on the assignment of additional enrollees shall take effect thirty (30) days after the date of Department's notification to the organization's contracting plan(s), and shall remain in effect until the Department notifies the organization's contracting health plan in writing that the organization's non-compliance has been remedied.
(4) That the plan complies with the corrective action process and cooperates in the implementation of a final CAP, including, but not limited to, implementing contingency plans for continuous delivery of health care services to plan enrollees served by the organization.
(5) That the plan shall advise the Department and the organization in writing within five (5) days of becoming aware: 1. that a contracting organization is not in compliance with the requirements of a final CAP, or 2. that an organization's conduct may cause the plan to be subject to disciplinary action pursuant to Health and Safety Code section 1386.
(6) That if a plan proposes to transfer plan enrollees receiving care from an organization that is compliant with a final CAP to alternative providers and the reassignment is based, in part, on the organization's failure to meet one or more of the Grading Criteria, the plan shall, prior to transferring enrollees from that organization, file with the Department a Block Transfer Filing pursuant to Health and Safety Code section 1373.65. In addition to all other criteria for reviewing block transfers, the Director may disapprove, postpone or suspend the plan's proposed transfer of enrollees if the department reasonably determines:
(A) That the proposed reassignment of enrollees will likely cause the organization's failure or result in the organization ceasing operations within three (3) months;
(B) That the organization has the financial and administrative capacity to provide timely access to care through an adequate network of qualified health care providers; and
(C) That the organization is not denying or delaying basic health care services or continuity of care for the plan's enrollees assigned to the organization.
(7) Notwithstanding subsection (6) of this section, nothing in these regulations shall limit or impair 1. the Director's authority, consistent with Health and Safety Code sections 1367, 1373.65 (b) and 1391.5, to require a plan to reassign or transfer plan enrollees to alternate providers or organizations on an expedited basis to avoid imminent harm to enrollees; 2. an enrollee's right to self-select a new provider; or 3. the plan's ability to transfer individual enrollees assigned to a provider who terminates his/her relationship with the organization to ensure that the enrollee receives appropriate continuity of care.
(b) Every contract involving a risk arrangement between a plan and an organization shall provide that an organization's failure to substantially comply with the contractual requirements required by these Solvency Regulations shall constitute a material breach of the risk arrangement contract. A plan shall not request or accept a waiver of any the contractual requirements set forth in these Solvency Regulations.
(c) Within 30 days of notification pursuant to section 1300.75.4.5(a)(2)(C) of Title 28, California Code of Regulations, a plan shall submit to the Department a specific Provider Transition Plan for the deficient organization which provides for the continuity of care for plan enrollees served by the organization.
(d) Any failure of a plan to comply with the requirements of Health and Safety Code section 1375.4 and these Solvency Regulations shall constitute grounds for disciplinary action against the plan pursuant to Health and Safety Code section 1386.
(e) The Director may seek and employ any combination of remedies and enforcement procedures provided under the Knox-Keene Act to enforce Health and Safety Code section 1375.4 and these Solvency Regulations.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Section 1375.4, Health and Safety Code.
HISTORY
1. New section filed 3-22-2001 as an emergency; operative 3-22-2001 (Register 2001, No. 12). A Certificate of Compliance must be transmitted to OAL by 7-20-2001 or emergency language will be repealed by operation of law on the following day.
2. Certificate of Compliance as to 3-22-2001 order transmitted to OAL 7-20-2001 and filed 8-31-2001 (Register 2001, No. 35).
3. Repealer and new section filed 8-10-2005; operative 9-9-2005 (Register 2005, No. 32).
§1300.75.4.6. Department Costs.
Note • History
The Department's costs incurred in the administration of Health and Safety Code Sections 1347.15 and 1375.4 shall come from amounts paid by plans, except specialized plans, pursuant to Health and Safety Code Section 1356.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Sections 1347.15, 1356 and 1375.4, Health and Safety Code.
HISTORY
1. New section filed 3-22-2001 as an emergency; operative 3-22-2001 (Register 2001, No. 12). A Certificate of Compliance must be transmitted to OAL by 7-20-2001 or emergency language will be repealed by operation of law on the following day.
2. Certificate of Compliance as to 3-22-2001 order transmitted to OAL 7-20-2001 and filed 8-31-2001 (Register 2001, No. 35).
§1300.75.4.7. Organization Evaluation.
Note • History
(a) Every contract involving a risk arrangement between a plan and an organization shall:
(1) Require the organization to comply with the Department of Managed Health Care's review and audit process, in determining the organization's satisfaction of the Grading Criteria; and
(2) Permit the Department to perform any of the following activities in conjunction with the plan's oversight process:
(A) Obtain and evaluate supplemental financial information pertaining to the organization when: 1. the organization fails to satisfactorily demonstrate its compliance with the Grading Criteria; 2. the organization experiences an event that materially alters its ability to remain compliant with the Grading Criteria; 3. the external party's review or audit process indicates that the organization may have insufficient financial capacity to continue to accept financial risk for the delivery of health care services consistent with the requirements of sections 1300.70(b)(2)(H)(1) of Title 28, California Code of Regulations; or 4. the Department receives information from complaints submitted to the HMO Help Center, health plan reporting, medical audits and surveys or any other source that indicates the organization may be delaying referrals or authorizations or failing to meet access standards for basic health care services based on financial considerations.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Section 1375.4, Health and Safety Code.
HISTORY
1. New section filed 8-10-2005; operative 9-9-2005 (Register 2005, No. 32).
§1300.75.4.8. Corrective Action.
Note • History
Every contract involving a risk arrangement between a plan and an organization shall require the plan and the organization to comply with a process, set forth in this regulation and administered by the Department, for the development and implementation of Corrective Action Plans (CAPs).
(a) Unless the organization has proactively demonstrated to the Department's written satisfaction that necessary and prudent capital investments has or may cause a temporary deficiency in its TNE, working capital or cash-to-claims ratios and that it has implemented an appropriate business plan that will correct the deficiency within a reasonable time period without causing a deficiency in its claim payment timeliness, beginning with the financial survey submission filed for the third quarter of calendar year 2005, organizations reporting deficiencies in any of the Grading Criteria shall simultaneously submit a self-initiated CAP proposal, in an electronic format developed by the Department, to the Department and every plan with which the organization maintains a contract involving a risk arrangement that meets the following requirements:
(1) Identifies the Grading Criteria that the organization has failed to meet;
(2) Identifies the amount by which the organization has failed to meet the Grading Criteria;
(3) Identifies all plans with which the organization has contracts involving a risk arrangement, including the identification of the name, title, telephone and facsimile numbers, and postal and e-mail addresses for the person responsible at each contracting health plan for monitoring compliance with the final CAP;
(4) Describes the specific actions the organization has taken or will take to correct any deficiency identified in subsections (1) and (2) of this section. This description should include any written representations made by contracting health plans to assist the organization in the implementation of its CAP. The actions shall be appropriate and reasonable in scope and breadth depending upon the nature and degree of the deficiency, and acceptable to the Department;
(5) Describes the timeframe for completing the corrective action and specifies a schedule for submitting progress reports to the Department and the organization's contracting health plans. Except in situations where the organization can demonstrate to the Department's satisfaction and written approval that an extended period of time is necessary and appropriate to correct the deficiency, that:
(A) Timetables specified in the self-initiated CAP for correcting working capital deficiencies shall not exceed 12 months;
(B) Timetables specified in the self-initiated CAP for correcting tangible net equity (TNE) deficiencies shall not exceed 12 months;
(C) Timetables specified in the self-initiated CAP for incurred but not reported (IBNR) deficiencies shall not exceed three (3) months;
(D) Timetables specified in the self-initiated CAP for correcting claims timeliness deficiencies shall not exceed six (6) months;
(E) Timetables specified in the self-initiated CAP for correcting cash-to-claims ratio deficiencies shall not exceed twelve (12) months.
(6) Identifies the name, title, telephone and facsimile numbers, and postal and e-mail addresses for the person responsible at the organization for ensuring compliance with the final CAP; and
(7) Describe:
(A) the organization's patient record retention and storage policies;
(B) the procedures and the steps the organization will take to ensure that patient medical records are appropriately stored and maintained; and
(C) the procedures and the steps the organization will take to ensure that patient medical records will be readily available and transferable to patients in the event the organization ceases operations or the organization fails to meet its obligations set forth in the final CAP. At a minimum, an organization's patient medical records policies and procedures shall be consistent with existing laws relating to the responsibilities for the preservation and maintenance of medical records and the protection of the confidentiality of medical information.
(b) To the extent possible, the self-initiated CAP proposal shall be set forth in a single document that addresses the concerns of all plans with which the organization maintains a contract that includes a risk arrangement.
(c) Unless, within 15 days of the receipt of an organization's self-initiated CAP proposal, a contracting health plan provides written notice to the Department and the risk-bearing organization stating the reason for its objections and recommendations for revisions, the self-initiated CAP shall be considered a final CAP, subject to the Department's approval process as set forth in sections (g) and (h) below.
(d) In the event that a contracting health plan files a written objection with the Department and the risk-bearing organization, the organization shall within twenty (20) days: (1) implement all corrective action strategies contained in its self-initiated CAP proposal that were not objected to by a contracting health plan; and (2) submit to each of its contracting health plans and the Department a revised CAP proposal that addresses the concerns raised by the objecting contracting health plan(s). To the extent possible, the revised CAP proposal shall be prepared as a single document that addresses the concerns of all plans with which the organization maintains a contract that includes a risk arrangement.
(e) Each contracting health plan shall have ten (10) days to submit to the organization and the Department its objections and recommended revisions, in an electronic format prepared by the Department, to the self-initiated revised CAP proposal.
(f) Within fifteen (15) days of receipt of any contracting health plans' objections and recommended revisions to the revised CAP proposal, the Department shall schedule a meeting (“CAP Settlement Conference”) with the organization and all of its contracting health plans to discuss and reconcile the differences.
(g) Within seven (7) days of the CAP Settlement Conference, the organization shall submit a final self-initiated CAP proposal to all of its contracting health plans and the Department.
(h) Within ten (10) days of receipt of the organization's final self-initiated CAP proposal, the external party shall submit its recommendation to the Department to approve, disapprove or modify the organization's final self-initiated CAP proposal.
(i) Within ten (10) days of receipt of the external party's recommendation, the Department shall approve, disapprove or modify the organization's final self-initiated CAP proposal, which shall then become the final CAP. If the Department does not act upon the recommendations of the external party within ten (10) days, the external party's recommendation shall be deemed approved.
(j) A final CAP shall remain in effect until the organization demonstrates compliance with the requirements of the CAP, or the CAP expires in accordance with its own terms.
(k) In addition to the CAP requirements specified in subsection (a) above, the Department may direct an organization to initiate a CAP whenever its determines that an organization has experienced an event that materially alters its ability to remain compliant with the Grading Criteria or when the Department's review process indicates that the organization may lack sufficient financial capacity to meet its contractual obligations consistent with the requirements of section 1300.70(b)(2)(11)(1) of Title 28 of the California Code of Regulations.
(l) CAP Reporting:
(1) Each periodic progress report prepared pursuant to a final CAP shall be submitted to the Department and all plans with which the organization has a contract involving a risk arrangement, and shall include a written verification stating that the periodic progress report is true and correct to the best knowledge and belief of a principal officer of the organization, as defined by section 1300.45(o) of Title 28 California Code of Regulations.
(2) In addition to the quarterly progress reports specified in a CAP, every contract involving a risk arrangement between a plan and an organization shall require that:
(A) the organization advise the plan and the Department in writing within five (5) days if the organization experiences an event that materially alters the organization's ability to remain compliant with the requirements of a final CAP; and
(B) the organization, upon the Department's request, provides additional documentation to the Department and its contracting plans to demonstrate the organization's progress towards fulfilling the requirements of a CAP.
(3) Non-disclosure of CAP documentation and supporting work papers:
(A) All draft, preliminary and final CAPs and all CAP compliance reports required by a final CAP, including supporting documentation and supplemental financial information, submitted to the Department shall be received and maintained on a confidential basis and shall not be disclosed, except for the information outlined in section 1300.75.4.4(c)(3) to any party other than the organization and, as necessary, to its contracting health plans that are participating in the CAP.
NOTE
Authority cited: Sections 1344 and 1375.4, Health and Safety Code. Reference: Section 1375.4, Health and Safety Code.
HISTORY
1. New section filed 8-10-2005; operative 9-9-2005 (Register 2005, No. 32).
§1300.76. Plan Tangible Net Equity Requirement.
Note • History
(a) Except as provided in subsection (b) or (c), each plan licensed pursuant to the provisions of the Act shall, at al times, have and maintain a tangible net equity at least equal to the greater of:
(1) $1 million; or
(2) the sum of two percent of the first $150 million of annualized premium revenues plus one percent of annualized premium revenues in excess of $150 million; or
(3) an amount equal to the sum of:
(A) eight percent of the first $150 million of annualized health care expenditures except those paid on a capitated basis or managed hospital payment basis; plus
(B) four percent of the annualized health care expenditures, except those paid on a capitated basis or managed hospital payment basis, which are in excess of $150 million; plus
(C) four percent of annualized hospital expenditures paid on a managed hospital payment basis.
(b) Except as provided in subsection(c), each plan licensed pursuant to the provisions of the Act and which only offers specialized health care service contracts shall, at all times, have and maintain a tangible net equity at least equal to the greater of:
(1) $50,000; or
(2) the sum of two percent of the first $7,500,000 of annualized premium revenues plus one percent of annualized premium revenues in excess of $7,500,000; or
(3) an amount equal to the sum of:
(A) eight percent of the first $7,500,000 of annualized health care expenditures, except those paid on a capitated or managed hospital payment basis; plus
(B) four percent of the annualized health care expenditures, except those paid on a capitated basis or managed hospital payment basis, which are in excess of $7,500,000; plus
(C) four percent of annualized hospital expenditures paid on a managed hospital payment basis.
(c) Each plan licensed pursuant to the provisions of the Act prior to the effective date of this section must maintain a minimum tangible net equity of:
(1) 20 percent of the amount required by subsection (a) or (b), as applicable within 6 months of the effective date of this section.
(2) 36 percent of the amount required by subsection (a) or (b), as applicable within 12 months of the effective date of this section.
(3) 52 percent of the amount required by subsection (a) or (b), as applicable within 18 months of the effective date of this subsection.
(4) 68 percent of the amount required in subsection (a) or (b), as applicable within 24 months of the effective date of this section.
(5) 84 percent of the amount required in subsection (a) or (b), as applicable within 30 months of the effective date of this section.
(6) 100 percent of the amount required in subsection (a) or (b), as applicable within 36 months of the effective date of this section.
(d) The Director may extend the time periods noted in subsection (c) if the Director determines that such extension is in the best interests of the plan and its enrollees and if it will not cause the plan to operated in a manner that may be hazardous to its enrollees.
(e) For the purpose of this section “net equity” means the excess of total assets over total liabilities, excluding liabilities which have been subordinated in a manner acceptable to the Director. “Tangible net equity” means net equity reduced by the value assigned to intangible assets including, but not limited to, goodwill; going concern value; organizational expense; starting-up costs; obligations of officers, directors, owners, or affiliates which are not fully secured, except short-term obligations of affiliates for goods or services arising in the normal course of business which are payable on the same terms as equivalent transactions with nonaffiliates and which are not past due; long term prepayments of deferred charges, and nonreturnable deposits. An obligation is fully secured for the purposes of this subsection if it is secured by tangible collateral, other than by securities of the plan or an affiliate, with an equity of at least 110 percent of the amount owing.
(f) For the purpose of this section, “capitated basis” means fixed per member per month payment or percentage of premium payment wherein the provider assumes the full risk for the cost of contracted services without regard to the type, value or frequency of services provided. For purposes of this definition, capitated basis includes the cost associated with operating staff model facilities.
(g) For the purpose of this section, “managed hospital payment basis” means agreements wherein the financial risk is primarily related to the degree of utilization rather than to the cost of services.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1376, Health and Safety Code.
HISTORY
1. Amendment of subsections (b) and (c) filed 4-27-79; effective thirtieth day thereafter (Register 79, No. 17).
2. Amendment of subsection (a), new subsections (b), (c),(d), (f) and (g), renumbering of former subsection (b) and repealer of former subsection (c) filed 12-14-90; operative 12-31-91 (Register 91, No. 6).
3. Editorial correction of printing error (Register 91, No. 17).
4. Change without regulatory effect amending subsections (d)-(e) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
Note • History
(a) Except as provided in subsection (b) or (c), each plan licensed pursuant to the provisions of the Act shall deposit with the Director or at the discretion of the Director with any bank authorized to do business in this state and insured by the Federal Deposit Insurance Corporation, or savings and loan association doing business in this state and insured by the Savings Association Insurance Fund, an amount which at all times shall have a value of not less than $300,000, except for plans which only offer specialized health care service contracts, which shall deposit an amount which at all times shall have a value of not less than $50,000. Cash, investment certificates, accounts, or any combination of these shall be assigned to the Director, upon those terms as the Director may prescribed, until released by the Director.
(b) Each plan licensed pursuant to the provisions of the Act prior to the effective date of this section, except any plan which only offers specialized health care services contracts, shall make a deposit of 50 percent of the amount required by subsection (a) within 12 months of the effective date of this section and 100 percent of the amount required by subsection (a) within 24 months of the effective date of this section.
(c) Each plan licensed pursuant to the provisions of the Act prior to the effective date of this section which only offers specialized health care service contracts shall make a deposit of 40 percent of the amount required by subsection (a) within 12 months of the effective date of this section, 70 percent of the amount required by subsection (a) within 24 months of the effective date of this section and 100 percent of the amount required by subsection (a) within 36 months of the effective date of this section.
(d) The Director may extend the time periods noted in subsection (c) if the Director determines that such extension is in the best interests of the plan and its enrollees and if it will not cause the plan to be operated in a manner that may be hazardous to its enrollees.
(e) The deposit required by subsection (a) shall be an allowable asset of the plan in the determination of tangible net equity and all income from the deposit shall be an asset of the plan.
(f) A plan that has made a deposit pursuant to subsection (a) may withdraw that deposit or any part thereof, after making a substitute deposit of cash, investment certificates, accounts or any combination of these. Any substitute deposit shall be approved by the Director before being deposited or substituted.
(g) The deposits shall be used to protect the interests of the plan's enrollees and to assure continuation of health care services to enrollees of a plan whenever the Director has brought actions pursuant to sections 1386, 1392, 1393 or 1394.1. The Director may use the deposit for administrative costs directly attributable to a conservatorship, receivership or liquidation.
NOTE
Authority cited: Section 1344, Health & Safety Code. Reference: Section 1376, Health & Safety Code.
HISTORY
1. New section filed 12-14-90; operative 12-31-90 (Register 91, No. 6).
2. Editorial correction of printing error (Register 91, No. 17).
3. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.76.2. Solicitor Firm Financial Requirement.
Note • History
(a) Each solicitor firm which handles funds of plans, subscribers, or other persons contracting with plans, shall at all times maintain a tangible net worth at least equal to 20 percent of such firm's aggregate indebtedness or $10,000, whichever is greater, and shall maintain liquid net assets of at least $5,000 in excess of it current liabilities.
(b) A solicitor firm which accepts only funds in the form of checks payable to plans, subscribers or other persons contracting with plans and forwards such checks to the payee by the close of the business day following receipt thereof does not “handle funds” within the meaning of this section.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1376, Health and Safety Code.
HISTORY
1. Editorial correction adding NOTE filed 12-8-82 (Register 82, No. 50).
Note • History
(a) Each plan shall at all times maintain a fidelity bond covering each officer, director, trustee, partner and employee of the plan, whether or not they are compensated. The fidelity bond may be either a primary commercial blanket bond or a blanket position bond written by an insurer licensed by the California Insurance Director, and it shall provide for 30 days' notice to the Director prior to cancellation. The fidelity bond shall provide at least the minimum coverage for the plan determined by the following schedule:
Annual Minimum
Gross Income Coverage
Up to $100,000 $10,000
100,000 to $300,000 20,000
300,000 to 500,000 30,000
500,000 to 750,000 50,000
750,000 to 1,000,000 75,000
1,000,000 to 2,000,000 100,000
2,000,000 to 4,000,000 200,000
4,000,000 to 6,000,000 400,000
6,000,000 to 10,000,000 600,000
10,000,000 to 20,000,000 1,000,000
20,000,000 and over 2,000,000
(b) The fidelity bond required pursuant to subsection (a) may contain a provision for a deductible amount from any loss which, except for such deductible provision, would be recoverable from the insurer. A deductible provision shall not be in excess of 10 percent of the required minimum bond coverage, but in no event shall the deductible amount be in excess of $100,000.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1376, Health and Safety Code.
HISTORY
1. Editorial correction adding NOTE filed 12-8-82 (Register 82, No. 50).
2. Change without regulatory effect amending subsection (a) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.76.4. Prohibited Financial Practices.
Note • History
(a) No solicitor shall maintain, and no plan or solicitor firm shall permit a solicitor in its employ to maintain, an account with a financial institution for funds of the plan, solicitor firm, subscribers or group representatives, except an account which is in the name of and under the control of the plan or solicitor firm.
(b) No solicitor shall receive funds on behalf of a plan or solicitor firm, and no plan or solicitor firm shall permit a solicitor in its employ to receive funds on behalf of the plan or solicitor firm, but this section shall not prohibit a solicitor from receiving only funds in the form of checks payable to the plan or solicitor firm if such solicitor deposits such checks to an account of the plan or solicitor firm by the close of the business day following receipt thereof or forwards such checks to the plan or solicitor firm by the close of the business day following receipt thereof.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1376, Health and Safety Code.
HISTORY
1. New section filed 11-9-77 as an emergency; effective upon filing (Register 77, No. 46).
2. Certificate of Compliance filed 2-6-78 (Register 78, No. 6).
3. Amendment filed 12-8-82; effective thirtieth day thereafter (Register 82, No. 50).
4. Amendment of NOTE filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
Note • History
(a) “Adequate insurance” for reimbursement for the purposes of subdivision (a)(2) of Section 1377 of the Act means a performance bond or insurance policy issued by an insurer licensed by the California Insurance Director, in an amount equal to at least the amount of cash, or cash equivalents, required to be maintained pursuant to subdivision (a)(1) of Section 1377 of the Act. The bond or insurance policy shall be payable to a corporate trustee for the benefit of noncontracting providers, subscribers and enrollees whose claims are unpaid upon the plan ceasing to do business because of insolvency or upon the plan being adjudged bankrupt.
(b) For the purposes of subdivision (a) of Section 1377 of the Act, “equivalents” to cash include only the following, provided that the investment in any one issuer of securities (other than securities issued or fully guaranteed or insured by the United States Government or any agency thereof) does not exceed 5% of the amount required pursuant to such subdivision:
(1) Shares listed on the New York Stock Exchange, the American Stock Exchange, the Pacific Stock Exchange or the O.T.C. Margin List, which shall be valued at 90 percent of their market value.
(2) Securities issued or guaranteed by the United States Government or any agency thereof, which shall be valued at the percentages of their market value specified below:
(A) less than 3 years to maturity 100%
(B) 3 or more years to maturity 98%
(3) Obligations of any state or political subdivision or
instrumentality thereof which are rated A or better by
Moody's Investors Service or A or better by Standard & Poor's,
which shall be valued at the percentages of their market value
specified below:
(A) less than 5 years to maturity 98%
(B) 5 or more years to maturity 95%
(4) Certificates of deposit or other evidence of deposit in, or acceptance of, a bank insured by the F.D.I.C. or certificates of deposit or share accounts of a savings and loan association insured by the F.S.L.I.C., which shall be valued at their book value.
(5) Promissory notes or other evidences of indebtedness having a maturity date within nine months of issuance, exclusive of days of grace, or any renewal thereof which is likewise limited, and which are rated P2 or better by Moody's Investors Service and A2 or better by Standard & Poor's, which shall be valued at their market value.
(6) Nonconvertible debt securities having a fixed maturity which are rated A or better by Moody's Investors Service or A or better by Standard & Poor's, which shall be valued at the percentages of their market value specified below:
(A) less than 2 years to maturity--100%
(B) 2 years but less than 5 years to maturity--98%
(C) 5 or more years to maturity--95%.
(c) The Director may waive the “haircut” requirements set forth in subsection (b) subject to the condition that the plan establish and maintain a securities valuation reserve fund consisting of cash or equivalents in an amount not less than 10 percent of the total amount of “cash and equivalents” required under Section 1377 which is not otherwise maintained in cash, or such other amount as the Director may require.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1377, Health and Safety Code.
HISTORY
1. Amendment of subsection (b) filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. New subsection (c) filed 12-8-82; effective thirtieth day thereafter (Register 82, No. 50).
3. Amendment filed 7-21-86; effective thirtieth day thereafter (Register 86, No. 30).
4. Change without regulatory effect amending subsection (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.77.1. Estimated Liability for Reimbursements.
Note • History
A plan subject to subdivision (b) of Section 1377 shall estimate its liability for incurred and unreported claims and record such estimate as an accrual in its books and records at least monthly.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1375.1, 1376 and 1377, Health and Safety Code.
HISTORY
1. Amendment filed 12-8-82; effective thirtieth day thereafter (Register 82, No. 50).
§1300.77.2. Calculation of Estimated Liability for Reimbursements.
Note • History
(a) Each plan subject to subdivision (b) of Section 1377 shall calculate the estimate of incurred and unreported claims pursuant to a method held unobjectionable by the Director. Such method may include a lag study as defined and illustrated in subsection (c), an actuarial estimate as defined in subsection (d), or other reasonable method of estimating incurred and unreported claims. The amount required by Section 1300.77.1 to be accrued in the plan's books and records must equal the estimated total of all claims incurred but not yet received as of the end of the month as calculated in working papers, schedules or reports prepared in support of the unobjectionable lag study, actuarial estimate, or other method of estimating incurred and unreported claims.
(b) Working papers which support the incurred and unreported claims calculation shall be maintained as part of the records of the plan. Lag study working papers shall include a detailed allocation of all claims received each month to the various months in which the services were performed. Actuarial estimate working papers must detail all underlying assumptions and calculations in establishing the actuarial rate. Any other method used to determine the amount of incurred and unreported claims must be supported by adequate working papers, schedules or reports which detail all aspects of the incurred and unreported calculation.
(c) A “lag study” is a schedule which analyzes historical claims information on an ongoing basis to determine the length of time lag between the date of service and the date a claim is submitted to the plan for payment. Such a study distributes all claims received each month in which the services were performed. An example of a lag study containing the minimum information necessary to be held unobjectionable by the Director is as follows:
ABC HEALTH PLAN OF CALIFORNIA
SCHEDULE TO CALCULATE HISTORIC PERCENTAGE
OF INCURRED BUT UNREPORTED CLAIMS FOR PRIOR
MONTHLY PERIODS WHICH HAVE BEEN FULLY OR
SUBSTANTIALLY REPORTED
JULY 31, 19X2
MONTH CLAIM RECEIVED
Totals for
Same Months of
Month 2nd 3rd 4th 5th 6th 7th Service
Month of Service:
Oct. 19X1 $150 $500 $200 $100 $50 $1,000
Nov. 19X1 220 500 240 110 30 1,110
Dec. 19X1 150 600 300 100 75 $25 1,250
Jan. 19X2 210 750 375 105 60 1,500
Feb. 19X2 230 670 290 85 100 75 1,450
Totals $960 $3,020 $1,405 $500 $315 $100 $6,300
Percentages:
Monthly 15% 48% 22% 8% 5% 2%
Cumulative 15% 63% 85% 93% 98% 100%
Explanatory notes:The above represents the first schedule that is prepared to determine the incurred and unreported claims for any month following February. The schedule allocates claims as they are received to the month in which the service was performed. For example, in October, the plan received $150 of claims which had service dates in October (same month). Because this schedule begins in October, the $150 amount would be the only entry which the plan would be able to make in October. In November, the plan received $220 in claims which had service dates in November (same month), and $500 of claims which had service dates in October (second month). In December, the plan received $150 of claims which had service dates in December (same month), $500 of claims which had service dates in November (second month), and $200 in claims which had service dates in October (third month). The schedule indicates that $6,300 in claims were received which had service dates of October through February. Of this amount, $960 was received during the month of service (same month), $3,020 in the following (second) month, $1,405 in the third month, $500 in the fourth month, etc. By converting these amounts to percentages of the total claims, the schedule indicates that on the average, 15% ($960 P $6,300 =) of all claims incurred during any month are received in the same month, 48% are received in the following (second) month, for a cumulative total of 63% (15% + 48% =) of all claims incurring during any month being received in the same and second months. By employing these cumulative percentages, the amount incurred but unreported claims can be estimated as of July 31, after the claims information for the current but incomplete monthly periods is analyzed, as illustrated in the following schedule:
ABC HEALTH PLAN OF CALIFORNIA
SCHEDULE TO ESTIMATE THE AMOUNT OF INCURRED
BUT UNREPORTED CLAIMS FOR THE CURRENT BUT
INCOMPLETE MONTHLY PERIODS WHICH HAVE NOT BEEN
FULLY OR SUBSTANTIALLY REPORTED
JULY 31, 19X2
MONTH CLAIM RECEIVED
Totals for
Same Months of
Month 2nd 3rd 4th 5th 6th 7th Service
Month of Service:
Mar., 19X2 $225 $720 $300 $120 $50 $1,415
April, 19X2 250 700 330 110 1,390
May, 19X2 240 750 350 1,340
June, 19X2 250 775 1,025
July, 19X2 270 270
Total Claims received for period March 1 through July 31 $5,440
COMPUTATION OF INCURRED
BUT UNREPORTED CLAIMS AS OF JULY 31
(A) (B) (C) (D) (E)
Claims received as
of July 31 as a
Total claims cumulative Total Incurred
Month received for each percentages claims to But unre-
of month of service of total claims be received ported
Service as of July 31 to be received (B-C) (D-B)
July $270 (i) 15% $1,800 $1,530
June 1,025 (ii) 63% 1,625 600
May 1,340 (iii) 85% 1,575 235
April 390 (iv) 93% 1,495 105
March 1,415 (v) 98% 1,440 25
February 1,450 (vi) 100% 1,450 0
Total incurred but unreported claims as of July 31 $2,495
Explanatory notes:(i) Represents July claims received in July. (ii) Represents June claims received in June and July. (iii) Represents May claims received in May, June and July. (iv)Represents April claims received in April, May, June and July. (v) Represents March claims received in March, April, May, June and July.(vi) Represents February claims received in February, March, April, May, June and July.
(d) An “actuarial estimate” is a calculation of incurred and unreported claims which is based on adequate and reasonable assumptions with respect to risk factors and trends which have been found to be applicable to the plan, such as utilization patterns of the plan's enrollees, the average benefit which will be payable, the enrollment mix in terms of age and sex of enrollees and geographic location, actual plan contract experience, and any other factors reasonably believed to affect the amount of incurred and unreported claims. Actuarial estimates must be supported by an actuarial certification, consisting of a signed declaration of any actuary who is a member in good standing of the American Academy of Actuaries in which such actuary states that the assumptions used in calculating the incurred and unreported claims are appropriate and reasonable. If the plan employs an actuarial study to estimate the amount of the incurred and un--reported claims, it must compare the actual claims amounts to those estimated, and make adjustments at least quarterly whenever a 5% difference from actual experience is noted.
(e) A plan may employ any other unobjectionable alternative method of estimating the amount of incurred and unreported claims other than the “lag study” or “actuarial estimate,” so long as such alternative method accurately estimates incurred and unreported claims. For example, a plan may receive daily reports of actual hospital admissions and referrals, thereby permitting the plan to compare these reports to the actual invoices and calculate the estimated amount due hospitals for the enrollees whose claims had not been received by the plan at that time.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1375.1, 1376 and 1377, Health and Safety Code.
HISTORY
1. New section filed 3-3-83; effective thirtieth day thereafter (Register 83, No. 10).
2. Change without regulatory effect amending subsections (a) and (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.77.3. Report on Reimbursements Exceeding Ten Percent.
Note • History
(a) Every plan which reimburses providers of health care services or subscribers and enrollees in the manner described in subdivision (a) or (b) of Section 1377 of the Act shall make and maintain as part of its records a computation for each calendar month and calendar quarter of reimbursements made, classified as provided in Section 1377, and showing the percentage of each class of reimbursements made to total expenditures for health care services during such month or quarter.
(b) When a report is required by subdivision (a) of Section 1377 of the Act, such report shall be filed with the Director no later than 30 business days after the close of the calendar quarter.
(c) When a report is required by subdivision (b) of Section 1377 of the Act, such report shall be filed with the Director no later than 30 business days after the close of the calendar month during which actual reimbursements made, or the amount estimated for incurred and unreported claims, exceeds 10 percent of its total expenditures for health care services.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1377, Health and Safety Code.
HISTORY
1. Editorial correction adding NOTE filed 12-8-82 (Register 82, No. 50).
2. Change without regulatory effect amending subsections (b) and (c) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.77.4. Reimbursements on a Fee-for-Services Basis: Determination of Status of Claims.
Note • History
Every plan shall institute procedures whereby all claim forms received by the plan from providers of health care services for reimbursement on a fee-for-service basis and from subscribers and enrollees for reimbursement are maintained and accounted for in a manner which permits the determination of the date of receipt of any claim, the status of any claim, the dollar amount of unpaid claims at any time, and rapid retrieval of any claim. Although any categories for status-determination held unobjectionable by the Director may be used, for the purposes of this section, the following status-determination categories, as a group, shall be presumptively reasonable:
(1) to be processed,
(2) processed, waiting for payment,
(3) pending, waiting for approval for payment or denial,
(4) pending, waiting for additional information,
(5) denied,
(6) paid, and, if appropriate,
(7) other. These procedures shall involve the use of either a claims log, claims numbering system, electronic data processing records, and/or any other method held unobjectionable by the Director.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1375.1, 1376 and 1377, Health and Safety Code.
HISTORY
1. New section filed 3-3-83; effective thirtieth day thereafter (Register 83, No. 10).
2. Change without regulatory effect amending first paragraph and subsection (7) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.78. Administrative Costs.
Note • History
(a) For the purposes of Section 1378 of the Act, “administrative costs” include only those costs which arise out of the operation of the plan as such, excluding direct and overhead costs incurred in the furnishing of health care services which would be ordinarily incurred in the provision of such services whether or not through a plan. Administrative costs include the following:
(1) Salaries, bonuses and benefits paid or incurred with respect to the officers, directors, partners, trustees or other principal management of the Plan, less to the extent that such persons also are providers of health care services, the minimum reasonable cost of obtaining such services from others.
(2) The cost of soliciting and enrolling subscribers and enrollees, including the solicitation of group contracts, and including any indirect costs of enrollment borne on behalf of the plan by the holder of a group contract.
(3) The cost of receiving, processing and paying claims of providers of health care services and of claims for reimbursement by subscribers and enrollees, excluding the actual amount paid on such claims.
(4) Legal and accounting fees and expenses.
(5) The premium on the fidelity and surety bonds, and any insurance maintained pursuant to Section 1377, and any insurance or other expense incurred for the purposes of complying with Section 1375 of the Act. Malpractice insurance is not included within this subsection.
(6) All costs associated with the establishment and maintenance of agreements with providers of health care services, excluding the cost of reviewing quality and utilization of such services, and the cost of reviewing utilization of health care services on a referral basis.
(7) The direct or pro rata portion of all expenses incurred in the operation of the plan which are not essential to the actual provision of health care services to subscribers and enrollees, including but not limited to office supplies and equipment, clerical services, interest expense, insurance, dues and subscriptions, licenses (other than licenses for medical facilities, equipment or personnel), utilities, telephone, travel, rent, repairs and maintenance, depreciation of facilities and equipment, and charitable or other contributions.
(b) The administrative cost incurred by a plan, directly, as herein defined, shall be reasonable and necessary, taking into consideration such factors as the plan's stage of development and other considerations. If the administrative costs of an established plan exceed 15 percent, or if the administrative costs of a plan in the development phase exceed 25 percent, during any period of the revenue obtained by the plan from subscribers and enrollees, or paid to the plan on their behalf, the plan shall demonstrate to the Director, if called upon to do so, that its administrative costs are not excessive administrative costs within the meaning of Section 1378 and are justified under the circumstances and/or that it has instituted procedures to reduce administrative costs which are proving effective. An established plan is a plan which has been in operation for a period of five years or more. For the purposes of Section 1378 of the Act, money borrowed will be deemed to be money derived from revenue obtained from subscribers and enrollees to the extent that such revenue is exposed to liability for repayment of such borrowings or that repayment is anticipated from such revenues and “money not derived from” such revenues includes only net assets arising independently of the operation of the plan and not traceable on a historical basis to such revenues, whether as net profit or otherwise.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1378, Health and Safety Code.
HISTORY
1. Editorial correction adding NOTE filed 12-8-82 (Register 82, No. 50).
2. Change without regulatory effect amending subsection (b) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
Article 10. Medical Surveys
§1300.80. Medical Survey Procedure.
Note • History
(a) Unless the Director in his discretion determines that advance notice will render the survey less useful, a plan will be notified approximately four weeks in advance of the date for commencement of an onsite medical survey. The Director may, without prior notice, conduct inspections of plan facilities or other elements of a medical survey, either in conjunction with the medical survey or as part of an unannounced inspection program.
(b) The onsite medical survey of a plan shall include, but not be limited to, the following procedures to the extent considered necessary based upon prior experience with the plan and in accordance with the procedures and standards developed by the Department.
(1) Review of the procedures for obtaining health services including, but not limited to, the scope of basic health care services.
(A) The availability and adequacy of facilities for telephone communication with health personnel, emergency care facilities, out-of-the-area coverage, referral procedures, and medical encounters.
(B) The means of advising enrollees of the procedures to obtain care, including the hours of operation, location and nature of facilities, types of care, telephone and other arrangements for appointment setting.
(C) The availability of qualified personnel at each facility referred to in Section 1368(b) to receive and handle inquiries concerning care, plan contracts, and grievances.
(2) Review of the design and implementation of procedures for reviewing and regulating utilization of services and facilities.
(3) Review of the design and implementation of procedures to review and control costs.
(4) Review of the design, implementation and effectiveness of the internal quality of care review systems, including review of medical records and medical records systems. A review of medical records and medical records systems may include, but is not limited to, determining whether:
(A) The entries establish the diagnosis stated, including an appropriate history and physical findings;
(B) The therapies noted reflect an awareness of current therapies;
(C) The important diagnoses are summarized or highlighted; (Important are those conditions that have a bearing on future clinical management.)
(D) Drug allergies and idiosyncratic medical problems are conspicuously noted;
(E) Pathology, laboratory and other reports are recorded;
(F) The health professional responsible for each entry is identifiable;
(G) Any necessary consultation and progress notes are evidenced as indicated;
(H) The maintenance of an appropriate system for coordination and availability of the medical records of the enrollee, including out-patient, in-patient and referral services and significant telephone consultations.
(5) Review of the overall performance of the plan in providing health care benefits, by consideration of the following:
(A) The numbers and qualifications of health professional and other personnel;
(B) The provision of, incentives for, and participation in, continuing education for health personnel and the provision for access to current medical literature;
(C) The adequacy of all physical facilities, including lighting, cleanliness, maintenance, equipment, furnishings, and convenience to enrollees, plan personnel and visitors;
(D) The practice of health professionals and allied personnel in a functionally integrated manner, including the extent of shared responsibility for patient care and coordinated use of equipment, medical records and other facilities and services;
(E) The appropriate functioning of health professionals and other health personnel, including specialists, consultants and referrals;
(F) Nursing practices, including reasonable supervision;
(G) Written nondiscriminatory personnel practices which attract and retain qualified health professionals and other personnel;
(H) The adequacy and utilization of pathology and other laboratory facilities, including the quality, efficiency and appropriateness of laboratory procedures and records and quality control procedures;
(I) X-ray and radiological services, including staffing, utilization, equipment, and the promptness of interpretation of X-ray films by a qualified physician;
(J) The handling and adequacy of medical record systems, including filing procedures, provisions for maintenance of confidentiality, the efficiency of procedures for retrieval and transmittal, and the utilization of sampling techniques for medical records audits and quality of care review;
(K) The adequacy, including convenience and readiness of availability to enrollees, of all provided services;
(L) The organization of the plan and its mechanisms for furnishing health care services, including the supervision of health professionals and other personnel;
(M) The extent to which individual medical decisions by qualified medical personnel are unduly constrained by fiscal or administrative personnel, policies or considerations;
(N) The adequacy of staffing, including medical specialties.
(6) Review of the overall performance of the plan in meeting the health needs of enrollees.
(A) Accessibility of facilities and services, based upon location of facilities, hours of operation, waiting periods for services and appointments, including elective services, the availability of parking and transportation;
(B) Continuity of care, including the ability of enrollees to select a primary care physician, staffing in medical specialties or arrangements therefor; the referral system (including instructions, monitoring and follow-up); the maintenance and ready availability of medical records; and the availability of health education to enrollees;
(C) The grievance procedure required by Section 1368 of the Act, including the availability to enrollees and subscribers of grievance procedure information, the time required for and the adequacy of the response to grievances and the utilization of grievance information by plan management.
(7) In considering the above and in pursuit of the survey objectives, the survey team may perform any or all of the following procedures:
(A) Private interviews and group conferences with enrollees, physicians and other health professionals, and members of its administrative staff including, but not limited to, its principal management persons.
(B) Examination of any records, books, reports and papers of the plan and of any management company, provider or subcontractor providing health care or other services to the plan including, but not limited to, the minutes of medical staff meetings, peer review, and quality of care review records, duty rosters of medical personnel, surgical logs, appointment records, the written procedures for the internal operation of the plan, and contracts and correspondence with enrollees and with providers of health care services and of other services to the plan, and such additional documentation the Director may specifically direct the surveyors to examine.
(C) Physical examination of facilities, including equipment.
(D) Investigation of grievances or complaints from enrollees or from the general public.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1380, Health and Safety Code.
HISTORY
1. Amendment of subsection (b)(7)(D) filed 12-8-82; effective thirtieth day thereafter (Register 82, No. 50).
2. Change without regulatory effect amending subsections (a) and (b)(7)(B) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.80.10. Medical Survey: Report of Correction of Deficiencies.
Note • History
Prior to or immediately upon the expiration of the 30-day period following notice to a plan of a deficiency as provided in subdivision (h) of Section 1380 of the Act, the plan shall file a written statement with the Director identifying the deficiency and describing the action taken to correct the deficiency and the results of such action. The report shall be signed by a principal officer of the plan.
Where such deficiencies may be reasonably adjudged to require long-term corrective action or to be of a nature which may be reasonably expected to require a period longer than 30 days to remedy, in some instances evidence that the plan has initiated remedial action and is on the way to achieving acceptable levels of compliance may be submitted.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1380, Health and Safety Code.
HISTORY
1. Amendment filed 12-8-8; effective thirtieth day thereafter (Register 82, No. 50).
2. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
Article 11. Examinations
§1300.81. Removal of Books and Records from State.
Note • History
The books and records of a plan, management company, solicitor firm, and any provider or subcontractor providing health care or other services to a plan, management company, or solicitor firm shall not be removed from this state without the prior consent of the Director.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1381, Health and Safety Code.
HISTORY
1. Amendment filed 12-8-82; effective thirtieth day thereafter (Register 82, No. 50).
2. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.82. Examination Procedure.
Note • History
Regular and additional or nonroutine examinations conducted by the Department pursuant to Section 1382 will ordinarily be commenced on an unannounced basis. To the extent feasible, deficiencies noted will be called to the attention of the responsible officers of the company under examination during the course of the examination, and in that event the company should take the corrective action indicated. When deemed appropriate, the company will be advised by letter of the deficiencies noted upon the examination. If the deficiency letter requires a report from the company, such report must be furnished within 15 days or such additional time as may be allowed.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1382, Health and Safety Code.
HISTORY
1. Amendment filed 12-8-82; effective thirtieth day thereafter (Register 82, No. 50).
§1300.82.1. Additional or Nonroutine Examinations and Surveys.
Note • History
(a) An examination or survey is additional or nonroutine for good cause for the purposes of Section 1382(b) when the reason for such examination or survey is any of the following:
(1) The plan's noncompliance with written instructions from the Department;
(2) The plan has violated, or the Director has reason to believe that the plan has violated, any of the provisions of Sections 1352, 1370, 1375.1, 1376, 1384 and 1385 of the Act and Sections 1300.76, 1300.80.10, 1300.81, 1300.82(a), 1300.84.2 and 1300.84.3 of these regulations.
(3) The plan has committed, or the Director has reason to believe that the plan has committed, any of the acts or omissions enumerated in Section 1386 of the Act.
(4) The Director deems such additional or nonroutine examination or survey necessary to verify representations made to this Department by a plan in response to a deficiency letter.
(b) Each situation giving rise to an additional or nonroutine examination or survey shall be evaluated on a case-by-case basis as to the seriousness of the violation, or lack of timely or adequate response by the plan to the Department's request to correct the violation. The plan shall be notified in writing of the provisions of the Act or regulations which have been, or may have been, violated and which therefore caused such additional or nonroutine examination or survey to be performed. The expense of such examinations and surveys shall be charged to the plan being examined or surveyed in accordance with Section 1382(b).
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1352, 1370, 1375.1, 1376, 1380, 1382, 1384, 1385 and 1386, Health and Safety Code.
HISTORY
1. New section filed 3-3-83; effective thirtieth day thereafter (Register 83, No. 10).
2. Change without regulatory effect amending subsections (a)(2)-(4) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
Article 12. Reports
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Stats. 1979, Ch. 1083.
HISTORY
1. Repealer filed 5-9-80; effective thirtieth day thereafter (Register 80, No. 19).
§1300.84. Financial Statements.
Note • History
(a) Whenever pursuant to these rules or pursuant to an order or request of the Director pursuant to the Act a financial statement or other report is required to be audited or be accompanied by the opinion of a certified public accountant or public accountant, such accountant shall be independent of the licensee, determined in accordance with section 602.02 of Financial Reporting Release Number 1 issued by the Securities and Exchange Commission.
(b) The financial statements required under subsections (a), (b) and (c) of Section 1384 of the Act shall be audited by an independent accountant in accordance with section 1300.45(e).
(c) Except as provided in subsection (d), financial statements of a plan required pursuant to these rules must be on a combining basis with an affiliate, if the plan or such affiliate is substantially dependent upon the other for the provision of health care, management or other services. An affiliate will normally be required to be combined, regardless of its form of organization, if the following conditions exist:
(1) The affiliate controls, is controlled by, or is under common control with, the plan, either directly or indirectly (see subsections (c) and (d) of section 1300.45), and
(2) The plan or the affiliate is substantially dependent, either directly or indirectly, upon the other for services or revenue.
(d) Upon written request of a plan, the Director may waive the requirement that an affiliate be combined in financial statements required pursuant to these rules. Normally, a waiver will be granted only when
(1) the affiliate is not directly engaged in the delivery of health care services or
(2) the affiliate is operating under an authority granted by a governmental agency pursuant to which the affiliate is required to submit periodic financial reports in a form prescribed by such governmental agency that cannot practicably be reformatted into the form prescribed by these rules (such as an insurance company).
(e) When combined financial statements are required by this section, the independent accountant's report or opinion must cover all the entities included in the combined financial statements. If the accountant's report or opinion makes reference to the fact that a part of the examination was performed by another auditor, the plan shall also file the individual financial statements and report or opinion issued by the other auditor.
(f) Plans which have subsidiaries that are required to be consolidated under generally accepted accounting principles must present either
(1) consolidating financial statements, or
(2) consolidating schedules for the balance sheet and statement of operations, which in either case must show the plan separate from the other entities included in the consolidated balances.
(g) This section shall not apply to a plan which is a public entity or political subdivision.
(h) All filings of financial statements required pursuant to these rules must include an original and one copy.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1384, Health and Safety Code.
HISTORY
1. Amendment filed 5-9-80; effective thirtieth day thereafter (Register 80, No. 19).
2. Amendment filed 7-3-84; effective thirtieth day thereafter (Register 84, No. 27).
3. Amendment of subsection (e) and new subsection (h) filed 7-21-86; effective thirtieth day thereafter (Register 86, No. 30).
4. Amendment of subsection (a) filed 12-14-90; operative 12-31-90 (Register 91, No. 6).
5. Change without regulatory effect amending subsections (a) and (d) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.84.05. Change of Independent Accountant.
Note • History
Whenever the financial statements required pursuant to subdivisions (a), (b) or (c) of Section 1384 are to be reported upon or certified by an accountant other than the accountant certifying the plan's most recent filing, the plan must furnish the Director with a separate letter stating whether in the eighteen (18) months preceding the engagement of the new accountants there was any disagreement with the former accountants on any matter of accounting principles or practices, financial statement disclosure or auditing procedures, which such disagreement if not resolved to the satisfaction of the former accountants would have caused him to make reference to the subject matter of such disagreement in his opinion or report. This letter must be verified by a principal officer of the plan. The plan shall also request the former accountants to furnish them with a letter addressed to the Director stating whether he agrees with the statements contained in the letter of the plan and, if not, stating the respects in which he does not agree. The notification by the plan along with the former accountant's letter, if necessary, must be furnished to the Director within 45 days of the engagement of the new accountants.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1345 and 1384, Health and Safety Code.
HISTORY
1. New section filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Change without regulatory effect amending section filed 7-14-99 pursuant to section 100, title 1, California Code of Regulations (Register 99, No. 29).
3. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.84.06. Plan Annual Report.
Note • History
The annual report required of a plan pursuant to subdivision (c) of section 1384 of the Act shall include or be accompanied by the following information for the period covered by the report, except as otherwise specified:
(a) The “Health Maintenance Organization Financial Report of Affairs and Conditions Form” as adopted by the National Association of Insurance Commissioners commonly known as the “HMO Annual Reporting Form” and the “Orange Blank” published by the Brandon Insurance Service Company. The “HMO Annual Reporting Form,” revised 1989, is incorporated by reference.
(b) Sufficient and appropriate supplemental information to provide adequate disclosure of at least the following:
(1) An explanation of the method of calculating the provision for incurred and unreported claims.
(2) Accounts and notes receivable from officers, directors, owners or affiliates, including the name of the debtor, nature of the relationship, nature of the receivable and its terms.
(3) Donated materials or services received by the plan for the period of the financial statements and the donor's name and affiliation with the plan, together with an explanation of the method used in determining the valuation of such materials or services.
(4) Forgiven debt or obligations during the period of the financial statements, including the creditor's name and affiliation with the plan and a summary of how the obligation arose.
(5) A calculation of the plan's tangible net equity in accordance with section 1300.76 of these rules. Such calculation shall include disclosure of the following information used to determine the required amount of tangible net equity pursuant to section 1300.76(a) and (b):
(A) Revenues
1. Two percent of the first $150 million, or $7.5 million for specialized plans, of annualized premium revenues;
2. One percent of annualized premium revenues in excess of $150 million, or $7.5 million for specialized plans;
3. Sum of 1. and 2. above.
(B) Healthcare Expenditures
1. Eight percent of the first $150 million, or $7,500,00 for specialized plans of annualized health care expenditures except those paid on a capitated basis or managed hospital payment basis.
2. Four percent of the annualized health care expenditures, except those paid on a capitated basis or managed hospital payment basis, which are in excess of $150 million, or $7,500,000 for specialized plans;
3. Four percent of annualized hospital expenditures paid on a managed hospital payment basis.
4. Sum of 1., 2. and 3. above.
(6) The percentage of administrative costs to revenue obtained from subscribers and enrollees.
(7) The amount of health care expenses incurred during the six month period immediately preceding the date of the report which were or will be paid to noncontracting providers or directly reimbursed to subscribers and enrollees.
(8) Total costs for health care services for the immediately preceding six months.
(9) If the amount of health care expenses incurred during the six month period immediately preceding the date of the report which were or will be paid to noncontracting providers or directly reimbursed to subscribers and enrollees exceeds 10% of the total costs for health care services for the immediately preceding six months, the following information, determined as of the date of the report, shall be provided:
(A) Amount of all claims for noncontracting provider services received for reimbursement but not yet processed.
(B) Amount of all claims for noncontracting provider services denied for reimbursement during the previous 60 days.
(C) Amount of all claims for noncontracting provider services approved for reimbursement but not yet paid.
(D) An estimate of the amount of claims for noncontracting provider services incurred, but not reported.
(E) A calculation of compliance with section 1377(a) as determined in accordance with such section.
NOTE
Authority cited: Sections 1344 and 1384, Health and Safety Code. Reference: Section 1384, Health and Safety Code.
HISTORY
1. New section filed 5-9-80; effective thirtieth day thereafter (Register 80, No. 19).
2. Amendment filed 7-21-86; effective thirtieth day thereafter (Register 86, No. 30).
3. Amendment filed 12-14-90; operative 12-31-90 (Register 91, No. 6).
§1300.84.1. Verification of Reports.
Note • History
NOTE
Authority cited: Sections 1344 and 1384, Health and Safety Code.
HISTORY
1. Repealer filed 7-21-86; effective thirtieth day thereafter (Register 86, No. 30).
§1300.84.2. Quarterly Financial Reports.
Note • History
Within 45 days after the close of each quarter of its fiscal year, each licensed plan shall file with the Director its report consisting of the following information:
(a) Financial statements (which need not be certified) prepared in accordance with generally accepted accounting principles, prepared on a basis consistent with the certified financial report furnished by the plan pursuant to Section 1384(c) of the Act, unless the plan receives the written approval of the Director to vary from that basis and the variance is adequately noted in its report under this section. The financial statements shall include the following statements, reports and schedules contained in the “HMO Annual Reporting Form” identified in Section 1300.84.06(a) of these rules for the period covered by the report:
(1) First page: “Statement”;
(2) Report #1-Part A: Balance Sheet Assets;
(3) Report #1-Part B: Balance Sheet Liabilities and Net Worth;
(4) Report #2: Statement of Revenue and Expenses;
(5) Report #3: Statement of Financial Position and Net Worth;
(6) Report #4: Enrollment and Utilization Table; and
(7) Section I of Schedule F: Unpaid Claims Analysis.
(b) The information required pursuant to Section 1300.84.06(b) of these rules for the period covered by the report, except as otherwise specified.
NOTE
Authority cited: Sections 1344 and 1384, Health and Safety Code. Reference: Section 1384, Health and Safety Code.
HISTORY
1. Amendment filed 5-9-80; effective thirtieth day thereafter (Register 80, No. 19).
2. Amendment filed 7-21-86; effective thirtieth day thereafter (Register 86, No. 30).
3. Change without regulatory effect amending first paragraph and subsection (a) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.84.3. Monthly Financial Reports.
Note • History
(a) Each plan shall maintain internal procedures which provide one or more of its principal officers on at least a monthly basis with the information necessary for the report required pursuant to this section.
(b) Each plan shall report to the Director the increase during any calendar quarter of the amount owed by the plan to providers for health care services, if the amount of such increase exceeds 10 percent of the amount owed at the close of the previous quarter. In the event the amount owed to a provider is disputed, the amount claimed as due by the provider shall control for the purposes of this section. This report shall be filed within 30 days after the close of the quarter for which the report is made.
(c) Each plan shall promptly advise the Director of any extraordinary loss, or of any claim whether or not admitted by the plan or a contingent claim, which
(1) renders the plan unable to meet its obligations as they become due, or
(2) reduces (or would reduce) the tangible net equity of the plan below the amount required by section 1300.76 of these rules.
(d) Each plan shall, upon the occurrence of any of the events specified below, file a report with the Director within 30 days of the close of the month for which such condition is noted, and each month thereafter until notified by the Director to discontinue such reports. Each such report shall consist of a balance sheet and statement of operations of the plan, which need not be certified, a calculation of tangible net equity in accordance with section 1300.76 of these rules, and the verification required by subsection (e) of this rule. Such financial statements must be prepared on a basis consistent with the financial statements furnished by the plan pursuant to section 1300.84.2 of these rules. The events the occurrence of which shall require reporting under this section are the following:
(1) The tangible net equity of the plan, individually or on a combined basis with affiliates (Rule 1300.84(c)), is less than the following:
(A) 200% of the minimum tangible net equity required by section 1300.76(c)(1);
(B) 155% of the minimum tangible net equity required by section 1300.76(c)(2);
(C) 148% of the minimum tangible net equity required by section 1300.76(c)(3);
(D) 137% of the minimum tangible net equity required by section 1300.76(c)(4);
(E) 136% of the minimum tangible net equity required by section 1300.76(c)(5);
(F) 130% of the minimum tangible net equity required by section 1300.76(c)(6);
(G) 130% of the minimum tangible net equity required by section 1300.76(a) or (b), as specified.
(2) The statement of operations of the plan, individually or on a combined basis with affiliates (Rule 1300.84(c)), reflects a loss during any month the amount of which exceeds the difference between the tangible net equity of the plan (or the combined entity) as of the end of such month and the minimum net equity required by Section 1300.76 of these rules.
(3) The plan has not been licensed for twelve (12) months.
(e) Each report required to be furnished by a plan pursuant to subsection (d) of this rule shall be verified by a principal officer of the plan as follows:
I certify (or declare) under penalty of perjury under the laws of the State of California that I have read this report and know the contents thereof, and that the statements therein are true and correct.
Executed at ____________________________________, on____________________
(Place) (Date)
(Signature)
NOTE
Authority cited: Sections 1344 and 1384, Health and Safety Code. Reference: Section 1384, Health and Safety Code.
HISTORY
1. Amendment of subsection (d) filed 6-2-78; effective thirtieth day thereafter (Register 78, No. 22).
2. Amendment of subsection (d) filed 7-3-84; effective thirtieth day thereafter (Register 84, No. 27).
3. Amendment filed 7-21-86; effective thirtieth day thereafter (Register 86, No. 30).
4. Change without regulatory effect of subsection (d) (Register 86, No. 38).
5. Amendment of subsection (d) filed 12-14-90; operative 12-31-90 (Register 91, No. 6).
6. Change without regulatory effect amending subsection (e) filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
7. Change without regulatory effect amending subsections (b), (c) and (d) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.84.4. Financial Reports by Solicitor Firms.
Note • History
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1384, Health and Safety Code.
HISTORY
1. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Repealer filed 7-3-84; effective thirtieth day thereafter (Register 84, No. 27).
§1300.84.5. Public Entity Plans.
Note • History
(a) A plan which is a public entity or political subdivision shall be subject to the provisions of this section.
(1) Financial statements of a plan which is a public entity or political subdivision, including financial statements or reports of specific funds or groups of accounts where health plan activity is recorded, which are required to be submitted pursuant to Section 1351(h) or 1384(c) of the Act or by rule, order or request of the Director, shall be accompanied either by an opinion of a certified public accountant or public accountant or by a report of a government audit organization.
(2) For the purposes of Sections 1351 and 1384, governmental auditing standards are defined to include the standards set forth in this item. Every audit which results in the opinion or report referred to in Item (1) of this subsection shall be conducted in accordance with the governmental auditing standards indicated below:
(A) General Standards:
(i) The auditors assigned to perform the audit must collectively possess adequate professional proficiency for the tasks required.
(ii) In all matters relating to the audit work, the audit organization and the individual auditors, whether government or public, must be free from personal or external impairments to independence, must be organizationally independent, and shall maintain an independent attitude and appearance.
(iii) Due professional care is to be used in conducting the audit and in preparing related reports.
(B) Standards of Field Work:
(i) The work is to be adequately planned and assistants, if any, are to be properly supervised.
(ii) There is to be a proper study and evaluation of the existing internal control as a basis for reliance thereon and for the determination of the resultant extent of the tests to which auditing procedures are to be restricted.
(iii) Sufficient competent evidential matter is to be obtained through inspection, observation, inquiries, and confirmations to afford a reasonable basis for an opinion regarding the financial statements under examination.
(C) Standards of Reporting:
(i) The report shall state whether the financial statements are presented in accordance with generally accepted accounting principles.
(ii) The report shall state whether such principles have been consistently observed in the current period in relation to the preceding period.
(iii) Informative disclosures in the financial statement are to be regarded as reasonably adequate unless otherwise stated in the report.
(iv) The report shall either contain an expression of opinion regarding the financial statements, taken as a whole, or an assertion to the effect that an opinion cannot be expressed. When an overall opinion cannot be expressed, the reasons therefor should be stated. In all cases where an auditor's name is associated with financial statements, the report should contain a clear-cut indication of the character of the auditor's examination, if any, and the degree of responsibility he is taking.
(D) Additional Standards and Requirements on Examination and Evaluation for Government Financial and Compliance Audits.
(i) Planning shall include consideration of the requirements of all levels of government.
(ii) A review is to be made of compliance with applicable laws and regulations.
(iii) A written record of the auditors' work shall be retained in the form of working papers.
(iv) Auditors shall be alert to situations or transactions that could be indicative of fraud, abuse, and illegal expenditures and acts and if such evidence exists, extend audit steps and procedures to identify the effect on the entity's financial statements.
(E) Additional Standards and Requirements on Reporting for Government Financial and Compliance Audits.
(i) Written audit reports are to be submitted to the appropriate officials of the organization audited and to the appropriate officials of the organizations requiring or arranging for the audits unless legal restrictions or ethical considerations prevent it. Copies of the reports should also be sent to other officials who may be responsible for taking action and to others authorized to receive such reports. Unless restricted by law or regulations, copies should be made available for public inspection.
(ii) A statement in the auditors' report that the examination was made in accordance with generally accepted government auditing standards for financial and compliance audits will be acceptable language to indicate that the audit was made in accordance with these standards.
(iii) Either the auditors' report on the entity's financial statements or a separate report shall contain a statement of positive assurance on those items of compliance tested and negative assurance on those items not tested. It shall also include material instances of noncompliance and instances or indications of fraud, abuse, or illegal acts found during or in connection with the audit.
(iv) The auditors shall report on their study and evaluation of internal accounting controls made as part of the financial and compliance audit. They shall identify as a minimum: (a) the entity's significant internal accounting controls, (b) the controls identified that were evaluated, (c) the controls identified that were not evaluated (the auditor may satisfy this requirement by identifying any significant classes of transactions and related assets not included in the study and evaluation), and (d) the material weaknesses identified as a result of the evaluation.
(v) Either the auditors' report on the entity's financial statements or a separate report shall contain any other material deficiency findings identified during the audit not covered in (ii) above.
(vi) If certain information is prohibited from general disclosure, the report shall state the nature of the information omitted and the requirement that makes the omission necessary.
(3) Financial statements, including reports of specific funds or groups of accounts, which are to be submitted pursuant to this section must be previously approved as to form by the Director. When all health plan activity has been separately controlled and accounted for in an Enterprise Fund, the financial statements or reports of such funds are presumptively approved as to form for purposes of this subsection.
(b) A plan which is a public entity or political subdivision shall be granted a total or partial exemption from Sections 1300.84.06 and 1300.84.2 upon proper application therefor, when and to the extent that
(1) the Director determines that such plan has demonstrated that the information set forth in Sections 1300.84.06 and 1300.84.2 is neither available to the plan nor necessary for its internal management and cannot be produced without significant cost to the plan, and
(2) such plan undertakes to furnish alternative information which the Director finds to be reasonable and adequate in view of the circumstances of the plan.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1345, 1351, 1384 and 1385, Health and Safety Code.
HISTORY
1. New section filed 5-9-80; effective thirtieth day thereafter (Register 80, No. 19).
2. Amendment filed 7-3-84; effective thirtieth day thereafter (Register 84, No. 27).
3. Change without regulatory effect amending subsections (a)(1), (a)(3) and (b)(1)-(2) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.84.6. Plan Annual Enrollee Report.
Note • History
(a) On or before May 15th of each year, each licensed plan shall file a report in the following form and containing the information specified therein:
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Sections 1356, 1384 and 1385, Health and Safety Code.
HISTORY
1. New section filed 5-9-80; effective thirtieth day thereafter (Register 80, No. 19).
2. Change without regulatory effect amending section filed 1-23-91 pursuant to section 100, title 1, California Code of Regulations (Register 92, No. 10).
3. Change without regulatory effect amending subsection (a) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
§1300.84.7. Special Reports Relating to Charitable or Public Activities.
Note • History
(a) Any plan whose purposes involve any charitable or public purposes shall provide a special report to the Director upon filing with the Attorney General any notice, request, or other materials pursuant to any law administered by the Attorney General and relating to matters which will or may have any financial effect on or implications for the plan. Such special report shall include the information provided to the Attorney General together with representations as to whether the transactions, actions, or other facts set forth in the materials submitted to the Attorney General will or may have any deleterious effect on the financial condition of the plan.
(b) Any plan whose purposes involved any charitable or public purposes shall provide a special report to the Director upon engaging in any transaction to which the corporation is a party and in which one or more of its directors has a material financial interest, if such transaction will or may have any material financial effect on or implications for the plan. Such special report shall specifically describe the transaction and shall contain representations as to whether the transaction will or may have any deleterious effect on the financial condition or operations of the plan.
(c) Any filing pursuant to this section may be combined with any appropriate filings pursuant to Article 2, Part 11, Division 2, Title 1 of the Corporations Code and may utilize common exhibits, subject to the provisions of Section 1300.824(c).
NOTE
Authority cited: Section 1344, Health and Safety Code, Reference: Section 1384, Health and Safety Code.
HISTORY
1. New section filed 4-16-82; effective thirtieth day thereafter (Register 82, No. 16).
2. Change without regulatory effect amending subsections (a) and (b) filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
Article 13. Books and Records
Note • History
(a) Each plan, solicitor firm, and solicitor shall keep and maintain their books of account and other records on a current basis.
(b) Each plan shall make or cause to be made and retain books and records which accurately reflect:
(1) The names and last known addresses of all subscribers to the plan.
(2) All contracts required to be submitted to the Department and all other contracts entered into by the plan.
(3) All requests made to the plan for payment of moneys for health care services, the date of such requests, and the dispositions thereof.
(4) A current list of the names and addresses of all individuals employed by it as a solicitor.
(5) A current list of the names and addresses of all solicitor firms with which it contracts.
(6) A current list of the names and addresses of all of the plan's officers, directors, principle shareholders, general managers, and other principle persons.
(7) The amount of any commissions paid to persons who obtain members for plans and the manner in which said commissions are determined.
(c) Each solicitor firm shall make and retain books and records which include a current list of the names and addresses of its partners, if any, and all of its employees who make act as solicitors.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1385, Health and Safety Code.
HISTORY
1. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
§1300.85.1. Retention of Books and Records.
Note • History
Every plan and solicitor firm shall preserve for a period of not less than five years, the last two years of which shall be in an easily accessible place at the offices of the plan or solicitor firm, the books of account and other records required under the provisions of, and for the purpose of the Act. After such books and records have been preserved for two years, they may be warehoused or stored, or microfilmed, subject to their availability to the Director within not more than 5 days after request therefore.
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1385, Health and Safety Code.
HISTORY
1. Change without regulatory effect amending section and adding Note filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
Article 14. Miscellaneous Provisions
§1300.86. Assessment of Administrative Penalties.
Note • History
(a) When assessing administrative penalties against a health plan the Director shall determine the appropriate amount of the penalty for each violation of the Act based upon one or more of the factors set forth in subsection (b).
(b) The factors referred to in subsection (a) include, but are not limited to the following:
(1) The nature, scope, and gravity of the violation;
(2) The good or bad faith of the plan;
(3) The plan's history of violations;
(4) The willfulness of the violation;
(5) The nature and extent to which the plan cooperated with the Department's investigation;
(6) The nature and extent to which the plan aggravated or mitigated any injury or damage caused by the violation;
(7) The nature and extent to which the plan has taken corrective action to ensure the violation will not recur;
(8) The financial status of the plan;
(9) The financial cost of the health care service that was denied, delayed, or modified;
(10) Whether the violation is an isolated incident; and/or
(11) The amount of the penalty necessary to deter similar violations in the future.
NOTE
Authority cited: Sections 1341, 1344 and 1386, Health and Safety Code. Reference: Section 1386, Health and Safety Code.
HISTORY
1. New section filed 11-8-2004; operative 12-8-2004 (Register 2004, No. 46).
Note • History
For purposes of section 1387 of the Health and Safety Code:
(a) A violation that is ongoing and continuous is subject to a civil penalty not to exceed two thousand five hundred dollars ($2,500) for each day that the violation continues.
(b) Each enrollee harmed by a violation of the Act constitutes a separate and distinct violation subject to a civil penalty not to exceed two thousand five hundred dollars ($2,500).
NOTE
Authority cited: Sections 1344 and 1387, Health and Safety Code. Reference: Section 1387, Health and Safety Code; and Section 11425.50, Government Code.
HISTORY
1. New section filed 9-18-2003; operative 9-18-2003 pursuant to Government Code section 11343.4 (Register 2003, No. 38).
§1300.89. Petition for Restoration.
Note • History
(a) The fee for the filing of a petition for restoration shall be $100 for a solicitor, $250 for a solicitor firm, and $500 for a plan.
(b) A petition for restoration shall be made upon the following form:
(c) If the petition provided in subsection (b) is filed by a plan, the plan shall file an amendment to its application on file with the Department which will bring that application current, or, if its application is current without the need for any amendment, it shall so allege.
(d) The Director may require additional information and/or undertakings as a condition of granting a petition for restoration. This requested material will be used to determine whether the petitioner, if restored, would engage in business in full compliance with the objectives and provisions of the Act and the applicable regulations. The Director, in evaluating the rehabilitation of the petitioner and his or her eligibility for a license or status as a solicitor, shall consider the following criteria:
(1) The nature and severity of the act(s) or offense(s).
(2) The administrative record applicable to the disciplinary proceedings.
(3) The time that has elapsed since commission of the act(s) or offense(s).
(4) Whether the petitioner has complied with any terms of parole, probation, restitution or any other sanctions imposed against him or her.
(5) If applicable, evidence of expungement proceedings pursuant to Section 1203.4 of the Penal Code.
(6) Evidence, if any, of rehabilitation submitted by the petitioner.
(7) Any other information or material that the Director deems to be appropriate and relevant.
NOTE
Authority cited; Section 1344, Health and Safety Code. Reference: Section 1389, Health and Safety Code.
HISTORY
1. New section filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
3. Change without regulatory effect updating title reference on sample execution page filed 12-22-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 51).
4. Change without regulatory effect amending subsection (b) filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
5. Amendment filed 12-16-2002; operative 1-15-2003 (Register 2002, No. 51).
§1300.99. Application to Surrender License.
Note • History
An application to surrender a license as a health plan shall be filed with the Director, in the following form:
NOTE
Authority cited: Section 1344, Health and Safety Code. Reference: Section 1399, Health and Safety Code.
HISTORY
1. Amendment filed 1-12-83; effective thirtieth day thereafter (Register 83, No. 3).
2. Amendment filed 7-3-84; effective thirtieth day thereafter (Register 84, No. 27).
3. Change without regulatory effect amending subsection (e) filed 4-4-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 14).
4. Change without regulatory effect amending section filed 7-18-2000 pursuant to section 100, title 1, California Code of Regulations (Register 2000, No. 29).
5. Change without regulatory effect amending section filed 11-21-2002 pursuant to section 100, title 1, California Code of Regulations (Register 2002, No. 47).
§1300.99.7. Application for Conversion or Restructuring.
Note • History
An application for conversion or restructuring pursuant to Article 11 (commencing with Section 1399.70) of the Act shall be filed as a Notice of Material Modification pursuant to Rule 1300.52.1.
NOTE
Authority cited: Sections 1344 and 1399.74, Health and Safety Code. Reference: Sections 1352, 1399.70, 1399.71, 1399.72, 1399.73, 1399.74 and 1399.75, Health and Safety Code.
HISTORY
1. New section filed 6-20-96 as an emergency; operative 6-20-96 (Register 96, No. 25). A Certificate of Compliance must be transmitted to OAL by 10-18-96 or emergency language will be repealed by operation of law on the following day.
2. New section refiled 10-15-96 as an emergency; operative 10-18-96 (Register 96, No. 42). A Certificate of Compliance must be transmitted to OAL by 2-12-97 or emergency language will be repealed by operation of law on the following day.
3. Certificate of Compliance as to 10-15-96 order transmitted to OAL 2-3-97 and filed 2-24-97 (Register 97, No. 9).
Article 15. Charitable or Public Activities
§1300.824. Requirements Relating to Charitable or Public Activity Filings.
Note • History
NOTE
Authority cited: Sections 10824 and 10826, Corporations Code. Reference: Sections 7238, 10824 and 10826, Corporations Code.
HISTORY
1. New Article 15 (Sections 1300.824-1300.826, not consecutive) filed 4-16-82; effective thirtieth day thereafter (Register 82, No. 16).
2. Change without regulatory effect repealing Section 1300.824 pursuant to Section 100, Title 1, California Code of Regulations filed 1-22-90 (Register 90, No. 11).
§1300.824.1. Notices and Requests for Approval of Certain Transactions.
Note • History
NOTE
Authority cited: Section 10824, Corporations Code. Reference: Section 10824, Corporations Code.
HISTORY
1. Change without regulatory effect repealing Section 1300.824.1 pursuant to Section 100, Title 1, California Code of Regulations filed 1-22-90 (register 90, No. 11).
§1300.826. Request for Ruling on Proposed Action or Article Amendment.
Note • History
NOTE
Authority cited: Section 10824, Corporations Code. Reference: Section 10826, Corporations Code.
HISTORY
1. Change without regulatory effect repealing Section 1300.826 pursuant to Section 100, Title 1, California Code of Regulations filed 1-22-90 (register 90, No. 11).